J Korean Med Sci.
2023 Nov;38(44):e345. 10.3346/jkms.2023.38.e345.
Real-World Treatment Patterns and Clinical Outcomes in Korean Patients With AML Ineligible for First-Line Intensive Chemotherapy: A Subanalysis of the CURRENT Study, a Non-Interventional, Retrospective Chart Review
- Affiliations
-
- 1Division of Hematology and Medical Oncology, Department of Internal Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- 2Division of Hematology and Oncology, Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea
- 3Division of Hematology and Oncology, Department of Internal Medicine, Chungnam National University School of Medicine, Daejeon, Korea
- 4Evidence Solutions, AbbVie Inc., North Chicago, IL, USA
- 5Medical Affairs, AbbVie Korea Ltd., Seoul, Korea
- 6Department of Hematology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2547968
- DOI: http://doi.org/10.3346/jkms.2023.38.e345
Abstract
- Background
Although most elderly patients with acute myeloid leukemia (AML) are ineligible for intensive chemotherapy (ICT), treatment options remain limited. CURRENT (UMIN000037786), a real-world, non-interventional, retrospective chart review, evaluated clinical outcomes, clinicopathologic characteristics, and treatment patterns in these patients. We present results from a subanalysis of Korean patients in this study.
Methods
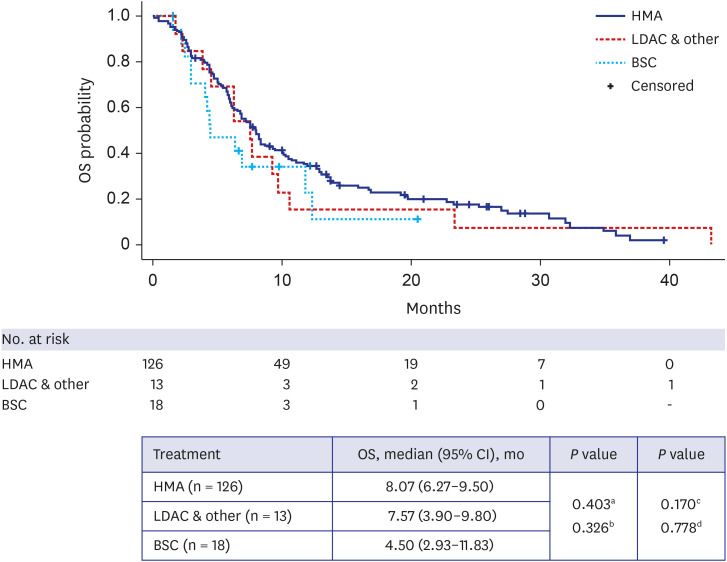
Patients were aged ≥ 18 years with primary or secondary AML ineligible for ICT who initiated first-line systemic therapy or best supportive care (BSC) between 2015 and 2018 across four centers in Korea. Primary endpoint was overall survival (OS) from diagnosis. Secondary endpoints included progression-free survival (PFS), time to treatment failure, and response rates. Data analyses were primarily descriptive, with time-to-event outcomes estimated using the Kaplan-Meier method, and Cox regression used to determine prognostic factors for survival.
Results
Among 194 patients enrolled, 84.0% received systemic therapy and 16.0% received BSC. Median age at diagnosis was 74 and 78 years, and Eastern Cooperative Oncology Group (ECOG) performance status 0 or 1 was reported in 73.0% and 48.4% of patients, respectively; poor cytogenetic risk was reported in 30.1% and 16.1% of patients. Median OS was 7.83 vs. 4.50 months, and median PFS was 6.73 vs. 4.50 months in the systemic therapy vs. BSC groups. Prognostic factors affecting OS included secondary AML (hazard ratio, 1.67 [95% confidence interval, 1.13–2.45]), ECOG performance status ≥ 2 (2.41 [1.51–3.83]), poor cytogenetic risk (2.10 [1.36–3.24]), and Charlson comorbidity index ≥ 1 (2.26 [1.43–3.58]).
Conclusion
Clinical outcomes are poor in Korean patients with AML ineligible for ICT who are prescribed current systemic therapies or BSC. There is a substantial unmet need for novel agents (monotherapy or in combination) to improve clinical outcomes in this patient population.
Figure
Reference
-
1. Saultz JN, Garzon R. Acute myeloid leukemia: a concise review. J Clin Med. 2016; 5(3):33. PMID: 26959069.
Article2. Pollyea DA, Bixby D, Perl A, Bhatt VR, Altman JK, Appelbaum FR, et al. NCCN guidelines insights: acute myeloid leukemia, version 2. 2021. J Natl Compr Canc Netw. 2021; 19(1):16–27. PMID: 33406488.3. National Cancer Institute. Cancer stat facts: leukemia — acute myeloid leukemia. Updated 2021. Accessed September 12, 2023. https://seer.cancer.gov/statfacts/html/amyl.html .4. Yi M, Li A, Zhou L, Chu Q, Song Y, Wu K. The global burden and attributable risk factor analysis of acute myeloid leukemia in 195 countries and territories from 1990 to 2017: estimates based on the global burden of disease study 2017. J Hematol Oncol. 2020; 13(1):72. PMID: 32513227.
Article5. Park EH, Lee H, Won YJ, Ju HY, Oh CM, Ingabire C, et al. Nationwide statistical analysis of myeloid malignancies in Korea: incidence and survival rate from 1999 to 2012. Blood Res. 2015; 50(4):204–217. PMID: 26770948.
Article6. Thein MS, Ershler WB, Jemal A, Yates JW, Baer MR. Outcome of older patients with acute myeloid leukemia: an analysis of SEER data over 3 decades. Cancer. 2013; 119(15):2720–2727. PMID: 23633441.
Article7. Deschler B, de Witte T, Mertelsmann R, Lübbert M. Treatment decision-making for older patients with high-risk myelodysplastic syndrome or acute myeloid leukemia: problems and approaches. Haematologica. 2006; 91(11):1513–1522. PMID: 17082009.8. Ferrara F, Barosi G, Venditti A, Angelucci E, Gobbi M, Pane F, et al. Consensus-based definition of unfitness to intensive and non-intensive chemotherapy in acute myeloid leukemia: a project of SIE, SIES and GITMO group on a new tool for therapy decision making. Leukemia. 2013; 27(5):997–999. PMID: 23653072.
Article9. Döhner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Büchner T, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017; 129(4):424–447. PMID: 27895058.
Article10. Heuser M, Ofran Y, Boissel N, Brunet Mauri S, Craddock C, Janssen J, et al. Acute myeloid leukaemia in adult patients: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2020; 31(6):697–712. PMID: 32171751.
Article11. Ha H, Jeong Y, Lim JH, Suh YJ. Treatment pattern, financial burden, and outcomes in elderly patients with acute myeloid leukemia in Korea: a nationwide cohort study. Int J Environ Res Public Health. 2022; 19(4):2317. PMID: 35206499.
Article12. Palmieri R, Paterno G, De Bellis E, Mercante L, Buzzatti E, Esposito F, et al. Therapeutic choice in older patients with acute myeloid leukemia: a matter of fitness. Cancers (Basel). 2020; 12(1):120. PMID: 31906489.
Article13. Büchner T, Berdel WE, Haferlach C, Haferlach T, Schnittger S, Müller-Tidow C, et al. Age-related risk profile and chemotherapy dose response in acute myeloid leukemia: a study by the German Acute Myeloid Leukemia Cooperative Group. J Clin Oncol. 2009; 27(1):61–69. PMID: 19047294.
Article14. Wahlin A, Markevärn B, Golovleva I, Nilsson M. Prognostic significance of risk group stratification in elderly patients with acute myeloid leukaemia. Br J Haematol. 2001; 115(1):25–33. PMID: 11722406.
Article15. Wheatley K, Brookes CL, Howman AJ, Goldstone AH, Milligan DW, Prentice AG, et al. Prognostic factor analysis of the survival of elderly patients with AML in the MRC AML11 and LRF AML14 trials. Br J Haematol. 2009; 145(5):598–605. PMID: 19344426.
Article16. Krok-Schoen JL, Fisher JL, Stephens JA, Mims A, Ayyappan S, Woyach JA, et al. Incidence and survival of hematological cancers among adults ages ≥75 years. Cancer Med. 2018; 7(7):3425–3433. PMID: 29654631.17. Miyamoto T, Sanford D, Tomuleasa C, Hsiao HH, Olivera LJ, Enjeti AK, et al. Real-world treatment patterns and clinical outcomes in patients with AML unfit for first-line intensive chemotherapy. Leuk Lymphoma. 2022; 63(4):928–938. PMID: 35147482.
Article18. Dombret H, Seymour JF, Butrym A, Wierzbowska A, Selleslag D, Jang JH, et al. International phase 3 study of azacitidine vs conventional care regimens in older patients with newly diagnosed AML with >30% blasts. Blood. 2015; 126(3):291–299. PMID: 25987659.
Article19. Seymour JF, Döhner H, Butrym A, Wierzbowska A, Selleslag D, Jang JH, et al. Azacitidine improves clinical outcomes in older patients with acute myeloid leukaemia with myelodysplasia-related changes compared with conventional care regimens. BMC Cancer. 2017; 17(1):852. PMID: 29241450.
Article20. Kantarjian HM, Thomas XG, Dmoszynska A, Wierzbowska A, Mazur G, Mayer J, et al. Multicenter, randomized, open-label, phase III trial of decitabine versus patient choice, with physician advice, of either supportive care or low-dose cytarabine for the treatment of older patients with newly diagnosed acute myeloid leukemia. J Clin Oncol. 2012; 30(21):2670–2677. PMID: 22689805.
Article21. Medeiros BC, Satram-Hoang S, Hurst D, Hoang KQ, Momin F, Reyes C. Big data analysis of treatment patterns and outcomes among elderly acute myeloid leukemia patients in the United States. Ann Hematol. 2015; 94(7):1127–1138. PMID: 25791241.
Article22. He PF, Zhou JD, Yao DM, Ma JC, Wen XM, Zhang ZH, et al. Efficacy and safety of decitabine in treatment of elderly patients with acute myeloid leukemia: a systematic review and meta-analysis. Oncotarget. 2017; 8(25):41498–41507. PMID: 28489568.
Article23. Bell JA, Galaznik A, Farrelly E, Blazer M, Murty S, Ogbonnaya A, et al. A retrospective study evaluating treatment patterns and survival outcomes in elderly patients with acute myeloid leukemia treated in the United States with either 7+3 or a hypomethylating agent. Leuk Res. 2019; 78:45–51. PMID: 30716655.
Article24. Organisation for Economic Co-operation and Development (OECD). OECD health care quality review: Korea assessment and recommendations. Updated 2012. Accessed May 23, 2023. https://www.oecd.org/korea/49818570.pdf .25. Papageorgiou SG, Kotsianidis I, Bouchla A, Symeonidis A, Galanopoulos A, Viniou NA, et al. Serum ferritin and ECOG performance status predict the response and improve the prognostic value of IPSS or IPSS-R in patients with high-risk myelodysplastic syndromes and oligoblastic acute myeloid leukemia treated with 5-azacytidine: a retrospective analysis of the Hellenic national registry of myelodysplastic and hypoplastic syndromes. Ther Adv Hematol. 2020; 11:2040620720966121. PMID: 33343854.
Article26. Dhakal P, Shostrom V, Al-Kadhimi ZS, Maness LJ, Gundabolu K, Bhatt VR. Usefulness of Charlson comorbidity index to predict early mortality and overall survival in older patients with acute myeloid leukemia. Clin Lymphoma Myeloma Leuk. 2020; 20(12):804–812.e8. PMID: 32739312.
Article27. Gbadamosi B, Ezekwudo D, Bastola S, Jaiyesimi I. Predictive and prognostic markers in adults with acute myeloid leukemia: a single-institution experience. Clin Lymphoma Myeloma Leuk. 2018; 18(7):e287–e294. PMID: 29803615.
Article28. Papaemmanuil E, Gerstung M, Bullinger L, Gaidzik VI, Paschka P, Roberts ND, et al. Genomic classification and prognosis in acute myeloid leukemia. N Engl J Med. 2016; 374(23):2209–2221. PMID: 27276561.
Article29. Ahn JS, Kim HJ. FLT3 mutations in acute myeloid leukemia: a review focusing on clinically applicable drugs. Blood Res. 2022; 57:32–36. PMID: 35483923.30. Jung J, Cho BS, Kim HJ, Han E, Jang W, Han K, et al. Reclassification of acute myeloid leukemia according to the 2016 WHO classification. Ann Lab Med. 2019; 39(3):311–316. PMID: 30623623.
Article31. de Leeuw DC, Ossenkoppele GJ, Janssen JJ. Older patients with acute myeloid leukemia deserve individualized treatment. Curr Oncol Rep. 2022; 24(11):1387–1400. PMID: 35653050.
Article32. DiNardo CD, Jonas BA, Pullarkat V, Thirman MJ, Garcia JS, Wei AH, et al. Azacitidine and venetoclax in previously untreated acute myeloid leukemia. N Engl J Med. 2020; 383(7):617–629. PMID: 32786187.
Article33. Chen Y, Yang T, Zheng X, Yang X, Zheng Z, Zheng J, et al. The outcome and prognostic factors of 248 elderly patients with acute myeloid leukemia treated with standard-dose or low-intensity induction therapy. Medicine (Baltimore). 2016; 95(30):e4182. PMID: 27472687.
Article34. Lübbert M, Rüter BH, Claus R, Schmoor C, Schmid M, Germing U, et al. A multicenter phase II trial of decitabine as first-line treatment for older patients with acute myeloid leukemia judged unfit for induction chemotherapy. Haematologica. 2012; 97(3):393–401. PMID: 22058219.
Article35. Kim S, Yoon SS, Hong J, Shin DY, Koh Y, Byun JM, et al. Characterization and prognosis of secondary acute myeloid leukemia in an Asian population: AML with antecedent hematological disease confers worst outcomes, irrespective of cytogenetic risk. Anticancer Res. 2020; 40(5):2917–2924. PMID: 32366443.
Article36. Yi HG, Lee MH, Kim CS, Hong J, Park J, Lee JH, et al. Clinical characteristics and treatment outcome of acute myeloid leukemia in elderly patients in Korea: a retrospective analysis. Blood Res. 2014; 49(2):95–99. PMID: 25025010.
Article37. Lee KH, Lee JS, Suh CW, Kim SW, Kim SB, Lee JH, et al. Prognostic factors of acute myelocytic leukemia: an analysis of 132 patients in a single institution. J Korean Med Sci. 1996; 11(3):222–232. PMID: 8843004.
Article38. Wang RQ, Chen CJ, Jing Y, Qin JY, Li Y, Chen GF, et al. Characteristics and prognostic significance of genetic mutations in acute myeloid leukemia based on a targeted next-generation sequencing technique. Cancer Med. 2020; 9(22):8457–8467. PMID: 32970934.
Article39. Roboz GJ, Wei AH, Ravandi F, Pocock C, Montesinos P, Dombret H, et al. Prognostic factors of overall (OS) and relapse-free survival (RFS) for patients with acute myeloid leukemia (AML) in remission after intensive chemotherapy (IC): multivariate analyses from the QUAZAR AML-001 trial of oral azacitidine (Oral-AZA). J Clin Oncol. 2021; 39(15):Suppl. 7014.
Article40. Kim DS, Kang KW, Yu ES, Kim HJ, Kim JS, Lee SR, et al. Selection of elderly acute myeloid leukemia patients for intensive chemotherapy: effectiveness of intensive chemotherapy and subgroup analysis. Acta Haematol. 2015; 133(3):300–309. PMID: 25470986.
Article41. Ma TT, Lin XJ, Cheng WY, Xue Q, Wang SY, Liu FJ, et al. Development and validation of a prognostic model for adult patients with acute myeloid leukaemia. EBioMedicine. 2020; 62:103126. PMID: 33232873.
Article42. Suvajdžić N, Cvetković Z, Dorđević V, Kraguljac-Kurtović N, Stanisavljević D, Bogdanović A, et al. Prognostic factors for therapy-related acute myeloid leukaemia (t-AML)--a single centre experience. Biomed Pharmacother. 2012; 66(4):285–292. PMID: 22401928.
Article43. Oh SB, Park SW, Chung JS, Lee WS, Lee HS, Cho SH, et al. Therapeutic decision-making in elderly patients with acute myeloid leukemia: conventional intensive chemotherapy versus hypomethylating agent therapy. Ann Hematol. 2017; 96(11):1801–1809. PMID: 28828639.
Article44. Choi EJ, Lee JH, Park HS, Lee JH, Seol M, Lee YS, et al. Decitabine versus intensive chemotherapy for elderly patients with newly diagnosed acute myeloid leukemia. Clin Lymphoma Myeloma Leuk. 2019; 19(5):290–299.e3. PMID: 30879987.
Article45. Österroos A, Eriksson A, Antunovic P, Cammenga J, Deneberg S, Lazarevic V, et al. Real-world data on treatment patterns and outcomes of hypomethylating therapy in patients with newly diagnosed acute myeloid leukaemia aged ≥ 60 years. Br J Haematol. 2020; 189(1):e13–e16. PMID: 32103493.46. Amadori S, Suciu S, Selleslag D, Aversa F, Gaidano G, Musso M, et al. Gemtuzumab ozogamicin versus best supportive care in older patients with newly diagnosed acute myeloid leukemia unsuitable for intensive chemotherapy: results of the randomized phase III EORTC-GIMEMA AML-19 trial. J Clin Oncol. 2016; 34(9):972–979. PMID: 26811524.
Article47. Cortes JE, Heidel FH, Hellmann A, Fiedler W, Smith BD, Robak T, et al. Randomized comparison of low dose cytarabine with or without glasdegib in patients with newly diagnosed acute myeloid leukemia or high-risk myelodysplastic syndrome. Leukemia. 2019; 33(2):379–389. PMID: 30555165.
Article48. DiNardo CD, Pratz K, Pullarkat V, Jonas BA, Arellano M, Becker PS, et al. Venetoclax combined with decitabine or azacitidine in treatment-naive, elderly patients with acute myeloid leukemia. Blood. 2019; 133(1):7–17. PMID: 30361262.
Article49. Lambert J, Pautas C, Terré C, Raffoux E, Turlure P, Caillot D, et al. Gemtuzumab ozogamicin for de novo acute myeloid leukemia: final efficacy and safety updates from the open-label, phase III ALFA-0701 trial. Haematologica. 2019; 104(1):113–119. PMID: 30076173.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Real-World Treatment Intensity and Patterns in Patients With Myopic Choroidal Neovascularization: Common Data Model in Ophthalmology
- Changing the strategic paradigm for the treatment of adult acute myeloid leukemia
- FLT3 mutations in acute myeloid leukemia: a review focusing on clinically applicable drugs
- Posaconazole versus Itraconazole as Prophylactic Antifungal Agents during Induction Chemotherapy for Acute Myeloid Leukemia: A Real-World Single Center Comparison
- Systemic treatment for advanced urothelial cancer: an update on recent clinical trials and current treatment options