Acute Crit Care.
2023 Aug;38(3):271-277. 10.4266/acc.2023.00591.
Awake prone positioning for COVID-19 acute hypoxemic respiratory failure in Tunisia
- Affiliations
-
- 1Medical Intensive Care Unit, Regional Hospital of Zaghouan and Faculty of Medicine of Tunis, University of Tunis El Manar, Zaghouan, Tunisia
- 2Research Unit for Respiratory Failure and Mechanical Ventilation UR22SP01, Abderrahmen Mami Hospital, Ministry of Higher Education and Scientific Research, Ariana, Tunisia
- KMID: 2547020
- DOI: http://doi.org/10.4266/acc.2023.00591
Abstract
- Background
In this study, we explored whether awake prone position (PP) can impact prognosis of severe hypoxemia coronavirus disease 2019 (COVID-19) patients.
Methods
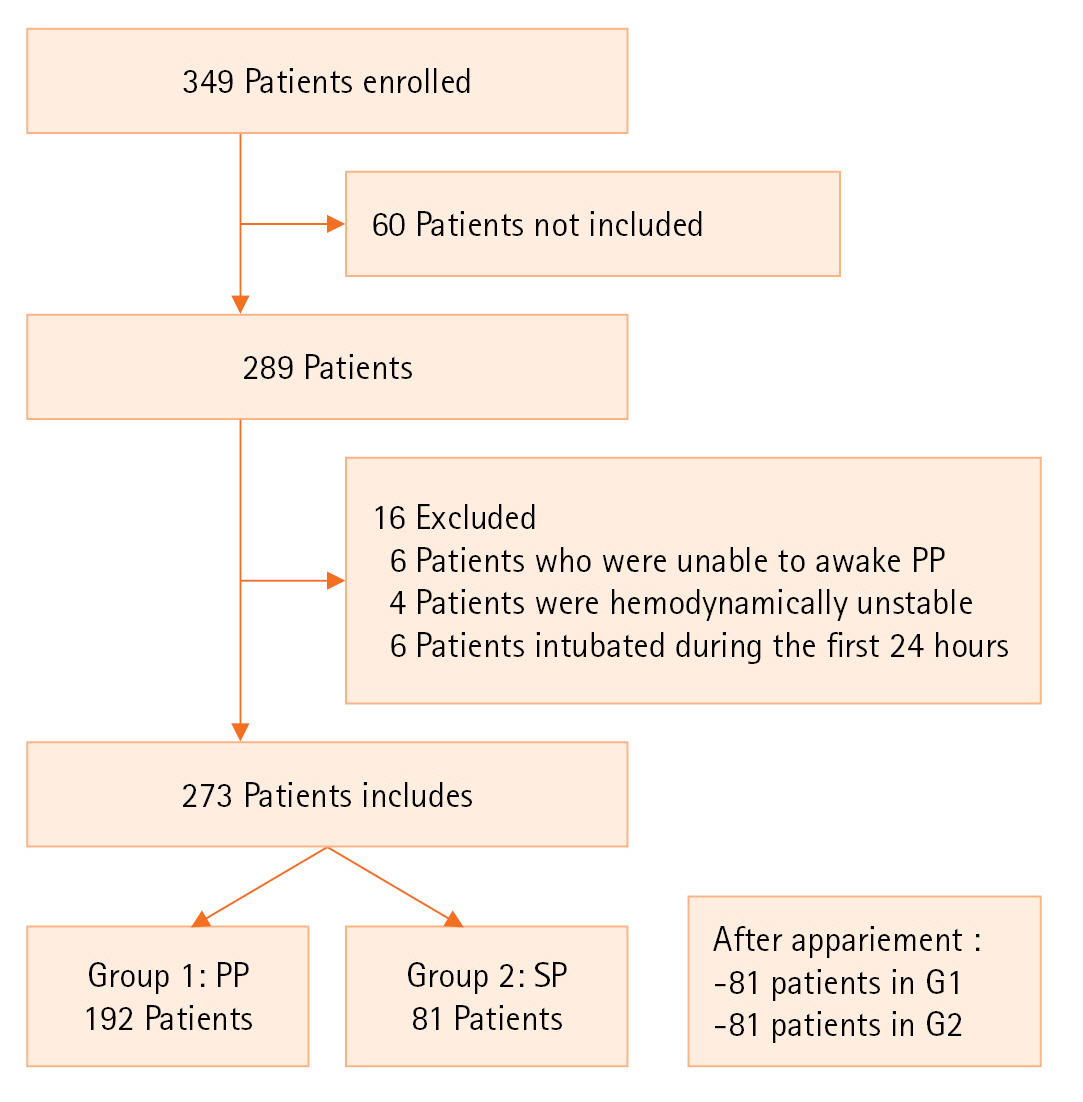
This was a prospective observational study of severe, critically ill adult COVID-19 patients admitted to the intensive care unit. Patients were divided into two groups: group G1, patients who benefited from a vigilant and effective PP (>4 hours minimum/24) and group G2, control group. We compared demographic, clinical, paraclinical and evolutionary data.
Results
Three hundred forty-nine patients were hospitalized during the study period, 273 met the inclusion criteria. PP was performed in 192 patients (70.3%). The two groups were comparable in terms of demographic characteristics, clinical severity and modalities of oxygenation at intensive care unit (ICU) admission. The mean PaO2/ FIO2 ratios were 141 and 128 mm Hg, respectively (P=0.07). The computed tomography scan was comparable with a critical >75% in 48.5% (G1) versus 54.2% (G2). The median duration of the daily PP session was 13±7 hours per day. The average duration of spontaneous PP days was 7 days (4–19). Use of invasive ventilation was lower in the G1 group (27% vs. 56%, P=0.002). Healthcare-associated infections were significantly lower in G1 (42.1% vs. 82%, P=0.01). Duration of total mechanical ventilation and length of ICU stay were comparable between the two groups. Mortality was significantly higher in G2 (64% vs. 28%, P=0.02).
Conclusions
Our study confirmed that awake PP can improve prognosis in COVID-19 patients. Randomized controlled trials are needed to confirm this result.
Figure
Reference
-
1. Li J, Luo J, Pavlov I, Perez Y, Tan W, Roca O, et al. Awake prone positioning for non-intubated patients with COVID-19-related acute hypoxaemic respiratory failure: a systematic review and meta-analysis. Lancet Respir Med. 2022; 10:573–83.2. Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013; 369:840–51.
Article3. Lopes JA, Jorge S. The RIFLE and AKIN classifications for acute kidney injury: a critical and comprehensive review. Clin Kidney J. 2013; 6:8–14.
Article4. Sikora A, Zahra F. Nosocomial infections [Internet]. StatPearls Publishing;2023. [cited 2023 Jun 1]. Available from: https://pubmed.ncbi.nlm.nih.gov/32644738/.5. Scaravilli V, Grasselli G, Castagna L, Zanella A, Isgrò S, Lucchini A, et al. Prone positioning improves oxygenation in spontaneously breathing nonintubated patients with hypoxemic acute respiratory failure: a retrospective study. J Crit Care. 2015; 30:1390–4.
Article6. Chalmers JD, Crichton ML, Goeminne PC, Cao B, Humbert M, Shteinberg M, et al. Management of hospitalised adults with coronavirus disease 2019 (COVID-19): European Respiratory Society living guideline. Eur Respir J. 2021; 57:2100048.7. Nasa P, Azoulay E, Khanna AK, Jain R, Gupta S, Javeri Y, et al. Expert consensus statements for the management of COVID-19-related acute respiratory failure using a Delphi method. Crit Care. 2021; 25:106.
Article8. Serpa Neto A, Checkley W, Sivakorn C, Hashmi M, Papali A, Schultz MJ, et al. Pragmatic recommendations for the management of acute respiratory failure and mechanical ventilation in patients with COVID-19 in low- and middle-income countries. Am J Trop Med Hyg. 2021; 104(3_Suppl):60–71.
Article9. Gattinoni L, Pesenti A. The concept of “baby lung”. Intensive Care Med. 2005; 31:776–84.
Article10. Gattinoni L, Pelosi P, Vitale G, Pesenti A, D'Andrea L, Mascheroni D. Body position changes redistribute lung computed-tomographic density in patients with acute respiratory failure. Anesthesiology. 1991; 74:15–23.
Article11. Bone RC. The ARDS lung. New insights from computed tomography. JAMA. 1993; 269:2134–5.
Article12. Albert RK, Leasa D, Sanderson M, Robertson HT, Hlastala MP. The prone position improves arterial oxygenation and reduces shunt in oleic-acid-induced acute lung injury. Am Rev Respir Dis. 1987; 135:628–33.13. Albert RK, Hubmayr RD. The prone position eliminates compression of the lungs by the heart. Am J Respir Crit Care Med. 2000; 161:1660–5.
Article14. Lamm WJ, Graham MM, Albert RK. Mechanism by which the prone position improves oxygenation in acute lung injury. Am J Respir Crit Care Med. 1994; 150:184–93.
Article15. Sartini C, Tresoldi M, Scarpellini P, Tettamanti A, Carcò F, Landoni G, et al. Respiratory parameters in patients with COVID-19 after using noninvasive ventilation in the prone position outside the intensive care unit. JAMA. 2020; 323:2338–40.
Article16. Coppo A, Bellani G, Winterton D, Di Pierro M, Soria A, Faverio P, et al. Feasibility and physiological effects of prone positioning in non-intubated patients with acute respiratory failure due to COVID-19 (PRON-COVID): a prospective cohort study. Lancet Respir Med. 2020; 8:765–74.17. Caputo ND, Strayer RJ, Levitan R. Early self-proning in awake, non-intubated patients in the emergency department: a single ED’s experience during the COVID-19 pandemic. Acad Emerg Med. 2020; 27:375–8.
Article18. Elharrar X, Trigui Y, Dols AM, Touchon F, Martinez S, Prud’homme E, et al. Use of prone positioning in nonintubated patients with COVID-19 and hypoxemic acute respiratory failure. JAMA. 2020; 323:2336–8.
Article19. Despres C, Brunin Y, Berthier F, Pili-Floury S, Besch G. Prone positioning combined with high-flow nasal or conventional oxygen therapy in severe COVID-19 patients. Crit Care. 2020; 24:256.
Article20. Paul V, Patel S, Royse M, Odish M, Malhotra A, Koenig S. Proning in non-intubated (PINI) in times of COVID-19: case series and a review. J Intensive Care Med. 2020; 35:818–24.
Article21. Chua EX, Zahir SM, Ng KT, Teoh WY, Hasan MS, Ruslan SR, et al. Effect of prone versus supine position in COVID-19 patients: a systematic review and meta-analysis. J Clin Anesth. 2021; 74:110406.
Article22. Bahloul M, Kharrat S, Hafdhi M, Maalla A, Turki O, Chtara K, et al. Impact of prone position on outcomes of COVID-19 patients with spontaneous breathing. Acute Crit Care. 2021; 36:208–14.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical characteristics and outcomes of critically ill COVID-19 patients in Sfax, Tunisia
- Gravity-induced ischemia in the brain and prone positioning for COVID-19 patients breathing spontaneously: still far from the truth!
- Treatment of Critically Ill Patients with Coronavirus Disease 2019
- Impact of prone position on outcomes of COVID-19 patients with spontaneous breathing
- Comparison of critically ill COVID-19 and influenza patients with acute respiratory failure