J Korean Med Sci.
2023 Oct;38(39):e323. 10.3346/jkms.2023.38.e323.
Toxocara canis and Fasciola hepatica Co-Infection Leading to Hepatic Abscess: A Case Report
- Affiliations
-
- 1Department of Internal Medicine, Keimyung University School of Medicine, Daegu, Korea
- KMID: 2546922
- DOI: http://doi.org/10.3346/jkms.2023.38.e323
Abstract
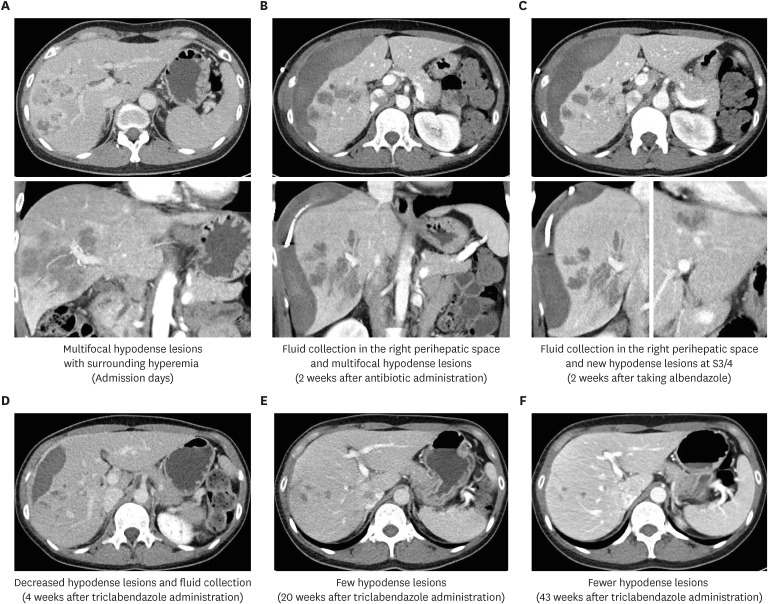
- Toxocariasis is a zoonotic disease caused by ingesting eggs from soil contaminated with Toxocara canis and Fasciola hepatica, commonly found in feces of infected dogs and cats, leading to a range of clinical symptoms including fever, abdominal pain and gastrointestinal manifestations. Fascioliasis is also a zoonotic disease caused by liver flukes Fasciola hepatica and Fasciola gigantica, which can be contracted through consumption of contaminated water or aquatic plants, leading to various clinical features. Here, we report a case of a 39-yearold woman diagnosed with a liver abscess caused by co-infection of T. canis and F. hepatica, as confirmed by serological tests. Although the existence of a pet dog and an experience of eating raw water dropwort are potential clues for diagnosis, it cannot be determined as the source of infection because the source of infection has not been clearly identified. After administrating albendazole and triclabendazole sequentially, the patient showed improvement in blood test and imaging findings. Clinicians should be aware of parasitic coinfection and take appropriate management.
Keyword
Figure
Reference
-
1. Magnaval JF, Glickman LT, Dorchies P, Morassin B. Highlights of human toxocariasis. Korean J Parasitol. 2001; 39(1):1–11. PMID: 11301585.2. Ma G, Holland CV, Wang T, Hofmann A, Fan CK, Maizels RM, et al. Human toxocariasis. Lancet Infect Dis. 2018; 18(1):e14–e24. PMID: 28781085.3. Peters L, Burkert S, Grüner B. Parasites of the liver - epidemiology, diagnosis and clinical management in the European context. J Hepatol. 2021; 75(1):202–218. PMID: 33636243.4. Pockros PJ, Capozza TA. Helminthic infections of the liver. Curr Gastroenterol Rep. 2004; 6(4):287–296. PMID: 15245696.5. Yoo JJ, Lee TK, Kyoung DS, Park MA, Kim SG, Kim YS. A population-based study of pyogenic liver abscess in Korea: incidence, mortality and temporal trends during 2007-2017. Liver Int. 2021; 41(11):2747–2758. PMID: 34396681.6. Park HJ, Choi GS, Jung M, Lee SU. Fasciola Hepatica induced hepatic abscess treated with triclabendazole. Korean J Gastroenterol. 2021; 77(1):39–44. PMID: 33495431.7. Jeong MJ, Park JK, Yu HS. Phylogenetic characteristics of Fasciola hepatica isolated from a Korean patient. Korean J Parasitol. 2022; 60(5):367–370. PMID: 36320115.8. Kim TY, Lee YS, Yun JH, Kim JJ, Choi WH, Oh IH, et al. A case of probable mixed-infection with Clonorchis sinensis and Fasciola sp.: CT and parasitological findings. Korean J Parasitol. 2010; 48(2):157–160. PMID: 20585533.9. Wang M, Liu W, Xiong Z, Li Z, Li J, Xu X, et al. Case report: “Area of Focus” atypical trichinellosis and fascioliasis coinfection. Front Med (Lausanne). 2022; 9:881356. PMID: 35646994.10. Jin Y, Shen C, Huh S, Sohn WM, Choi MH, Hong ST. Serodiagnosis of toxocariasis by ELISA using crude antigen of Toxocara canis larvae. Korean J Parasitol. 2013; 51(4):433–439. PMID: 24039286.11. Woodhall DM, Fiore AE. Toxocariasis: a review for pediatricians. J Pediatric Infect Dis Soc. 2014; 3(2):154–159. PMID: 26625368.12. Despommier D. Toxocariasis: clinical aspects, epidemiology, medical ecology, and molecular aspects. Clin Microbiol Rev. 2003; 16(2):265–272. PMID: 12692098.13. Mas-Coma S, Bargues MD, Valero MA. Diagnosis of human fascioliasis by stool and blood techniques: update for the present global scenario. Parasitology. 2014; 141(14):1918–1946. PMID: 25077569.14. Dusak A, Onur MR, Cicek M, Firat U, Ren T, Dogra VS. Radiological imaging features of Fasciola hepatica infection - a pictorial review. J Clin Imaging Sci. 2012; 2:2. PMID: 22347685.15. Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL. Harrison’s Principles of Internal Medicine. New York, NY, USA: McGraw-Hill Companies, Inc.;2005.16. Center for Disease Control and Prevention. Fasciola. Updated 2020. Accessed March 14, 2023. https://www.cdc.gov/parasites/fasciola/health_professionals/index.html#tx .17. Pan American Health Organization. Facioliasis. Updated 2023. Accessed March 14, 2023. https://www.paho.org/en/topics/fascioliasis .18. Kim HS, Jin Y, Choi MH, Kim JH, Lee YH, Yoon CH, et al. Significance of serum antibody test for toxocariasis in healthy healthcare examinees with eosinophilia in Seoul and Gyeongsangnam-do, Korea. J Korean Med Sci. 2014; 29(12):1618–1625. PMID: 25469060.19. Lee JY, Yang MH, Hwang JH, Kang M, Paeng JW, Yune S, et al. The prevalence of toxocariasis and diagnostic value of serologic tests in asymptomatic Korean adults. Allergy Asthma Immunol Res. 2015; 7(5):467–475. PMID: 26122506.20. Jacquier P, Gottstein B, Stingelin Y, Eckert J. Immunodiagnosis of toxocarosis in humans: evaluation of a new enzyme-linked immunosorbent assay kit. J Clin Microbiol. 1991; 29(9):1831–1835. PMID: 1774303.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Hepatic Abscess Caused by Toxocara
- Atypical Toxocara canis-Induced Hepatic Visceral Larva Migrans: Diagnostic Challenges and Literature Review
- Eosinophilic Myocarditis Associated with Visceral Larva Migrans Caused by Toxocara Canis Infection
- Study on Infectivity of Toxocara canis Eggs from Soil
- Fasciola Hepatica Induced Hepatic Abscess Treated with Triclabendazole