Acute Crit Care.
2023 Aug;38(3):278-285. 10.4266/acc.2023.00514.
Factors influencing sleep quality in the intensive care unit: a descriptive pilot study in Korea
- Affiliations
-
- 1Department of Critical Care Medicine, Seoul National University Hospital, Seoul, Korea
- 2Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea
- KMID: 2547021
- DOI: http://doi.org/10.4266/acc.2023.00514
Abstract
- Background
As sleep disturbances are common in the intensive care unit (ICU), this study assessed the sleep quality in the ICU and identified barriers to sleep.
Methods
Patients admitted to the ICUs of a tertiary hospital between June 2022 and December 2022 who were not mechanically ventilated at enrollment were included. The quality of sleep (QoS) at home was assessed on a visual analog scale as part of an eight-item survey, while the QoS in the ICU was evaluated using the Korean version of the Richards-Campbell Sleep Questionnaire (K-RCSQ). Good QoS was defined by a score of ≥50.
Results
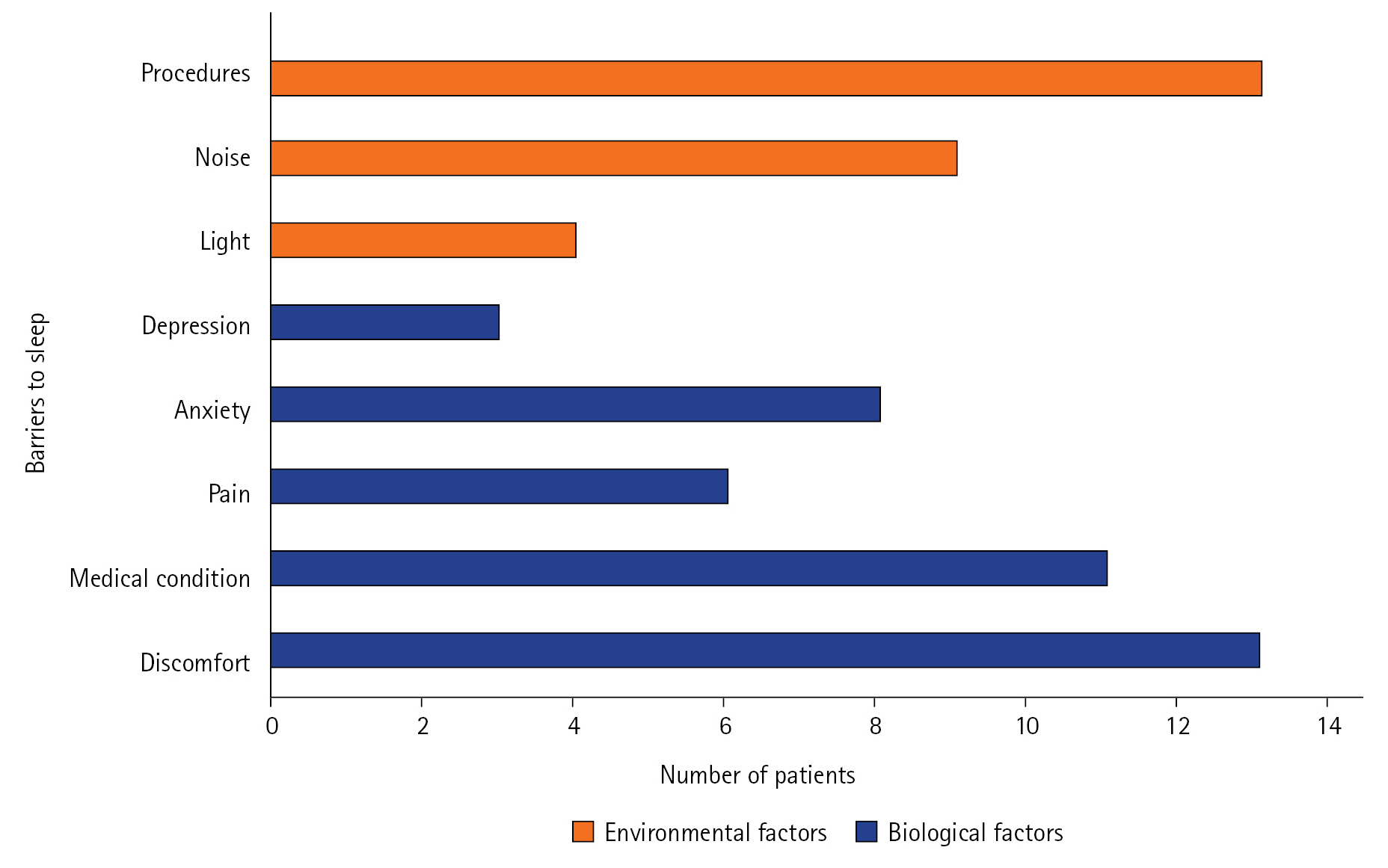
Of the 30 patients in the study, 19 reported a QoS score <50. The Spearman correlation coefficient showed no meaningful relationship between the QoS at home and the overall K-RCSQ QoS score in the ICU (r=0.16, P=0.40). The most common barriers to sleep were physical discomfort (43%), being awoken for procedures (43%), and feeling unwell (37%); environmental factors including noise (30%) and light (13%) were also identified sources of sleep disruption. Physical discomfort (median [interquartile range]: 32 [28.0–38.0] vs. 69 [42.0–80.0], P=0.004), being awoken for procedures (36 [20.0–48.0] vs. 54 [36.0–80.0], P=0.04), and feeling unwell (31 [18.0–42.0] vs. 54 [40.0–76.0], P=0.01) were associated with lower K-RCSQ scores.
Conclusions
In the ICU, physical discomfort, patient care interactions, and feeling unwell were identified as barriers to sleep.
Keyword
Figure
Cited by 1 articles
-
Could fever dreams influence sleep in intensive care units?
Jeng Swen Ng, Sheryn Tan, Sanjana Santhosh, Brandon Stretton, Joshua Kovoor, Aashray Gupta, Stephen Bacchi
Acute Crit Care. 2024;39(2):327-329. doi: 10.4266/acc.2023.01074.
Reference
-
1. Krueger JM, Rector DM, Roy S, Van Dongen HP, Belenky G, Panksepp J. Sleep as a fundamental property of neuronal assemblies. Nat Rev Neurosci. 2008; 9:910–9.
Article2. Krause AJ, Simon EB, Mander BA, Greer SM, Saletin JM, Goldstein-Piekarski AN, et al. The sleep-deprived human brain. Nat Rev Neurosci. 2017; 18:404–18.
Article3. Riemann D, Krone LB, Wulff K, Nissen C. Sleep, insomnia, and depression. Neuropsychopharmacology. 2020; 45:74–89.
Article4. Parthasarathy S, Vasquez MM, Halonen M, Bootzin R, Quan SF, Martinez FD, et al. Persistent insomnia is associated with mortality risk. Am J Med. 2015; 128:268–75.5. Figueroa-Ramos MI, Arroyo-Novoa CM, Lee KA, Padilla G, Puntillo KA. Sleep and delirium in ICU patients: a review of mechanisms and manifestations. Intensive Care Med. 2009; 35:781–95.
Article6. Pisani MA, D’Ambrosio C. Sleep and delirium in adults who are critically ill: a contemporary review. Chest. 2020; 157:977–84.
Article7. Telias I, Wilcox ME. Sleep and circadian rhythm in critical illness. Crit Care. 2019; 23:82.
Article8. Richards KC, O’Sullivan PS, Phillips RL. Measurement of sleep in critically ill patients. J Nurs Meas. 2000; 8:131–44.
Article9. Kim JK, Park JH, Cho J, Lee SM, Lee J. Reliability of the Korean version of the Richards-Campbell Sleep Questionnaire. Acute Crit Care. 2020; 35:164–8.
Article10. Haimovich B, Calvano J, Haimovich AD, Calvano SE, Coyle SM, Lowry SF. In vivo endotoxin synchronizes and suppresses clock gene expression in human peripheral blood leukocytes. Crit Care Med. 2010; 38:751–8.
Article11. Delaney LJ, Currie MJ, Huang HC, Lopez V, Van Haren F. “They can rest at home”: an observational study of patients’ quality of sleep in an Australian hospital. BMC Health Serv Res. 2018; 18:524.
Article12. Little A, Ethier C, Ayas N, Thanachayanont T, Jiang D, Mehta S. A patient survey of sleep quality in the intensive care unit. Minerva Anestesiol. 2012; 78:406–14.
Article13. Martinez FE, Poulter AL, Seneviratne C, Chrimes A, Havill K, Balogh ZJ, et al. ICU patients’ perception of sleep and modifiable versus non-modifiable factors that affect it: a prospective observational study. J Clin Med. 2022; 11:3725.
Article14. Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O’Neal PV, Keane KA, et al. The Richmond Agitation-Sedation Scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med. 2002; 166:1338–44.15. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983; 67:361–70.
Article16. Naik RD, Gupta K, Soneja M, Elavarasi A, Sreenivas V, Sinha S. Sleep quality and quantity in intensive care unit patients: a cross-sectional study. Indian J Crit Care Med. 2018; 22:408–14.
Article17. Locihová H, Axmann K, Žiaková K, Šerková D, Černochová S. Sleep quality assessment in intensive care: actigraphy vs. Richards-Campbell sleep questionnaire. Sleep Sci. 2020; 13:235–41.18. Julious SA. Sample size of 12 per group rule of thumb for a pilot study. Pharma Stat. 2005; 4:287–91.
Article19. Julious SA. Pilot studies in clinical research. Stat Methods Med Res. 2016; 25:995–6.
Article20. Billingham SA, Whitehead AL, Julious SA. An audit of sample sizes for pilot and feasibility trials being undertaken in the United Kingdom registered in the United Kingdom Clinical Research Network database. BMC Med Res Methodol. 2013; 13:104.
Article21. Stewart JA, Green C, Stewart J, Tiruvoipati R. Factors influencing quality of sleep among non-mechanically ventilated patients in the Intensive Care Unit. Aust Crit Care. 2017; 30:85–90.
Article22. Van Eijk M, Slooter A. Quality and quantity of sleep in multipatient versus single-room ICUs. Crit Care. 2012; 16(Suppl 1):P321.
Article23. Gabor JY, Cooper AB, Crombach SA, Lee B, Kadikar N, Bettger HE, et al. Contribution of the intensive care unit environment to sleep disruption in mechanically ventilated patients and healthy subjects. Am J Respir Crit Care Med. 2003; 167:708–15.
Article24. Darbyshire JL, Young JD. An investigation of sound levels on intensive care units with reference to the WHO guidelines. Crit Care. 2013; 17:R187.
Article25. Berglund B, Lindvall T, Schwela DH; World Health Organization. Guidelines for community noise. World Health Organization; 1999.26. Tegnestedt C, Günther A, Reichard A, Bjurström R, Alvarsson J, Martling CR, et al. Levels and sources of sound in the intensive care unit: an observational study of three room types. Acta Anaesthesiol Scand. 2013; 57:1041–50.
Article27. Blume C, Garbazza C, Spitschan M. Effects of light on human circadian rhythms, sleep and mood. Somnologie (Berl). 2019; 23:147–56.
Article28. Bihari S, Doug McEvoy R, Matheson E, Kim S, Woodman RJ, Bersten AD. Factors affecting sleep quality of patients in intensive care unit. J Clin Sleep Med. 2012; 8:301–7.
Article29. Parthasarathy S, Tobin MJ. Sleep in the intensive care unit. Intensive Care Med. 2004; 30:197–206.
Article30. Lu W, Fu Q, Luo X, Fu S, Hu K. Effects of dexmedetomidine on sleep quality of patients after surgery without mechanical ventilation in ICU. Medicine (Baltimore). 2017; 96:e7081.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A study on the sleep amount of patient and environmental factors influencing to the sleep amount in intensive care unit.
- The Optimal Dose of Midazolam for Promoting Sleep in Critically Ill Patients: A Pilot Study
- Factors Influencing on Quality of Sleep among Patients at Surgical Intensive Care Units
- Factors Influencing Sleep Quality in Nursing Students and non Nursing Students
- Influencing factors for Sleep Disturbance in the Intensive Care Unit Patients: A Systematic Review