J Korean Med Sci.
2023 Oct;38(41):e353. 10.3346/jkms.2023.38.e353.
Empiric Anti-Pseudomonal β-Lactam Monotherapy Versus Fluoroquinolone Combination Therapy in Patients With Hospital-Acquired Pneumonia: A Multicenter Cohort Study With Propensity Score Matching
- Affiliations
-
- 1Division of Pulmonary, Allergy and Critical Care Medicine, Department of Internal Medicine, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Korea
- 2Division of Allergy and Pulmonary Medicine, Department of Internal Medicine, Soonchunhyang University Bucheon Hospital, Bucheon, Korea
- 3Department of Pulmonary and Critical Care Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 4Department of Integrated Internal Medicine, Myoungji Hospital, Hanyang University College of Medicine, Goyang, Korea
- 5Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea
- 6Department of Internal Medicine, Jeju National University Hospital, Jeju National University School of Medicine, Jeju, Korea
- 7Department of Internal Medicine, Division of Pulmonology, Allergy and Critical Care Medicine, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea
- 8Division of Allergy, Pulmonary and Critical Care Medicine, Department of Internal Medicine, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Busan, Korea
- 9Division of Respiratory and Critical Care Medicine, Department of Internal Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea
- 10Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Inje University Sanggye Paik Hospital, Seoul, Korea
- 11Department of Internal Medicine, Research Center for Pulmonary Disorders, Jeonbuk National University Hospital, Jeonju, Korea
- 12Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- 13Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea
- 14Division of Pulmonary, Allergy and Critical Care Medicine, Department of Internal Medicine, Konkuk University School of Medicine, Seoul, Korea
- 15Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Internal Medicine, Chungnam National University College of Medicine, Sejong Hospital, Sejong, Korea
- 16Division of Pulmonary, Allergy and Critical Care Medicine, Department of Internal Medicine, Korea University Guro Hospital, Seoul, Korea
- 17Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2547180
- DOI: http://doi.org/10.3346/jkms.2023.38.e353
Abstract
- Background
There is insufficient data on the benefits of empiric antibiotic combinations for hospital-acquired pneumonia (HAP). We aimed to investigate whether empiric antipseudomonal combination therapy with fluoroquinolones decreases mortality in patients with HAP.
Methods
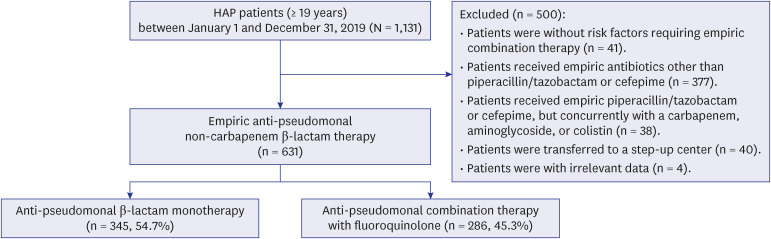
This multicenter, retrospective cohort study included adult patients admitted to 16 tertiary and general hospitals in Korea between January 1 and December 31, 2019. Patients with risk factors for combination therapy were divided into anti-pseudomonal non-carbapenem β-lactam monotherapy and fluoroquinolone combination therapy groups. Primary outcome was 30-day mortality. Propensity score matching (PSM) was used to reduce selection bias.
Results
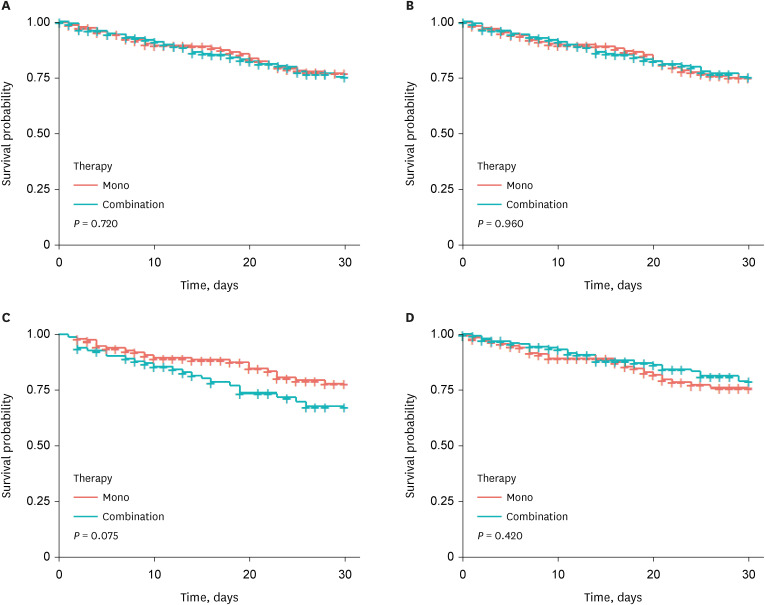
In total, 631 patients with HAP were enrolled. Monotherapy was prescribed in 54.7% (n = 345) of the patients, and combination therapy was prescribed in 45.3% (n = 286). There was no significant difference in 30-day mortality between the two groups (16.8% vs. 18.2%, P = 0.729) or even after the PSM (17.5% vs. 18.2%, P = 0.913). After the PSM, adjusted hazard ratio for 30-day mortality from the combination therapy was 1.646 (95% confidence interval, 0.782–3.461; P = 0.189) in the Cox proportional hazards model. Moreover, there was no significant difference in the appropriateness of initial empiric antibiotics between the two groups (55.0% vs. 56.8%, P = 0.898). The proportion of multidrug-resistant (MDR) pathogens was high in both groups.
Conclusion
Empiric anti-pseudomonal fluoroquinolone combination therapy showed no survival benefit compared to β-lactam monotherapy in patients with HAP. Caution is needed regarding the routine combination of fluoroquinolones in the empiric treatment of HAP patients with a high risk of MDR.
Keyword
Figure
Reference
-
1. Jiao J, Li Z, Wu X, Cao J, Liu G, Liu Y, et al. Risk factors for 3-month mortality in bedridden patients with hospital-acquired pneumonia: a multicentre prospective study. PLoS One. 2021; 16(3):e0249198. PMID: 33784317.2. Xu E, Pérez-Torres D, Fragkou PC, Zahar JR, Koulenti D. Nosocomial pneumonia in the era of multidrug-resistance: updates in diagnosis and management. Microorganisms. 2021; 9(3):534. PMID: 33807623.3. Zaragoza R, Vidal-Cortés P, Aguilar G, Borges M, Diaz E, Ferrer R, et al. Update of the treatment of nosocomial pneumonia in the ICU. Crit Care. 2020; 24(1):383. PMID: 32600375.4. Kalil AC, Metersky ML, Klompas M, Muscedere J, Sweeney DA, Palmer LB, et al. Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 clinical practice guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016; 63(5):e61–111. PMID: 27418577.5. Ko RE, Min KH, Hong SB, Baek AR, Lee HK, Cho WH, et al. Characteristics, management, and clinical outcomes of patients with hospital-acquired and ventilator-associated pneumonia: a multicenter cohort study in Korea. Tuberc Respir Dis (Seoul). 2021; 84(4):317–325. PMID: 34134465.6. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016; 315(8):801–810. PMID: 26903338.7. Mandell LA, Niederman MS. Aspiration pneumonia. N Engl J Med. 2019; 380(7):651–663. PMID: 30763196.8. Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012; 18(3):268–281. PMID: 21793988.9. Vilella AL, Seifert CF. Timing and appropriateness of initial antibiotic therapy in newly presenting septic patients. Am J Emerg Med. 2014; 32(1):7–13. PMID: 24139996.10. Raman G, Avendano E, Berger S, Menon V. Appropriate initial antibiotic therapy in hospitalized patients with gram-negative infections: systematic review and meta-analysis. BMC Infect Dis. 2015; 15(1):395. PMID: 26423743.11. Merchant S, Proudfoot EM, Quadri HN, McElroy HJ, Wright WR, Gupta A, et al. Risk factors for Pseudomonas aeruginosa infections in Asia-Pacific and consequences of inappropriate initial antimicrobial therapy: a systematic literature review and meta-analysis. J Glob Antimicrob Resist. 2018; 14:33–44. PMID: 29454906.12. Chung DR, Song JH, Kim SH, Thamlikitkul V, Huang SG, Wang H, et al. High prevalence of multidrug-resistant nonfermenters in hospital-acquired pneumonia in Asia. Am J Respir Crit Care Med. 2011; 184(12):1409–1417. PMID: 21920919.13. Assefa M. Multi-drug resistant gram-negative bacterial pneumonia: etiology, risk factors, and drug resistance patterns. Pneumonia. 2022; 14(1):4. PMID: 35509063.14. Marquet K, Liesenborgs A, Bergs J, Vleugels A, Claes N. Incidence and outcome of inappropriate in-hospital empiric antibiotics for severe infection: a systematic review and meta-analysis. Crit Care. 2015; 19(1):63. PMID: 25888181.15. Puzniak L, DePestel DD, Srinivasan A, Ye G, Murray J, Merchant S, et al. A combination antibiogram evaluation for Pseudomonas aeruginosa in respiratory and blood sources from intensive care unit (ICU) and non-ICU settings in U.S. hospitals. Antimicrob Agents Chemother. 2019; 63(4):e02564-18. PMID: 30917987.16. Luu Q, Vitale K, Shan G, Jayakumar R, Viswesh V. Evaluation of guideline recommendations for dual antipseudomonal therapy in hospitalized adults with pneumonia using combination antibiograms. Pharmacotherapy. 2020; 40(11):1089–1098. PMID: 33037659.17. Kang JS, Moon C, Mun SJ, Lee JE, Lee SO, Lee S, et al. Antimicrobial susceptibility trends and risk factors for antimicrobial resistance in Pseudomonas aeruginosa bacteremia: 12-year experience in a Tertiary Hospital in Korea. J Korean Med Sci. 2021; 36(43):e273. PMID: 34751008.18. Klinker KP, Hidayat LK, DeRyke CA, DePestel DD, Motyl M, Bauer KA. Antimicrobial stewardship and antibiograms: importance of moving beyond traditional antibiograms. Ther Adv Infect Dis. 2021; 8:20499361211011373. PMID: 33996074.19. Jang JH, Yeo HJ, Kim T, Cho WH, Min KH, Hong SB, et al. Microbiologic pattern and clinical outcome of non-ICU-acquired pneumonia: Korean HAP registry analysis. Korean J Intern Med. 2022; 37(4):800–810. PMID: 35811368.20. Chang Y, Jeon K, Lee SM, Cho YJ, Kim YS, Chong YP, et al. The distribution of multidrug-resistant microorganisms and treatment status of hospital-acquired pneumonia/ventilator-associated pneumonia in adult intensive care units: a prospective cohort observational study. J Korean Med Sci. 2021; 36(41):e251. PMID: 34697926.21. Bae MH, Kim MS, Kim TS, Kim S, Yong D, Ha GY, et al. Changing epidemiology of pathogenic bacteria over the past 20 years in Korea. J Korean Med Sci. 2023; 38(10):e73. PMID: 36918027.22. Wenzler E, Goff DA, Humphries R, Goldstein EJC. Anticipating the unpredictable: a review of antimicrobial stewardship and Acinetobacter infections. Infect Dis Ther. 2017; 6(2):149–172. PMID: 28260148.23. Kim YA, Park YS. Epidemiology and treatment of antimicrobial-resistant gram-negative bacteria in Korea. Korean J Intern Med. 2018; 33(2):247–255. PMID: 29506343.24. Tamma PD, Aitken SL, Bonomo RA, Mathers AJ, van Duin D, Clancy CJ. Infectious Diseases Society of America guidance on the treatment of AmpC β-lactamase-producing Enterobacterales, carbapenem-resistant Acinetobacter baumannii, and Stenotrophomonas maltophilia infections. Clin Infect Dis. 2022; 74(12):2089–2114. PMID: 34864936.25. Latibeaudiere R, Rosa R, Laowansiri P, Arheart K, Namias N, Munoz-Price LS. Surveillance cultures growing carbapenem-resistant Acinetobacter baumannii predict the development of clinical infections: a retrospective cohort study. Clin Infect Dis. 2015; 60(3):415–422. PMID: 25352586.26. Tacconelli E, Cataldo MA, De Pascale G, Manno D, Spanu T, Cambieri A, et al. Prediction models to identify hospitalized patients at risk of being colonized or infected with multidrug-resistant Acinetobacter baumannii calcoaceticus complex. J Antimicrob Chemother. 2008; 62(5):1130–1137. PMID: 18635519.27. Owens RC Jr, Ambrose PG. Antimicrobial safety: focus on fluoroquinolones. Clin Infect Dis. 2005; 41(Suppl 2):S144–S157. PMID: 15942881.28. Mullish BH, Williams HR. Clostridium difficile infection and antibiotic-associated diarrhoea. Clin Med (Lond). 2018; 18(3):237–241. PMID: 29858434.29. McDonald LC, Gerding DN, Johnson S, Bakken JS, Carroll KC, Coffin SE, et al. Clinical practice guidelines for Clostridium difficile infection in adults and children: 2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. 2018; 66(7):e1–48. PMID: 29462280.30. Kuula LSM, Backman JT, Blom ML. Healthcare costs and mortality associated with serious fluoroquinolone-related adverse reactions. Pharmacol Res Perspect. 2022; 10(2):e00931. PMID: 35170862.31. Neuhauser MM, Weinstein RA, Rydman R, Danziger LH, Karam G, Quinn JP. Antibiotic resistance among gram-negative bacilli in US intensive care units: implications for fluoroquinolone use. JAMA. 2003; 289(7):885–888. PMID: 12588273.32. Paramythiotou E, Lucet JC, Timsit JF, Vanjak D, Paugam-Burtz C, Trouillet JL, et al. Acquisition of multidrug-resistant Pseudomonas aeruginosa in patients in intensive care units: role of antibiotics with antipseudomonal activity. Clin Infect Dis. 2004; 38(5):670–677. PMID: 14986251.33. Kopterides P, Koletsi PK, Michalopoulos A, Falagas ME. Exposure to quinolones is associated with carbapenem resistance among colistin-susceptible Acinetobacter baumannii blood isolates. Int J Antimicrob Agents. 2007; 30(5):409–414. PMID: 17851052.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Community Acquired Pneumonia
- Beta-Lactam Plus Macrolide for Patients Hospitalized With CommunityAcquired Pneumonia: Difference Between Autumn and Spring
- Is β-Lactam Plus Macrolide More Effective than β-Lactam Plus Fluoroquinolone among Patients with Severe Community-Acquired Pneumonia?: a Systemic Review and Meta-Analysis
- The Etiologies and Initial Antimicrobial Therapy Outcomes in One Tertiary Hospital ICU-admitted Patient with Severe Community- acquired Pneumonia
- Antibiotic Resistance and Treatment Update of Community-Acquired Pneumonia