Acute Crit Care.
2023 Aug;38(3):315-324. 10.4266/acc.2023.00500.
Risk factors for cannula-associated arterial thrombosis following extracorporeal membrane oxygenation support: a retrospective study
- Affiliations
-
- 1Department of Emergency and Critical Care Medicine, University of Medicine and Pharmacy at Ho Chi Minh City, Ho Chi Minh City, Vietnam
- 2Intensive Care Unit, Cho Ray Hospital, Ho Chi Minh City, Vietnam
- 3Intensive Care Unit, Tam Anh Hospital, Ho Chi Minh City, Vietnam
- KMID: 2547025
- DOI: http://doi.org/10.4266/acc.2023.00500
Abstract
- Background
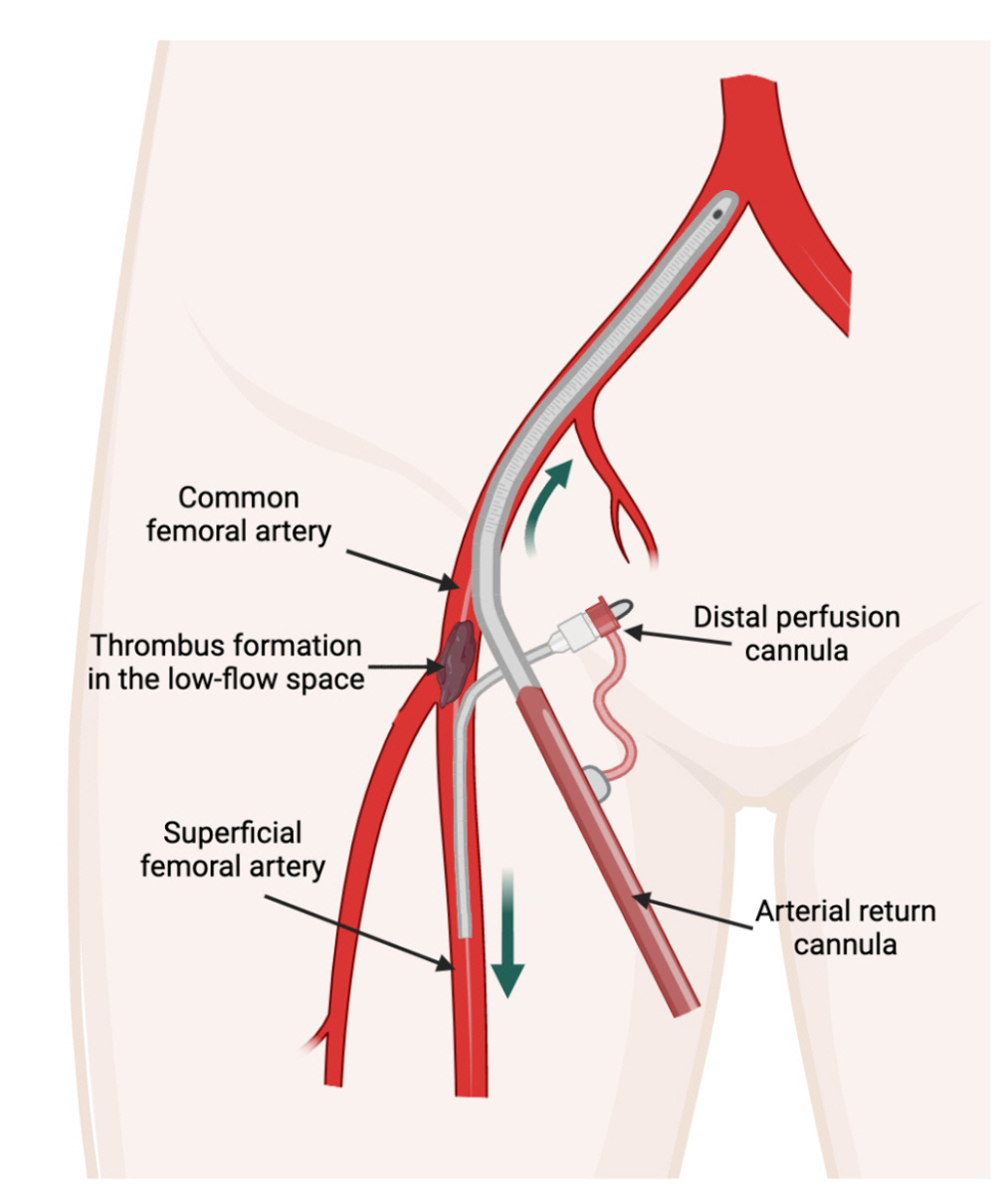
Hemostatic dysfunction during extracorporeal membrane oxygenation (ECMO) due to blood-circuit interaction and the consequences of shear stress imposed by flow rates lead to rapid coagulation cascade and thrombus formation in the ECMO system and blood vessels. We aimed to identify the incidence and risk factors for cannula-associated arterial thrombosis (CaAT) post-decannulation.
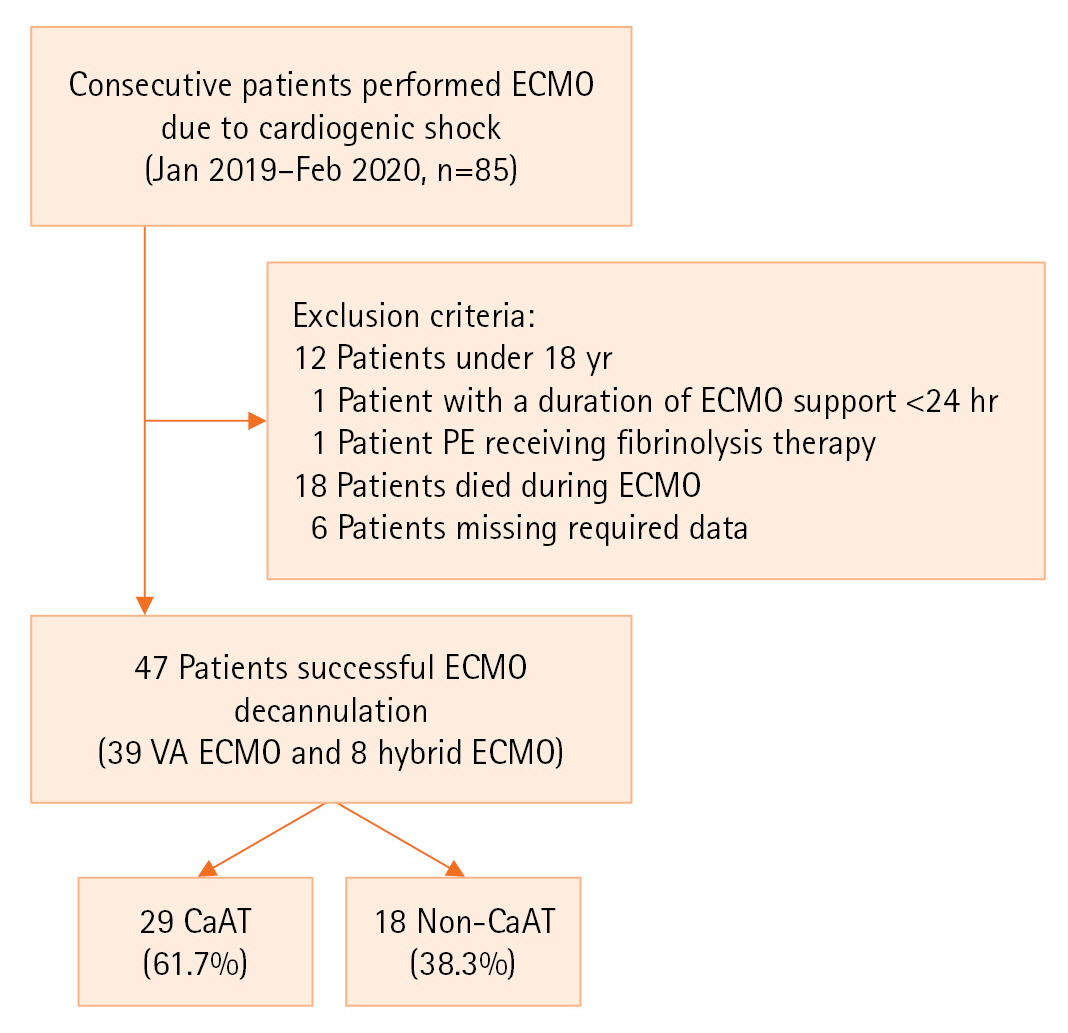
Methods
A retrospective study of patients undergoing arterial cannula removal following ECMO was performed. We evaluated the incidence of CaAT and compared the characteristics, ECMO machine parameters, cannula sizes, number of blood products transfused during ECMO, and daily hemostasis parameters in patients with and without CaAT. Multivariate analysis identified the risk factors for CaAT.
Results
Forty-seven patients requiring venoarterial ECMO (VA-ECMO) or hybrid methods were recruited for thrombosis screening. The median Sequential Organ Failure Assessment score was 11 (interquartile range, 8–13). CaAT occurred in 29 patients (61.7%), with thrombosis in the superficial femoral artery accounting for 51.7% of cases. The rate of limb ischemia complications in the CaAT group was 17.2%. Multivariate analysis determined that the ECMO flow rate–body surface area (BSA) ratio (100 ml/min/m2) was an independent factor for CaAT, with an odds ratio of 0.79 (95% confidence interval, 0.66–0.95; P=0.014).
Conclusions
We found that the incidence of CaAT was 61.7% following successful decannulation from VA-ECMO or hybrid modes, and the ECMO flow rate–BSA ratio was an independent risk factor for CaAT. We suggest screening for arterial thrombosis following VA-ECMO, and further research is needed to determine the risks and benefits of such screening.
Figure
Reference
-
1. Pineton de Chambrun M, Bréchot N, Combes A. Venoarterial extracorporeal membrane oxygenation in cardiogenic shock: indications, mode of operation, and current evidence. Curr Opin Crit Care. 2019; 25:397–402.
Article2. Doyle AJ, Hunt BJ. Current understanding of how extracorporeal membrane oxygenators activate haemostasis and other blood components. Front Med (Lausanne). 2018; 5:352.
Article3. Esper SA, Levy JH, Waters JH, Welsby IJ. Extracorporeal membrane oxygenation in the adult: a review of anticoagulation monitoring and transfusion. Anesth Analg. 2014; 118:731–43.4. Bonicolini E, Martucci G, Simons J, Raffa GM, Spina C, Lo Coco V, et al. Limb ischemia in peripheral veno-arterial extracorporeal membrane oxygenation: a narrative review of incidence, prevention, monitoring, and treatment. Crit Care. 2019; 23:266.
Article5. Bisdas T, Beutel G, Warnecke G, Hoeper MM, Kuehn C, Haverich A, et al. Vascular complications in patients undergoing femoral cannulation for extracorporeal membrane oxygenation support. Ann Thorac Surg. 2011; 92:626–31.
Article6. Kim J, Cho YH, Sung K, Park TK, Lee GY, Lee JM, et al. Impact of cannula size on clinical outcomes in peripheral venoarterial extracorporeal membrane oxygenation. ASAIO J. 2019; 65:573–9.
Article7. Tanaka D, Hirose H, Cavarocchi N, Entwistle JW. The impact of vascular complications on survival of patients on venoarterial extracorporeal membrane oxygenation. Ann Thorac Surg. 2016; 101:1729–34.
Article8. Yen CC, Kao CH, Tsai CS, Tsai SH. Identifying the risk factor and prevention of limb ischemia in extracorporeal membrane oxygenation with femoral artery cannulation. Heart Surg Forum. 2018; 21:E018–22.
Article9. Lorusso R, Shekar K, MacLaren G, Schmidt M, Pellegrino V, Meyns B, et al. ELSO interim guidelines for venoarterial extracorporeal membrane oxygenation in adult cardiac patients. ASAIO J. 2021; 67:827–44.
Article10. Sulimov DS, Markuske M, Desch S, Thiele H. Management of dead space thrombosis during decannulation of peripherally inserted venoarterial extracorporeal membrane oxygenation. Catheter Cardiovasc Interv. 2021; 98:E122–3.
Article11. Cooper E, Burns J, Retter A, Salt G, Camporota L, Meadows CI, et al. Prevalence of venous thrombosis following venovenous extracorporeal membrane oxygenation in patients with severe respiratory failure. Crit Care Med. 2015; 43:e581–4.
Article12. Fisser C, Reichenbächer C, Müller T, Schneckenpointner R, Malfertheiner MV, Philipp A, et al. Incidence and risk factors for cannula-related venous thrombosis after venovenous extracorporeal membrane oxygenation in adult patients with acute respiratory failure. Crit Care Med. 2019; 47:e332–9.
Article13. Menaker J, Tabatabai A, Rector R, Dolly K, Kufera J, Lee E, et al. Incidence of cannula-associated deep vein thrombosis after veno-venous extracorporeal membrane oxygenation. ASAIO J. 2017; 63:588–91.
Article14. Parzy G, Daviet F, Persico N, Rambaud R, Scemama U, Adda M, et al. Prevalence and risk factors for thrombotic complications following venovenous extracorporeal membrane oxygenation: a CT scan study. Crit Care Med. 2020; 48:192–9.
Article15. Bidar F, Lancelot A, Lebreton G, Pineton de Chambrun M, Schmidt M, Hékimian G, et al. Venous or arterial thromboses after venoarterial extracorporeal membrane oxygenation support: frequency and risk factors. J Heart Lung Transplant. 2021; 40:307–15.
Article16. Cartwright B, Bruce HM, Kershaw G, Cai N, Othman J, Gattas D, et al. Hemostasis, coagulation and thrombin in venoarterial and venovenous extracorporeal membrane oxygenation: the HECTIC study. Sci Rep. 2021; 11:7975.
Article17. Kohs TC, Liu P, Raghunathan V, Amirsoltani R, Oakes M, McCarty OJ, et al. Severe thrombocytopenia in adults undergoing extracorporeal membrane oxygenation is predictive of thrombosis. Platelets. 2022; 33:570–6.
Article18. Lamarche Y, Chow B, Bédard A, Johal N, Kaan A, Humphries KH, et al. Thromboembolic events in patients on extracorporeal membrane oxygenation without anticoagulation. Innovations (Phila). 2010; 5:424–9.
Article19. Avenarius JK, Breek JC, Lampmann LE, van Berge Henegouwen DP, Hamming JF. The additional value of angiography after colour-coded duplex on decision making in patients with critical limb ischaemia: a prospective study. Eur J Vasc Endovasc Surg. 2002; 23:393–7.
Article20. Lai DT, Huber D, Glasson R, Grayndler V, Evans J, Hogg J, et al. Colour duplex ultrasonography versus angiography in the diagnosis of lower-extremity arterial disease. Cardiovasc Surg. 1996; 4:384–8.
Article21. Mennitt K, Deol M, Gao J. Emergency color Doppler sonography of the extremity artery: a pictorial essay. Clin Imaging. 2017; 42:240–8.
Article22. Patton-Rivera K, Beck J, Fung K, Chan C, Beck M, Takayama H, et al. Using near-infrared reflectance spectroscopy (NIRS) to assess distal-limb perfusion on venoarterial (V-A) extracorporeal membrane oxygenation (ECMO) patients with femoral cannulation. Perfusion. 2018; 33:618–23.
Article23. Thiagarajan RR, Barbaro RP, Rycus PT, Mcmullan DM, Conrad SA, Fortenberry JD, et al. Extracorporeal Life Support Organization Registry International Report 2016. ASAIO J. 2017; 63:60–7.
Article24. Rastan AJ, Lachmann N, Walther T, Doll N, Gradistanac T, Gommert JF, et al. Autopsy findings in patients on postcardiotomy extracorporeal membrane oxygenation (ECMO). Int J Artif Organs. 2006; 29:1121–31.
Article25. Sertic F, Chavez L, Diagne D, Richards T, Wald J, Acker M, et al. Predictors of in-hospital mortality and midterm outcomes of patients successfully weaned from venoarterial extracorporeal membrane oxygenation. J Thorac Cardiovasc Surg. 2021; 161:666–78.
Article26. Kohler K, Valchanov K, Nias G, Vuylsteke A. ECMO cannula review. Perfusion. 2013; 28:114–24.
Article27. Fraser KH, Zhang T, Taskin ME, Griffith BP, Wu ZJ. Computational fluid dynamics analysis of thrombosis potential in left ventricular assist device drainage cannulae. ASAIO J. 2010; 56:157–63.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Extracorporeal Membrane Oxygenation Cannula Malposition in the Azygos Vein in a Neonate with Right-Sided Congenital Diaphragmatic Hernia
- Fatal Left Ventricular Thrombosis in an Infant Receiving Extracorporeal Membrane Oxygenation Support: A Case Report
- Sequential Bilateral Lung Transplantation with Extracorporeal Membrane Oxygenation (ECMO) Support: A case report
- Extracorporeal Membrane Oxygenation Support for Dogs in Acute Respiratory Failure : Comparison of venovenous extracorporeal lung assist using a double lumen tube with venoarterial extracorporeal lung assist
- Cardiopulmonary resuscitation with assisted extracorporeal life support during cardiac arrest caused by drug-eluting stent thrombosis: a case report