Brain Tumor Res Treat.
2023 Oct;11(4):289-294. 10.14791/btrt.2023.0035.
Awake Surgery for Lesional Epilepsy in Resource-Limited Settings: Case Report and Review of Literature
- Affiliations
-
- 1Section of Neurosurgery, Department of Surgery, The Aga Khan University, Karachi, Pakistan
- 2Department of Anesthesiology, The Aga Khan University, Karachi, Pakistan
- 3Medical College, The Aga Khan University, Karachi, Pakistan
- KMID: 2547409
- DOI: http://doi.org/10.14791/btrt.2023.0035
Abstract
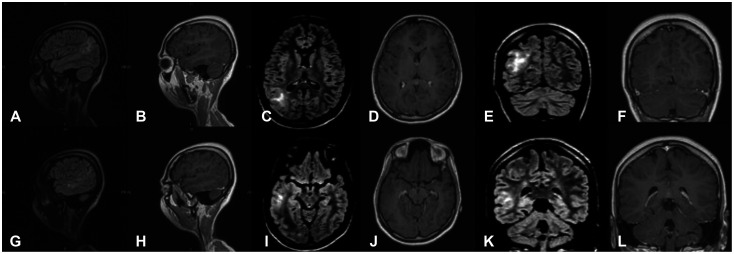
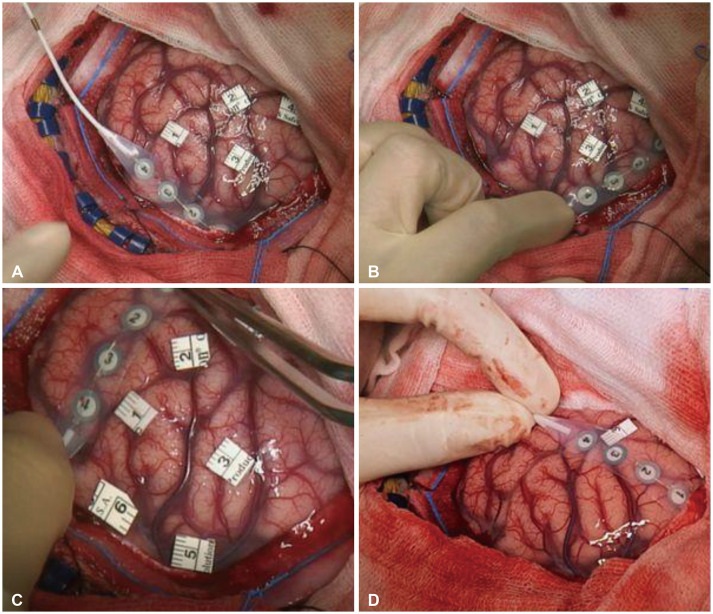
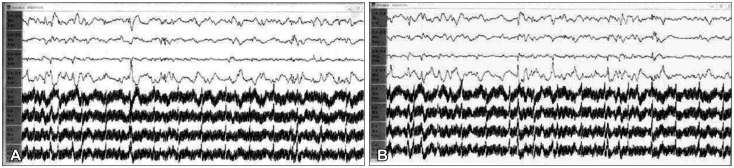
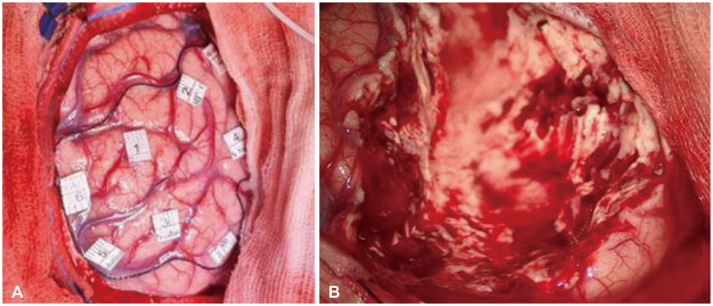
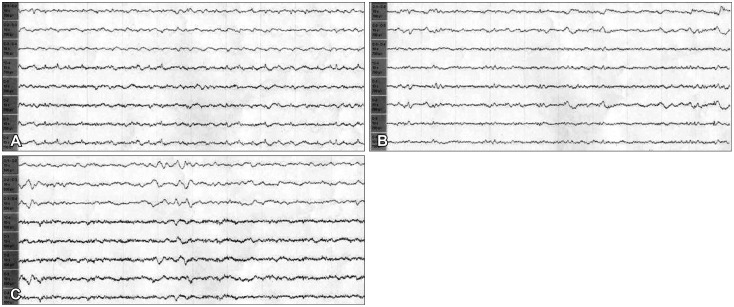
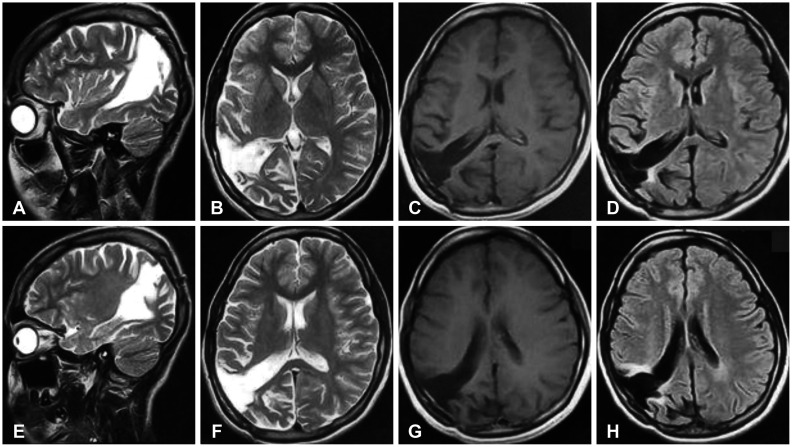
- Epilepsy surgery is a well-established treatment for drug-resistant epilepsy, with awake craniotomy being used in certain cases to remove epileptogenic foci while preserving crucial brain functions. We are presenting the first reported case from Pakistan of a 19-year-old woman who underwent awake epilepsy surgery to treat cortical dysplasia. She had a history of generalized tonic-clonic seizures since her childhood and was referred to our clinic due to an increase in seizure frequency. EEG and MRI identified the epileptogenic focus in the right parieto-temporal region. The patient underwent a neuro-navigation guided awake craniotomy and an excision of the epileptogenic focus in the right parieto-temporal region. The procedure was carried out using a scalp block and dexmedetomidine for conscious sedation, enabling the patient to remain awake throughout the surgery. Intraoperative mapping and electrocorticography were used for complex multidisciplinary care. Post-resection corticography showed no spikes along the resected margins. The patient was discharged without any complications and remained free of symptoms a year after the surgery. Awake epilepsy surgery is a viable option for removing epileptogenic foci while preserving vital cognitive functions. However, it is seldom used in low- and middle-income countries such as Pakistan. The successful outcome of this case underscores the need for greater awareness and availability of epilepsy surgery in resource-limited settings. Cost-effective measures, such as using small subdural strips for intraoperative localization, can be implemented.
Figure
Reference
-
1. Maesawa S, Nakatsubo D, Fujii M, Iijima K, Kato S, Ishizaki T, et al. Application of awake surgery for epilepsy in clinical practice. Neurol Med Chir (Tokyo). 2018; 58:442–452. PMID: 30249918.
Article2. Korkar GH, Isnard J, Montavont A, Catenoix H, Rheims S, Guénot M. Awake craniotomy for epilepsy surgery on eloquent speech areas: a single-centre experience. Epileptic Disord. 2021; 23:347–356. PMID: 33926856.
Article3. Choi SA, Kim KJ. The surgical and cognitive outcomes of focal cortical dysplasia. J Korean Neurosurg Soc. 2019; 62:321–327. PMID: 31085958.
Article4. Hauptman JS, Mathern GW. Surgical treatment of epilepsy associated with cortical dysplasia: 2012 update. Epilepsia. 2012; 53(Suppl 4):98–104.
Article5. Cohen-Gadol AA, Ozduman K, Bronen RA, Kim JH, Spencer DD. Long-term outcome after epilepsy surgery for focal cortical dysplasia. J Neurosurg. 2004; 101:55–65. PMID: 15255252.
Article6. Minkin K, Gabrovski K, Karazapryanov P, Milenova Y, Sirakov S, Karakostov V, et al. Awake epilepsy surgery in patients with focal cortical dysplasia. World Neurosurg. 2021; 151:e257–e264. PMID: 33872840.
Article7. Khatri IA, Iannaccone ST, Ilyas MS, Abdullah M, Saleem S. Epidemiology of epilepsy in Pakistan: review of literature. J Pak Med Assoc. 2003; 53:594–597. PMID: 14765939.8. Shafiq F, Parkash J, Enam A, Khan MF, Baig T. An awake throughout approach for awake craniotomy: a perspective from a resource-limited country. World Neurosurg. 2019; 126:e1489–e1493. PMID: 30905650.
Article9. Shen SL, Zheng JY, Zhang J, Wang WY, Jin T, Zhu J, et al. Comparison of dexmedetomidine and propofol for conscious sedation in awake craniotomy: a prospective, double-blind, randomized, and controlled clinical trial. Ann Pharmacother. 2013; 47:1391–1399. PMID: 24259599.
Article10. Souter MJ, Rozet I, Ojemann JG, Souter KJ, Holmes MD, Lee L, et al. Dexmedetomidine sedation during awake craniotomy for seizure resection: effects on electrocorticography. J Neurosurg Anesthesiol. 2007; 19:38–44. PMID: 17198099.
Article11. Viderman D, Nabidollayeva F, Bilotta F, Abdildin YG. Comparison of dexmedetomidine and propofol for sedation in awake craniotomy: a meta-analysis. Clin Neurol Neurosurg. 2023; 226:107623. PMID: 36791589.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary Reading Epilepsy: A Case Report
- Discerning Trends in Multiplex Immunoassay Technology with Potential for Resource-Limited Settings
- Pediatric postintensive care syndrome: high burden and a gap in evaluation tools for limited-resource settings
- Temporal lobe epilepsy caused by intrahippocampal calcified cysticercus: a case report
- Outcome of Resective Surgery for Non-lesional Neocortical Temporal Lobe Epilepsy