J Yeungnam Med Sci.
2023 Oct;40(4):412-418. 10.12701/jyms.2023.00234.
Risk factors for prostate-specific antigen persistence in pT3aN0 prostate cancer after robot-assisted laparoscopic radical prostatectomy: a retrospective study
- Affiliations
-
- 1Department of Urology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2547365
- DOI: http://doi.org/10.12701/jyms.2023.00234
Abstract
- Background
The aim of this study was to evaluate the risk factors for prostate-specific antigen (PSA) persistence in pathological stage T3aN0 prostate cancer (PCa) after robot-assisted laparoscopic radical prostatectomy (RALP).
Methods
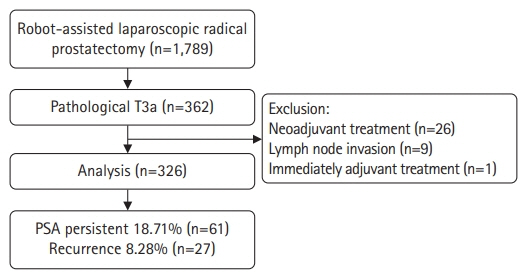
A retrospective study was performed on 326 patients with pT3aN0 PCa who underwent RALP between March 2020 and February 2022. PSA persistence was defined as nadir PSA of >0.1 ng/mL after RALP, and the risk factors for PSA persistence were evaluated using logistic regression analysis.
Results
Among 326 patients, 61 (18.71%) had PSA persistence and 265 (81.29%) had PSA of <0.1 ng/mL after RALP (successful radical prostatectomy [RP] group). In the PSA persistence group, 51 patients (83.61%) received adjuvant treatment. Biochemical recurrence occurred in 27 patients (10.19%) in the successful RP group during the mean follow-up period of 15.22 months. Multivariate analysis showed that the risk factors for PSA persistence were large prostate volume (hazard ratio [HR], 1.017; 95% confidence interval [CI], 1.002–1.036; p=0.046), lymphovascular invasion (LVI) (HR, 2.605; 95% CI, 1.022–6.643; p=0.045), and surgical margin involvement (HR, 2.220; 95% CI, 1.110–4.438; p=0.024).
Conclusion
Adjuvant treatment may be needed for improved prognosis in patients with pT3aN0 PCa after RALP with a large prostate size, LVI, or surgical margin involvement.
Keyword
Figure
Reference
-
References
1. Rakauskas A, Tawadros T, Lucca I, Herrera F, Bourhis J, Burruni R, et al. Active surveillance in males with low- to intermediate-risk localized prostate cancer: a modern prospective cohort study. Investig Clin Urol. 2021; 62:416–22.
Article2. Klotz L. Active surveillance in intermediate-risk prostate cancer. BJU Int. 2020; 125:346–54.
Article3. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020; 70:7–30.
Article4. Mottet N, Bellmunt J, Bolla M, Briers E, Cumberbatch MG, De Santis M, et al. EAU-ESTRO-SIOG Guidelines on Prostate Cancer. Part 1: Screening, diagnosis, and local treatment with curative intent. Eur Urol. 2017; 71:618–29.
Article5. Jang TL, Patel N, Faiena I, Radadia KD, Moore DF, Elsamra SE, et al. Comparative effectiveness of radical prostatectomy with adjuvant radiotherapy versus radiotherapy plus androgen deprivation therapy for men with advanced prostate cancer. Cancer. 2018; 124:4010–22.
Article6. van den Ouden D, Hop WC, Schröder FH. Progression in and survival of patients with locally advanced prostate cancer (T3) treated with radical prostatectomy as monotherapy. J Urol. 1998; 160:1392–7.
Article7. Gözen AS, Akin Y, Ates M, Hruza M, Rassweiler J. Impact of laparoscopic radical prostatectomy on clinical T3 prostate cancer: experience of a single centre with long-term follow-up. BJU Int. 2015; 116:102–8.
Article8. Koo KC, Cho JS, Bang WJ, Lee SH, Cho SY, Kim SI, et al. Cancer-specific mortality among Korean men with localized or locally advanced prostate cancer treated with radical prostatectomy versus radiotherapy: a multi-center study using propensity scoring and competing risk regression analyses. Cancer Res Treat. 2018; 50:129–37.
Article9. Moris L, Cumberbatch MG, Van den Broeck T, Gandaglia G, Fossati N, Kelly B, et al. Benefits and risks of primary treatments for high-risk localized and locally advanced prostate cancer: an international multidisciplinary systematic review. Eur Urol. 2020; 77:614–27.10. Kliment J Jr, Elias B, Baluchova K, Kliment J Sr. The long-term outcomes of radical prostatectomy for very high-risk prostate cancer pT3b-T4 N0-1 on definitive histopathology. Cent European J Urol. 2017; 70:13–9.11. Casey JT, Meeks JJ, Greco KA, Wu SD, Nadler RB. Outcomes of locally advanced (T3 or greater) prostate cancer in men undergoing robot-assisted laparoscopic prostatectomy. J Endourol. 2009; 23:1519–22.
Article12. Hajili T, Ohlmann CH, Linxweiler J, Niklas C, Janssen M, Siemer S, et al. Radical prostatectomy in T4 prostate cancer after inductive androgen deprivation: results of a single-institution series with long-term follow-up. BJU Int. 2019; 123:58–64.
Article13. Shipley WU, Seiferheld W, Lukka HR, Major PP, Heney NM, Grignon DJ, et al. Radiation with or without antiandrogen therapy in recurrent prostate cancer. N Engl J Med. 2017; 376:417–28.
Article14. Wiegel T, Bartkowiak D, Bottke D, Thamm R, Hinke A, Stöckle M, et al. Prostate-specific antigen persistence after radical prostatectomy as a predictive factor of clinical relapse-free survival and overall survival: 10-year data of the ARO 96-02 trial. Int J Radiat Oncol Biol Phys. 2015; 91:288–94.15. Rogers CG, Khan MA, Craig Miller M, Veltri RW, Partin AW. Natural history of disease progression in patients who fail to achieve an undetectable prostate-specific antigen level after undergoing radical prostatectomy. Cancer. 2004; 101:2549–56.
Article16. Moreira DM, Presti JC Jr, Aronson WJ, Terris MK, Kane CJ, Amling CL, et al. Natural history of persistently elevated prostate specific antigen after radical prostatectomy: results from the SEARCH database. J Urol. 2009; 182:2250–5.
Article17. Gandaglia G, Boorjian SA, Parker WP, Zaffuto E, Fossati N, Bandini M, et al. Impact of postoperative radiotherapy in men with persistently elevated prostate-specific antigen after radical prostatectomy for prostate cancer: a long-term survival analysis. Eur Urol. 2017; 72:910–7.
Article18. Fossati N, Karnes RJ, Colicchia M, Boorjian SA, Bossi A, Seisen T, et al. Impact of early salvage radiation therapy in patients with persistently elevated or rising prostate-specific antigen after radical prostatectomy. Eur Urol. 2018; 73:436–44.
Article19. Preisser F, Chun FK, Pompe RS, Heinze A, Salomon G, Graefen M, et al. Persistent prostate-specific antigen after radical prostatectomy and its impact on oncologic outcomes. Eur Urol. 2019; 76:106–14.
Article20. Freedland SJ, Isaacs WB, Platz EA, Terris MK, Aronson WJ, Amling CL, et al. Prostate size and risk of high-grade, advanced prostate cancer and biochemical progression after radical prostatectomy: a search database study. J Clin Oncol. 2005; 23:7546–54.
Article21. Min SH, Park YH, Lee SB, Ku JH, Kwak C, Kim HH. Impact of prostate size on pathologic outcomes and prognosis after radical prostatectomy. Korean J Urol. 2012; 53:463–6.
Article22. Loeb S, Roehl KA, Yu X, Antenor JA, Han M, Gashti SN, et al. Lymphovascular invasion in radical prostatectomy specimens: prediction of adverse pathologic features and biochemical progression. Urology. 2006; 68:99–103.
Article23. May M, Kaufmann O, Hammermann F, Loy V, Siegsmund M. Prognostic impact of lymphovascular invasion in radical prostatectomy specimens. BJU Int. 2007; 99:539–44.
Article24. Jamil M, Rakic N, Sood A, Keeley J, Modonutti D, Novara G, et al. Impact of lymphovascular invasion on overall survival in patients with prostate cancer following radical prostatectomy: stage-per-stage analysis. Clin Genitourin Cancer. 2021; 19:e319–25.
Article25. Zhang L, Wu B, Zha Z, Zhao H, Jiang Y, Yuan J. Positive surgical margin is associated with biochemical recurrence risk following radical prostatectomy: a meta-analysis from high-quality retrospective cohort studies. World J Surg Oncol. 2018; 16:124.
Article26. Hegemann NS, Morcinek S, Buchner A, Karl A, Stief C, Knüchel R, et al. Risk of biochemical recurrence and timing of radiotherapy in pT3a N0 prostate cancer with positive surgical margin: a single center experience. Strahlenther Onkol. 2016; 192:440–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radical Prostatectomy
- A Case of Robot-Assisted Laparoscopic Radical Prostatectomy in Primary Small Cell Prostate Cancer
- Robot-Assisted Laparoscopic Radical Prostatectomy: Four Cases
- Clinical Experience with Limited Lymph Node Dissection for Prostate Cancer in Korea: Single Center Comparison of 247 Open and 354 Robot-Assisted Laparoscopic Radical Prostatectomy Series
- Robot-assisted Laparoscopic Radical Prostatectomy