Restor Dent Endod.
2021 Nov;46(4):e59. 10.5395/rde.2021.46.e59.
Comparative analysis of bond strength to root dentin and compression of bioceramic cements used in regenerative endodontic procedures
- Affiliations
-
- 1Department of Endodontics, School of Dentistry, Federal University of Goiás, Goiânia, Goiás, Brazil
- 2Department of Endodontics, South American College, Goiânia, Goiás, Brazil
- KMID: 2548103
- DOI: http://doi.org/10.5395/rde.2021.46.e59
Abstract
Objectives
This study compared the Biodentine, MTA Repair HP, and Bio-C Repair bioceramics in terms of bond strength to dentin, failure mode, and compression.
Materials and Methods
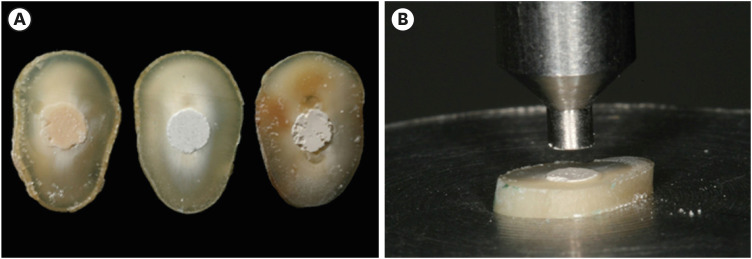
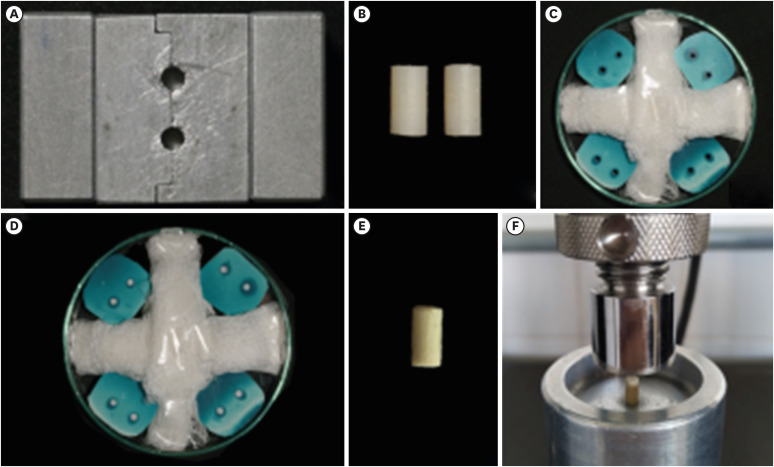
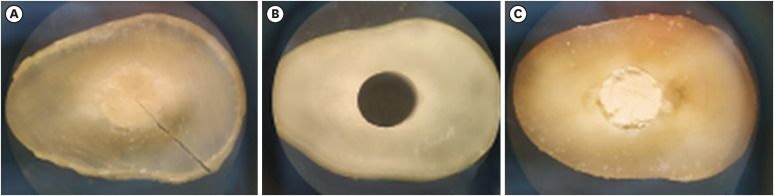
Fifty-four slices obtained from the cervical third of 18 single-rooted human mandibular premolars were randomly distributed (n = 18). After insertion of the bioceramic materials, the push-out test was performed. The failure mode was analyzed using stereomicroscopy. Another set of cylindrically-shaped bioceramic samples (n = 10) was prepared for compressive strength testing. The normality of data distribution was analyzed using the Shapiro-Wilk test. The Kruskal-Wallis and Friedman tests were used for the pushout test data, while compressive strength was analyzed with analysis of variance and the Tukey test, considering a significance level of 0.05.
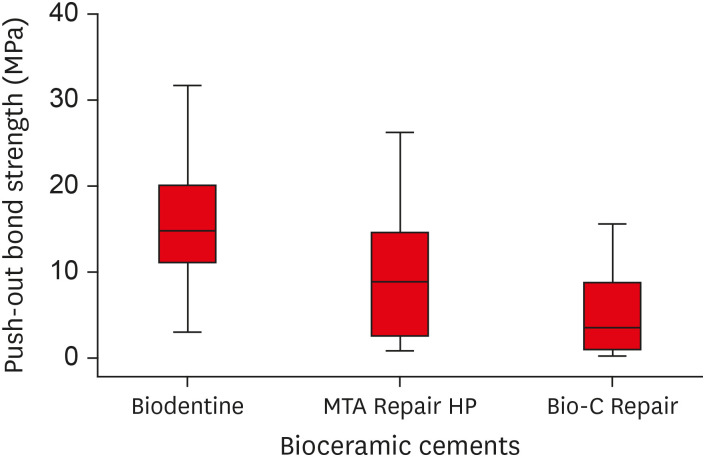
Results
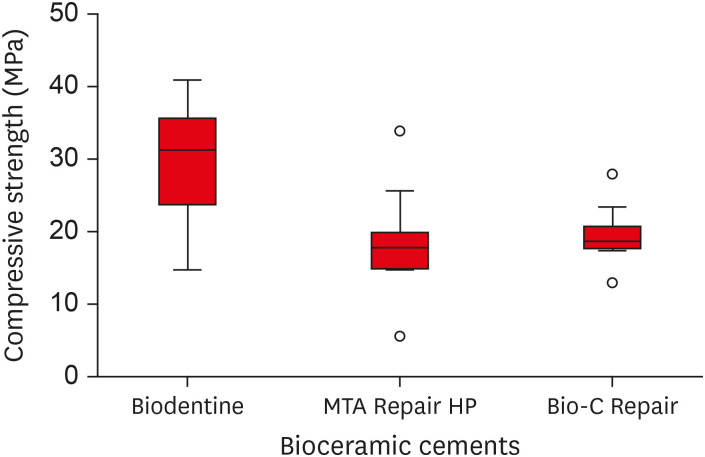
Biodentine presented a higher median bond strength value (14.79 MPa) than MTA Repair HP (8.84 MPa) and Bio-C Repair (3.48 MPa), with a significant difference only between Biodentine and Bio-C Repair. In the Biodentine group, the most frequent failure mode was mixed (61%), while in the MTA Repair HP and Bio-C Repair groups, it was adhesive (94% and 72%, respectively). Biodentine showed greater resistance to compression (29.59 ± 8.47 MPa) than MTA Repair HP (18.68 ± 7.40 MPa) and Bio-C Repair (19.96 ± 3.96 MPa) (p < 0.05).
Conclusions
Biodentine showed greater compressive strength than MTA Repair HP and Bio-C Repair, and greater bond strength than Bio-C Repair. The most frequent failure mode of Biodentine was mixed, while that of MTA Repair HP and Bio-C Repair was adhesive.
Keyword
Figure
Cited by 1 articles
-
Effects of different calcium-silicate based materials on fracture resistance of immature permanent teeth with replacement root resorption and osteoclastogenesis
Gabriela Leite de Souza, Gabrielle Alves Nunes Freitas, Maria Tereza Hordones Ribeiro, Nelly Xiomara Alvarado Lemus, Carlos José Soares, Camilla Christian Gomes Moura
Restor Dent Endod. 2023;48(2):e21. doi: 10.5395/rde.2023.48.e21.
Reference
-
1. Cvek M. Prognosis of luxated non-vital maxillary incisors treated with calcium hydroxide and filled with gutta-percha. A retrospective clinical study. Endod Dent Traumatol. 1992; 8:45–55. PMID: 1521505.
Article2. Nosrat A, Seifi A, Asgary S. Regenerative endodontic treatment (revascularization) for necrotic immature permanent molars: a review and report of two cases with a new biomaterial. J Endod. 2011; 37:562–567. PMID: 21419310.
Article3. Bansal R, Bansal R. Regenerative endodontics: a state of the art. Indian J Dent Res. 2011; 22:122–131. PMID: 21525690.4. Diogenes A, Ruparel NB. Regenerative endodontic procedures: clinical outcomes. Dent Clin North Am. 2017; 61:111–125. PMID: 27912813.5. Téclès O, Laurent P, Aubut V, About I. Human tooth culture: a study model for reparative dentinogenesis and direct pulp capping materials biocompatibility. J Biomed Mater Res B Appl Biomater. 2008; 85:180–187. PMID: 17853422.
Article6. Zhao X, He W, Song Z, Tong Z, Li S, Ni L. Mineral trioxide aggregate promotes odontoblastic differentiation via mitogen-activated protein kinase pathway in human dental pulp stem cells. Mol Biol Rep. 2012; 39:215–220. PMID: 21559841.
Article7. Zhu Q, Haglund R, Safavi KE, Spangberg LS. Adhesion of human osteoblasts on root-end filling materials. J Endod. 2000; 26:404–406. PMID: 11199765.8. Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review--Part I: chemical, physical, and antibacterial properties. J Endod. 2010; 36:16–27. PMID: 20003930.9. Neha K, Kansal R, Garg P, Joshi R, Garg D, Grover HS. Management of immature teeth by dentin-pulp regeneration: a recent approach. Med Oral Patol Oral Cir Bucal. 2011; 16:e997–ee1004. PMID: 21743418.10. Bortoluzzi EA, Araújo GS, Guerreiro Tanomaru JM, Tanomaru-Filho M. Marginal gingiva discoloration by gray MTA: a case report. J Endod. 2007; 33:325–327. PMID: 17320726.
Article11. Marconyak LJ Jr, Kirkpatrick TC, Roberts HW, Roberts MD, Aparicio A, Himel VT, Sabey KA. A comparison of coronal tooth discoloration elicited by various endodontic reparative materials. J Endod. 2016; 42:470–473. PMID: 26620853.
Article12. Lee YL, Lee BS, Lin FH, Yun Lin A, Lan WH, Lin CP. Effects of physiological environments on the hydration behavior of mineral trioxide aggregate. Biomaterials. 2004; 25:787–793. PMID: 14609667.
Article13. Han L, Okiji T. Bioactivity evaluation of three calcium silicate-based endodontic materials. Int Endod J. 2013; 46:808–814. PMID: 23402321.
Article14. Shokouhinejad N, Nekoofar MH, Iravani A, Kharrazifard MJ, Dummer PM. Effect of acidic environment on the push-out bond strength of mineral trioxide aggregate. J Endod. 2010; 36:871–874. PMID: 20416436.
Article15. Hashem AA, Wanees Amin SA. The effect of acidity on dislodgment resistance of mineral trioxide aggregate and bioaggregate in furcation perforations: an in vitro comparative study. J Endod. 2012; 38:245–249. PMID: 22244646.
Article16. Shahi S, Rahimi S, Yavari HR, Samiei M, Janani M, Bahari M, Abdolrahimi M, Pakdel F, Aghbali A. Effects of various mixing techniques on push-out bond strengths of white mineral trioxide aggregate. J Endod. 2012; 38:501–504. PMID: 22414837.
Article17. Kurtz JS, Perdigão J, Geraldeli S, Hodges JS, Bowles WR. Bond strengths of tooth-colored posts, effect of sealer, dentin adhesive, and root region. Am J Dent. 2003; 16:31A–36A.18. Fisher MA, Berzins DW, Bahcall JK. An in vitro comparison of bond strength of various obturation materials to root canal dentin using a push-out test design. J Endod. 2007; 33:856–858. PMID: 17804329.
Article19. Tagger M, Tagger E, Tjan AH, Bakland LK. Measurement of adhesion of endodontic sealers to dentin. J Endod. 2002; 28:351–354. PMID: 12026917.
Article20. Lucas CP, Viapiana R, Bosso-Martelo R, Guerreiro-Tanomaru JM, Camilleri J, Tanomaru-Filho M. Physicochemical properties and dentin bond strength of a tricalcium silicate-based retrograde material. Braz Dent J. 2017; 28:51–56. PMID: 28301018.
Article21. Abramson JH. WINPEPI updated: computer programs for epidemiologists, and their teaching potential. Epidemiol Perspect Innov. 2011; 8:1–9. PMID: 21288353.
Article22. Topçuoğlu HS, Arslan H, Akçay M, Saygili G, Çakici F, Topçuoğlu G. The effect of medicaments used in endodontic regeneration technique on the dislocation resistance of mineral trioxide aggregate to root canal dentin. J Endod. 2014; 40:2041–2044. PMID: 25282380.
Article23. Rosatto CM, Bicalho AA, Veríssimo C, Bragança GF, Rodrigues MP, Tantbirojn D, Versluis A, Soares CJ. Mechanical properties, shrinkage stress, cuspal strain and fracture resistance of molars restored with bulk-fill composites and incremental filling technique. J Dent. 2015; 43:1519–1528. PMID: 26449641.
Article24. Aguiar BA, Frota LM, Taguatinga DT, Vivan RR, Camilleri J, Duarte MA, de Vasconcelos BC. Influence of ultrasonic agitation on bond strength, marginal adaptation, and tooth discoloration provided by three coronary barrier endodontic materials. Clin Oral Investig. 2019; 23:4113–4122.
Article25. American Association of Endodontists. AAE Clinical Considerations for a Regenerative Procedure Revised 4/1/2018 [Internet]. updated 2020 Oct 20. Available from: https://www.aae.org/specialty/wp-content/uploads/sites/2/2018/06/ConsiderationsForRegEndo_AsOfApril2018.pdf.26. Iwaya SI, Ikawa M, Kubota M. Revascularization of an immature permanent tooth with apical periodontitis and sinus tract. Dent Traumatol. 2001; 17:185–187. PMID: 11585146.
Article27. Akcay M, Arslan H, Yasa B, Kavrık F, Yasa E. Spectrophotometric analysis of crown discoloration induced by various antibiotic pastes used in revascularization. J Endod. 2014; 40:845–848. PMID: 24862714.
Article28. Tagelsir A, Yassen GH, Gomez GF, Gregory RL. Effect of antimicrobials used in regenerative endodontic procedures on 3-week-old Enterococcus faecalis biofilm. J Endod. 2016; 42:258–262. PMID: 26577870.
Article29. Arnold WH, Konopka S, Gaengler P. Qualitative and quantitative assessment of intratubular dentin formation in human natural carious lesions. Calcif Tissue Int. 2001; 69:268–273. PMID: 11768196.
Article30. Lo Giudice G, Cutroneo G, Centofanti A, Artemisia A, Bramanti E, Militi A, Rizzo G, Favaloro A, Irrera A, Lo Giudice R, Cicciù M. Dentin morphology of root canal surface: a quantitative evaluation based on a scanning electronic microscopy study. BioMed Res Int. 2015; 2015:164065. PMID: 26413504.
Article31. Brichko J, Burrow MF, Parashos P. Design variability of the push-out bond test in endodontic research: a systematic review. J Endod. 2018; 44:1237–1245. PMID: 29935874.
Article32. Zanatta RF, Barreto BC, Xavier TA, Versluis A, Soares CJ. Effect of punch and orifice base sizes in different push-out test setups: stress distribution analysis. J Adhes Dent. 2015; 17:45–50. PMID: 25625138.33. Nagas E, Cehreli ZC, Uyanik MO, Vallittu PK, Lassila LV. Effect of several intracanal medicaments on the push-out bond strength of ProRoot MTA and Biodentine. Int Endod J. 2016; 49:184–188. PMID: 25631153.
Article34. Turk T, Fidler A. Effect of medicaments used in endodontic regeneration technique on push-out bond strength of MTA and Biodentine. Biotechnol Biotechnol Equip. 2016; 30:140–144.
Article35. Majeed A, AlShwaimi E. Push-out bond strength and surface microhardness of calcium silicate-based biomaterials: an in vitro study. Med Princ Pract. 2017; 26:139–145. PMID: 27852076.
Article36. Silva EJ, Carvalho NK, Zanon M, Senna PM, DE-Deus G, Zuolo ML, Zaia AA. Push-out bond strength of MTA HP, a new high-plasticity calcium silicate-based cement. Braz Oral Res. 2016; 30:1–5.
Article37. Ørstavik D. Physical properties of root canal sealers: measurement of flow, working time, and compressive strength. Int Endod J. 1983; 16:99–107. PMID: 6583168.
Article38. Çelik D, Er K, Serper A, Taşdemir T, Ceyhanlı KT. Push-out bond strength of three calcium silicate cements to root canal dentine after two different irrigation regimes. Clin Oral Investig. 2014; 18:1141–1146.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The effect of repeated bonding on the shear bond strength of different resin cements to enamel and dentin
- The effect of bonding resin on bond strength of dual-cure resin cements
- Push-out bond strength of a self-adhesive resin cement used as endodontic sealer
- Effect of dentin surface wetness on tensile bond strength of self adhesive resin cements
- Comparative evaluation of micro-shear bond strength between two different luting methods of resin cement to dentin