J Korean Med Sci.
2023 Nov;38(44):e371. 10.3346/jkms.2023.38.e371.
Effective Vaccination and Education Strategies for Emerging Infectious Diseases Such as COVID-19
- Affiliations
-
- 1Division of Infectious Diseases, Department of Internal Medicine, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea
- 2Department of Preventive Medicine, Gachon University College of Medicine, Incheon, Korea
- 3Division of Infectious Diseases, Department of Internal Medicine, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea
- KMID: 2547975
- DOI: http://doi.org/10.3346/jkms.2023.38.e371
Abstract
- Social isolation and control owing to coronavirus disease 2019 (COVID-19) are easing; however, concerns regarding new infectious diseases have not disappeared. Given epidemic experiences such as severe acute respiratory syndrome (SARS), the influenza pandemic, Middle East respiratory syndrome (MERS), and COVID-19, it is necessary to prepare for the outbreak of new infectious diseases and situations in which large-scale vaccinations are required. Although the development of vaccines against COVID-19 has contributed greatly to overcoming the pandemic, concerning vaccine side effects from the general public, including medical personnel, and decreased confidence in vaccine efficacy and side effects, present many challenges in promoting and educating vaccinations for new infectious diseases in the future. In addition to plans to develop vaccines for the outbreak of new infectious diseases, education and promotion plans are necessary to administer the latest developments of vaccines to the general public. Moreover, efforts are needed to secure the necessity, legitimacy, and evidence for rapid vaccination on a large scale at the national level. It is also necessary to carefully prepare scientific bases and explanatory statements so that the general public can easily understand them. This study aimed to establish vaccine strategies and vaccination education plans for new infectious diseases that may occur in the future. Many ways to promote vaccination to the general public and healthcare workers should be prepared to ensure that the latest vaccines against new infectious diseases are administered safely. Thus, education and promotion of vaccine efficacy and safety based on specific data from clinical studies are necessary.
Figure
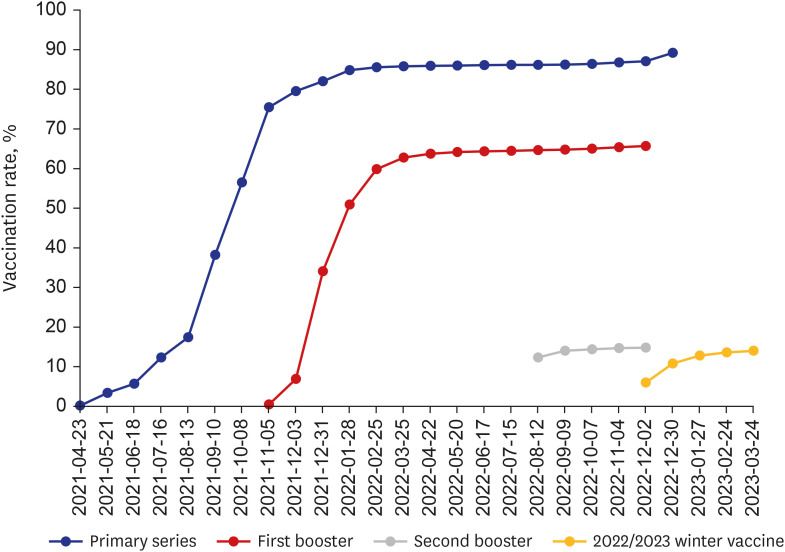
Reference
-
1. Wouters OJ, Shadlen KC, Salcher-Konrad M, Pollard AJ, Larson HJ, Teerawattananon Y, et al. Challenges in ensuring global access to COVID-19 vaccines: production, affordability, allocation, and deployment. Lancet. 2021; 397(10278):1023–1034. PMID: 33587887.
Article2. Romer D, Winneg KM, Jamieson PE, Brensinger C, Jamieson KH. Misinformation about vaccine safety and uptake of COVID-19 vaccines among adults and 5-11-year-olds in the United States. Vaccine. 2022; 40(45):6463–6470. PMID: 36192273.
Article3. Song I, Lee SH. COVID-19 vaccine refusal associated with health literacy: findings from a population-based survey in Korea. BMC Public Health. 2023; 23(1):255. PMID: 36747179.
Article4. de Figueiredo A, Simas C, Larson HJ. COVID-19 vaccine acceptance and its socio-demographic and emotional determinants: a multi-country cross-sectional study. Vaccine. 2023; 41(2):354–364. PMID: 36414475.
Article5. Watson OJ, Barnsley G, Toor J, Hogan AB, Winskill P, Ghani AC. Global impact of the first year of COVID-19 vaccination: a mathematical modelling study. Lancet Infect Dis. 2022; 22(9):1293–1302. PMID: 35753318.
Article6. Lip A, Pateman M, Fullerton MM, Chen HM, Bailey L, Houle S, et al. Vaccine hesitancy educational tools for healthcare providers and trainees: a scoping review. Vaccine. 2023; 41(1):23–35. PMID: 36437208.
Article7. Whitehead HS, French CE, Caldwell DM, Letley L, Mounier-Jack S. A systematic review of communication interventions for countering vaccine misinformation. Vaccine. 2023; 41(5):1018–1034. PMID: 36628653.
Article8. Gesser-Edelsburg A, Diamant A, Hijazi R, Mesch GS. Correcting misinformation by health organizations during measles outbreaks: a controlled experiment. PLoS One. 2018; 13(12):e0209505. PMID: 30566485.
Article9. Jeon M, Kim J, Oh CE, Lee JY. Adverse events following immunization associated with coronavirus disease 2019 vaccination reported in the mobile vaccine adverse events reporting system. J Korean Med Sci. 2021; 36(17):e114. PMID: 33942578.
Article10. Excler JL, Saville M, Berkley S, Kim JH. Vaccine development for emerging infectious diseases. Nat Med. 2021; 27(4):591–600. PMID: 33846611.
Article11. Zhang Z, Shen Q, Chang H. Vaccines for COVID-19: a systemic review of immunogenicity, current development, and future prospects. Front Immunol. 2022; 13:843928. PMID: 35572592.
Article12. Ford A, Hwang A, Mo AX, Baqar S, Touchette N, Deal C, et al. Meeting summary: global vaccine and immunization research forum, 2021. Vaccine. 2023; 41(11):1799–1807. PMID: 36803897.
Article13. Nham E, Song JY, Noh JY, Cheong HJ, Kim WJ. COVID-19 vaccination in Korea: past, present, and the way forward. J Korean Med Sci. 2022; 37(47):e351. PMID: 36472087.
Article14. Jamieson KH, Romer D, Jamieson PE, Winneg KM, Pasek J. The role of non-COVID-specific and COVID-specific factors in predicting a shift in willingness to vaccinate: a panel study. Proc Natl Acad Sci U S A. 2021; 118(52):e2112266118. PMID: 34930844.
Article15. Jung J. Preparing for the coronavirus disease (COVID-19) vaccination: evidence, plans, and implications. J Korean Med Sci. 2021; 36(7):e59. PMID: 33619920.
Article16. Thompson KM, Gellin BG, Hinman AR, Orenstein WA. The national vaccine advisory committee at 30: Impact and opportunity. Vaccine. 2018; 36(11):1330–1344. PMID: 29422369.
Article17. Choi YY, Kim MK, Kwon HC, Kim GH. Safety monitoring after the BNT162b2 COVID-19 vaccine among adults aged 75 years or older. J Korean Med Sci. 2021; 36(45):e318. PMID: 34811980.
Article18. García-Grimshaw M, Ceballos-Liceaga SE, Hernández-Vanegas LE, Núñez I, Hernández-Valdivia N, Carrillo-García DA, et al. Neurologic adverse events among 704,003 first-dose recipients of the BNT162b2 mRNA COVID-19 vaccine in Mexico: a nationwide descriptive study. Clin Immunol. 2021; 229:108786. PMID: 34147649.
Article19. SeyedAlinaghi S, Karimi A, Pashaei Z, Afzalian A, Mirzapour P, Ghorbanzadeh K, et al. Safety and adverse events related to COVID-19 mRNA vaccines; a systemic review. Arch Acad Emerg Med. 2022; 10(1):e41. PMID: 35765616.20. Patone M, Mei XW, Handunnetthi L, Dixon S, Zaccardi F, Shankar-Hari M, et al. Risk of myocarditis after sequential doses of COVID-19 vaccine and SARS-CoV-2 infection by age and sex. Circulation. 2022; 146(10):743–754. PMID: 35993236.
Article21. Link-Gelles R, Weber ZA, Reese SE, Payne AB, Gaglani M, Adams K, et al. Estimates of bivalent mRNA vaccine durability in preventing COVID-19-Associated hospitalization and critical illness among adults with and without immunocompromising conditions — VISION Network, September 2022–April 2023. MMWR Morb Mortal Wkly Rep. 2023; 72(21):579–588. PMID: 37227984.
Article22. Tenforde MW, Weber ZA, Natarajan K, Klein NP, Kharbanda AB, Stenehjem E, et al. Early estimates of bivalent mRNA vaccine effectiveness in preventing COVID-19-associated emergency department or urgent care encounters and hospitalizations among immunocompetent adults—VISION Network, Nine States, September–November 2022. MMWR Morb Mortal Wkly Rep. 2023; 71(53):1637–1646. PMID: 36921274.23. Nham E, Kim YE, Jung J, Kim DW, Jang H, Hyun H, et al. COVID-19 vaccination rates in patients with chronic medical conditions: a nationwide cross-sectional study. J Korean Med Sci. 2022; 37(45):e325. PMID: 36413798.
Article24. Shin A, Kim DW, Kim YE, Kim DR, Jung J, Kim YJ. COVID-19 vaccination status among Korean pediatric population with comorbidities. J Korean Med Sci. 2023; 38(32):e248. PMID: 37582498.
Article25. Hwang SE, Kim WH, Heo J. Socio-demographic, psychological, and experiential predictors of COVID-19 vaccine hesitancy in South Korea, October-December 2020. Hum Vaccin Immunother. 2022; 18(1):1–8.
Article26. Lee M, You M. Direct and indirect associations of media use with COVID-19 vaccine hesitancy in South Korea: cross-sectional web-based survey. J Med Internet Res. 2022; 24(1):e32329. PMID: 34870605.
Article27. Pires C. Global predictors of COVID-19 vaccine hesitancy: a systemic review. Vaccines (Basel). 2022; 10(8):1349. PMID: 36016237.28. Kweon SS, Yun I, Choi C, Ryu SY, Cho JH, Shin MH. Factors associated with COVID-19 vaccine hesitancy in Korea. Chonnam Med J. 2022; 58(1):43–47. PMID: 35169559.
Article29. Paterson P, Meurice F, Stanberry LR, Glismann S, Rosenthal SL, Larson HJ. Vaccine hesitancy and healthcare providers. Vaccine. 2016; 34(52):6700–6706. PMID: 27810314.
Article30. Nguyen KH, Srivastav A, Razzaghi H, Williams W, Lindley MC, Jorgensen C, et al. COVID-19 vaccination intent, perceptions, and reasons for not vaccinating among groups prioritized for early vaccination - United States, September and December 2020. Am J Transplant. 2021; 21(4):1650–1656. PMID: 33788992.
Article31. MacDonald NE. SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015; 33(34):4161–4164. PMID: 25896383.
Article32. Kim JS. Association of COVID-19 vaccine attitudes and cognitions of COVID-19-related stigma with vaccine hesitancy among college students. J Korean Acad Soc Nurs Educ. 2022; 28(3):296–304.
Article33. Choi SH, Jo YH, Jo KJ, Park SE. Pediatric and parents’ attitudes towards COVID-19 vaccines and intention to vaccinate for children. J Korean Med Sci. 2021; 36(31):e227. PMID: 34402237.
Article34. Noh Y, Kim JH, Yoon D, Choe YJ, Choe SA, Jung J, et al. Predictors of COVID-19 booster vaccine hesitancy among fully vaccinated adults in Korea: a nationwide cross-sectional survey. Epidemiol Health. 2022; 44:e2022061. PMID: 35914771.
Article35. Choe YH, Cha J. Factors influencing clinical nurse’s intention for acquiring coronavirus disease 2019 vaccination. J Health Info Stat. 2022; 47(1):48–56.
Article36. Bae S, Kim HJ. Influencing factors of COVID-19 vaccination intention among college students: based on Andersen’s model. J Korean Public Health Nurs. 2021; 35(3):384–400.37. Choi BY, Yoon H, Seong WJ, Cho GJ, Na S, Jung YM, et al. Knowledge and acceptability of the COVID-19 vaccine among obstetricians and gynecologists in Korea, and factors affecting its recommendation in the pregnant population. J Korean Soc Matern Child Health. 2022; 26(4):245–253.
Article38. Peterson CJ, Lee B, Nugent K. COVID-19 vaccination hesitancy among healthcare workers—a review. Vaccines (Basel). 2022; 10(6):948. PMID: 35746556.
Article39. Janssen C, Maillard A, Bodelet C, Claudel AL, Gaillat J, Delory T, et al. Hesitancy towards COVID-19 vaccination among healthcare workers: a multi-centric survey in France. Vaccines (Basel). 2021; 9(6):547. PMID: 34067490.
Article40. Toth-Manikowski SM, Swirsky ES, Gandhi R, Piscitello G. COVID-19 vaccination hesitancy among health care workers, communication, and policy-making. Am J Infect Control. 2022; 50(1):20–25. PMID: 34653527.
Article41. Choi IS, Kim EA. Factors influencing the COVID-19 vaccination intentions in parents for their children aged 5~11: Korea, April 2022. J Korean Acad Nurs. 2023; 53(2):208–221. PMID: 37164348.
Article42. Tan LJ, Koh CP, Lai SK, Poh WC, Othman MS, Hussin H. A systemic review and recommendation for an autopsy approach to death followed the COVID 19 vaccination. Forensic Sci Int. 2022; 340:111469. PMID: 36162300.
Article43. Yoon D, Jeon HL, Noh Y, Choe YJ, Choe SA, Jung J, et al. A nationwide survey of mRNA COVID-19 vaccinee’s experiences on adverse events and its associated factors. J Korean Med Sci. 2023; 38(22):e170. PMID: 37272559.
Article44. Lu X, Masuda S, Horlad H, Katoh T. Safety and adverse effects of the coronavirus disease 2019 vaccine among the general Japanese adult population. Vaccine. 2023; 41(35):5090–5096. PMID: 37455163.
Article45. Kahn AL, Steffen CA, Henaff L, MacDonald NE, Morgan C, Faden R, et al. COVID-19 vaccine policy development in a sample of 44 countries - key findings from a December 2021 survey of National Immunization Technical Advisory Groups (NITAGs). Vaccine. 2023; 41(3):676–683. PMID: 36494252.
Article46. MacDonald NE, Dube E, Comeau JL. Have vaccine hesitancy models oversimplified a complex problem to our detriment? The Adapted Royal Society of Canada vaccine uptake framework. Vaccine. 2022; 40(29):3927–3930. PMID: 35637069.
Article47. Canning AG, Watson KE, McCreedy KE, Olawepo JO. Ethics and effectiveness of US COVID-19 vaccine mandates and vaccination passports: a review. J Res Health Sci. 2022; 22(2):e00546. PMID: 36511258.
Article48. Bardosh K, de Figueiredo A, Gur-Arie R, Jamrozik E, Doidge J, Lemmens T, et al. The unintended consequences of COVID-19 vaccine policy: why mandates, passports and restrictions may cause more harm than good. BMJ Glob Health. 2022; 7(5):e008684.
Article49. Fishman J, Mandell DS, Salmon MK, Candon M. Large and small financial incentives may motivate COVID-19 vaccination: a randomized, controlled survey experiment. PLoS One. 2023; 18(3):e0282518. PMID: 36930588.
Article50. Skafle I, Nordahl-Hansen A, Quintana DS, Wynn R, Gabarron E. Misinformation about COVID-19 vaccines on social media: rapid review. J Med Internet Res. 2022; 24(8):e37367. PMID: 35816685.
Article51. Mohamed K, Rzymski P, Islam MS, Makuku R, Mushtaq A, Khan A, et al. COVID-19 vaccinations: the unknowns, challenges, and hopes. J Med Virol. 2022; 94(4):1336–1349. PMID: 34845731.
Article52. Colosi E, Bassignana G, Contreras DA, Poirier C, Boëlle PY, Cauchemez S, et al. Screening and vaccination against COVID-19 to minimise school closure: a modelling study. Lancet Infect Dis. 2022; 22(7):977–989. PMID: 35378075.
Article53. Fontanet A, Cauchemez S. COVID-19 herd immunity: where are we? Nat Rev Immunol. 2020; 20(10):583–584. PMID: 32908300.
Article54. McDermott A. Core concept: Herd immunity is an important-and often misunderstood-public health phenomenon. Proc Natl Acad Sci U S A. 2021; 118(21):e2107692118. PMID: 34011611.
Article55. Wang CW, de Jong EP, Faure JA, Ellington JL, Chen CS, Chan CC. A matter of trust: a qualitative comparison of the determinants of COVID-19 vaccine hesitancy in Taiwan, the United States, the Netherlands, and Haiti. Hum Vaccin Immunother. 2022; 18(5):2050121. PMID: 35349382.
Article56. Geisen UM, Berner DK, Tran F, Sümbül M, Vullriede L, Ciripoi M, et al. Immunogenicity and safety of anti-SARS-CoV-2 mRNA vaccines in patients with chronic inflammatory conditions and immunosuppressive therapy in a monocentric cohort. Ann Rheum Dis. 2021; 80(10):1306–1311. PMID: 33762264.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Suggestions for Advancing the Control of Emerging Infectious Diseases
- Factors Influencing the COVID-19 Vaccination Intentions in Nurses: Korea, February 2021
- The relationship between nursing professionalism and nursing intention for patients with emerging infectious diseases of nursing students who had experienced COVID-19 pandemic: the mediating effect of e-Health literacy
- COVID-19 Vaccination and Herd Immunity
- Post COVID-19 Emerging Infectious Diseases: What is the Next Pandemic Agent?