Clin Endosc.
2023 Nov;56(6):754-760. 10.5946/ce.2022.177.
Endoscopic vacuum therapy for treatment of spontaneous and iatrogenic upper gastrointestinal defects
- Affiliations
-
- 1Department of Medicine, Baylor College of Medicine, Houston, TX, USA
- 2Section of Gastroenterology and Hepatology, Baylor College of Medicine, Houston, TX, USA
- 3Austin Gastroenterology PA, Austin, TX, USA
- KMID: 2547897
- DOI: http://doi.org/10.5946/ce.2022.177
Abstract
- Background/Aims
Endoscopic vacuum therapy (EVT) can heal a variety of defects within the gastrointestinal (GI) tract via applying negative pressure, which reduces the defect size, aspirates the infected fluid, and promotes granulation tissue. Here we present our experience with EVT as it relates to both spontaneous and iatrogenic upper GI tract perforations, leaks, and fistulas.
Methods
This retrospective study was conducted at four large hospital centers. All patients who underwent EVT between June 2018 and March 2021 were included. Data on multiple variables were collected, including demographics, defect size and location, number and intervals of EVT exchanges, technical success, and hospital length of stay. Student t-test and the chi-squared test were used to analyze the data.
Results
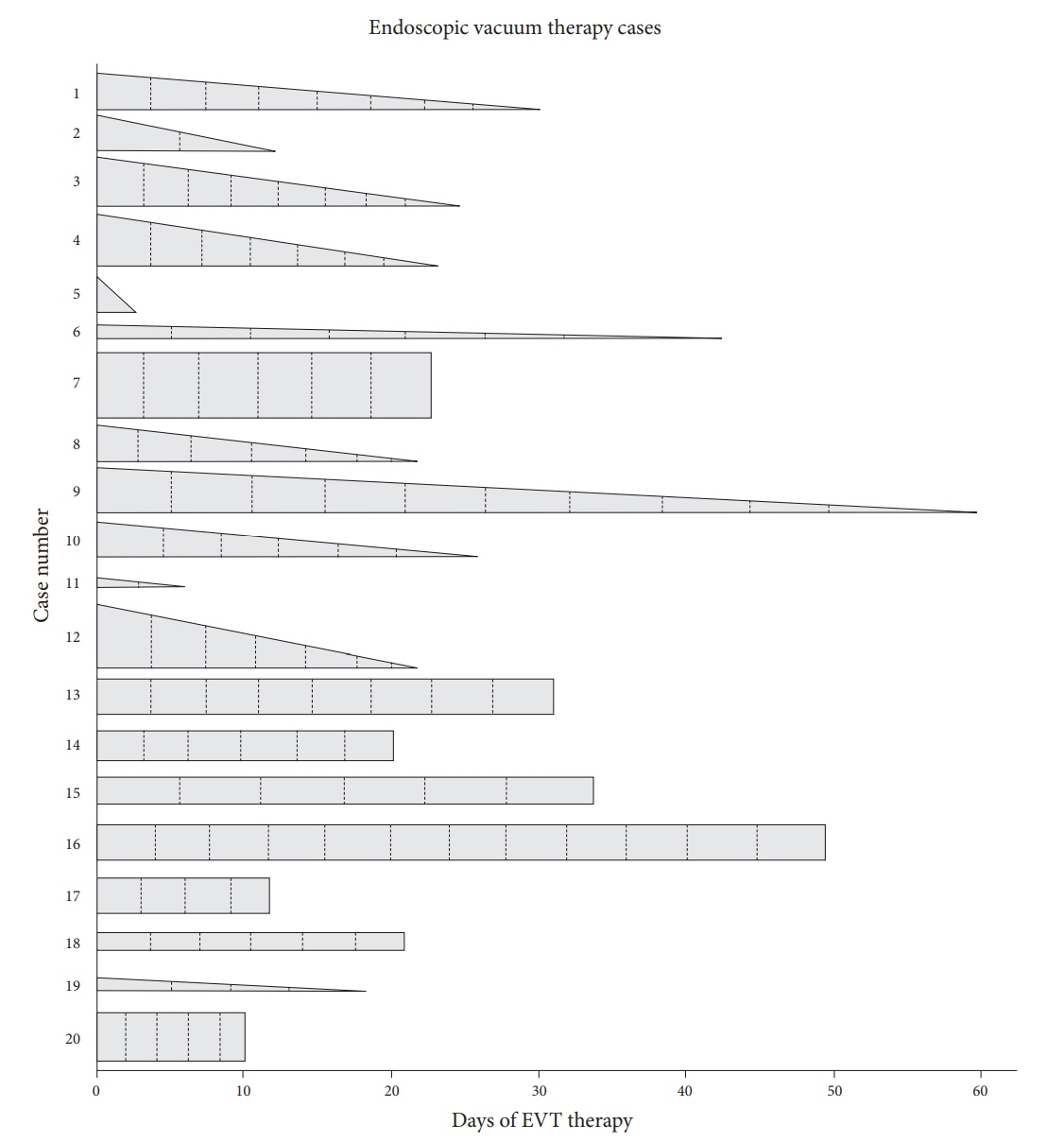
Twenty patients underwent EVT. The most common defect cause was spontaneous esophageal perforation (50%). The most common defect location was the distal esophagus (55%). The success rate was 80%. Seven patients were treated with EVT as the primary closure method. The mean number of exchanges was five with a mean interval of 4.3 days between exchanges. The mean length of hospital stay was 55.8 days.
Conclusions
EVT is a safe and effective initial management option for esophageal leaks and perforations.
Figure
Reference
-
1. Fleischmann W, Strecker W, Bombelli M, et al. Vacuum sealing as treatment of soft tissue damage in open fractures. Unfallchirurg. 1993; 96:488–492.2. Abdulsada M, Sealock RJ, Cornwell L, et al. Endoluminal vacuum therapy of esophageal perforations. VideoGIE. 2019; 5:8–10.
Article3. Weidenhagen R, Gruetzner KU, Wiecken T, et al. Endoscopic vacuum-assisted closure of anastomotic leakage following anterior resection of the rectum: a new method. Surg Endosc. 2008; 22:1818–1825.
Article4. Wedemeyer J, Schneider A, Manns MP, et al. Endoscopic vacuum-assisted closure of upper intestinal anastomotic leaks. Gastrointest Endosc. 2008; 67:708–711.
Article5. Kuehn F, Loske G, Schiffmann L, et al. Endoscopic vacuum therapy for various defects of the upper gastrointestinal tract. Surg Endosc. 2017; 31:3449–3458.
Article6. Neumann PA, Mennigen R, Palmes D, et al. Pre-emptive endoscopic vacuum therapy for treatment of anastomotic ischemia after esophageal resections. Endoscopy. 2017; 49:498–503.
Article7. Lalezari S, Lee CJ, Borovikova AA, et al. Deconstructing negative pressure wound therapy. Int Wound J. 2017; 14:649–657.
Article8. Mennigen R, Senninger N, Laukoetter MG. Novel treatment options for perforations of the upper gastrointestinal tract: endoscopic vacuum therapy and over-the-scope clips. World J Gastroenterol. 2014; 20:7767–7776.
Article9. Pournaras DJ, Hardwick RH, Safranek PM, et al. Endoluminal vacuum therapy (E-Vac): a treatment option in oesophagogastric surgery. World J Surg. 2018; 42:2507–2511.
Article10. Still S, Mencio M, Ontiveros E, et al. Primary and rescue endoluminal vacuum therapy in the management of esophageal perforations and leaks. Ann Thorac Cardiovasc Surg. 2018; 24:173–179.
Article11. Heits N, Stapel L, Reichert B, et al. Endoscopic endoluminal vacuum therapy in esophageal perforation. Ann Thorac Surg. 2014; 97:1029–1035.
Article12. Rubicondo C, Lovece A, Pinelli D, et al. Endoluminal vacuum-assisted closure (E-Vac) therapy for postoperative esophageal fistula: successful case series and literature review. World J Surg Oncol. 2020; 18:301.
Article13. Durbin S, Aranez JL, Shobassy M, et al. Endoluminal vacuum therapy in the management of a large gastrobronchial fistula. VideoGIE. 2020; 5:552–554.
Article14. de Medeiros FS, Junior ES, França RL, et al. Preemptive endoluminal vacuum therapy after pancreaticoduodenectomy: a case report. World J Gastrointest Endosc. 2020; 12:493–499.
Article15. Jung DH, Huh CW, Min YW, et al. Endoscopic vacuum therapy for the management of upper GI leaks and perforations: a multicenter retrospective study of factors associated with treatment failure (with video). Gastrointest Endosc. 2022; 95:281–290.
Article16. Leeds SG, Mencio M, Ontiveros E, et al. Endoluminal vacuum therapy: how I do it. J Gastrointest Surg. 2019; 23:1037–1043.
Article17. Mennigen R, Harting C, Lindner K, et al. Comparison of endoscopic vacuum therapy versus stent for anastomotic leak after esophagectomy. J Gastrointest Surg. 2015; 19:1229–1235.
Article18. Brangewitz M, Voigtländer T, Helfritz FA, et al. Endoscopic closure of esophageal intrathoracic leaks: stent versus endoscopic vacuum-assisted closure, a retrospective analysis. Endoscopy. 2013; 45:433–438.
Article19. Ahrens M, Schulte T, Egberts J, et al. Drainage of esophageal leakage using endoscopic vacuum therapy: a prospective pilot study. Endoscopy. 2010; 42:693–698.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Treatments in Perforation or Fistula in Upper Gastrointestinal Tract
- Endoscopic Management of Nonvariceal Upper Gastrointestinal Bleeding
- Endoscopic Vacuum-assisted Closure in a Patient with an Overtube-induced Esophageal Perforation
- Endoscopic Closure for Full-Thickness Gastrointestinal Defects: Available Applications and Emerging Innovations
- Clinical Evaluation of Endoscopic Microwave Coagulation Therapy for Upper Gastrointestinal Bleeding