J Stroke.
2023 Sep;25(3):399-408. 10.5853/jos.2023.00318.
Anesthetic Management and Outcomes of Endovascular Treatment of Basilar Artery Occlusion: Results From the ATTENTION Registry
- Affiliations
-
- 1Department of Neurology, The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, University of Science and Technology of China, Hefei, China
- 2Department of Emergency, Xiangtan Central Hospital, Xiangtan, China
- 3Department of Neurology, Linyi People’s Hospital, Linyi, China
- 4Department of Neurology, Xiangyang No.1 People’s Hospital, Hubei University of Medicine, Xiangyang, China
- 5Department of Neurology, Zhangzhou Affiliated Hospital of Fujian Medical University, Zhangzhou, China
- 6Department of Neurology, Heze Municipal Hospital, Heze, Shandong, China
- 7Department of Neurology, Taihe County People’s Hospital, Fuyang, China
- 8Department of Neurology, Nanyang Central Hospital, Nanyang, China
- 9Department of Radiology, Boston Medical Center, Boston University School of Medicine, Boston, MA, USA
- 10Department of Neurology, Boston Medical Center, Boston University School of Medicine, Boston, MA, USA
- 11Department of Laboratory Medicine, The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, University of Science and Technology of China, Hefei, China
- 12Core Facility Center, The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, University of Science and Technology of China, Hefei, China
- KMID: 2546441
- DOI: http://doi.org/10.5853/jos.2023.00318
Abstract
- Background and Purpose
To examine the clinical and safety outcomes after endovascular treatment (EVT) for acute basilar artery occlusion (BAO) with different anesthetic modalities.
Methods
This was a retrospective analysis using data from the Endovascular Treatment for Acute Basilar Artery Occlusion (ATTENTION) registry. Patients were divided into two groups defined by anesthetic modality performed during EVT: general anesthesia (GA) or non-general anesthesia (non-GA). The association between anesthetic management and clinical outcomes was evaluated in a propensity score matched (PSM) cohort and an inverse probability of treatment weighting (IPTW) cohort to adjust for imbalances between the two groups.
Results
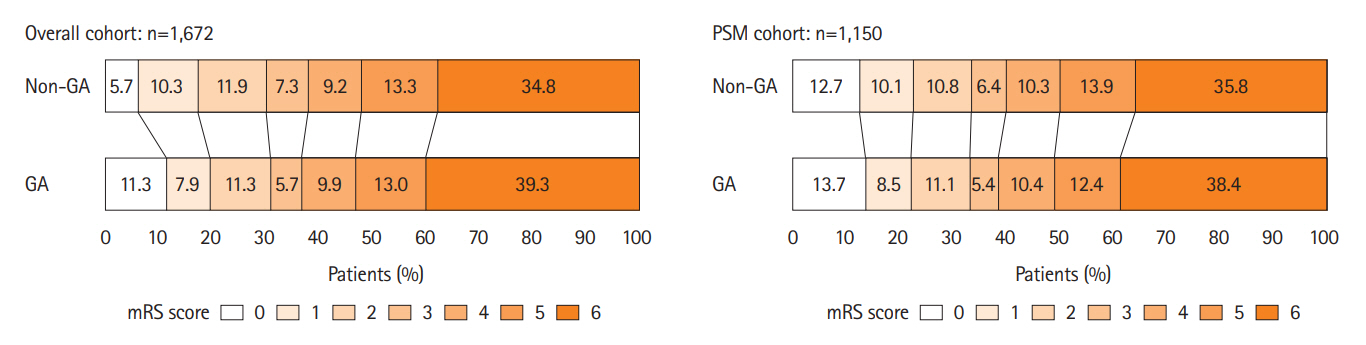
Our analytic sample included 1,672 patients from 48 centers. The anesthetic modality was GA in 769 (46.0%) and non-GA in 903 (54.0%) patients. In our primary analysis with the PSM-based cohort, non-GA was comparable to GA concerning the primary outcome (adjusted common odds ratio [acOR], 1.01; 95% confidence interval [CI], 0.82 to 1.25; P=0.91). Mortality at 90 days was 38.4% in the GA group and 35.8% in the non-GA group (adjusted risk ratio, 0.95; 95% CI, 0.83 to 1.08; P=0.44). In our secondary analysis with the IPTW-based cohort, the anesthetic modality was significantly associated with the distribution of modified Rankin Scale at 90 days (acOR: 1.45 [95% CI: 1.20 to 1.75]).
Conclusion
In this nationally-representative observational study, acute ischemic stroke patients due to BAO undergoing EVT without GA had similar clinical and safety outcomes compared with patients treated with GA. These findings provide the basis for large-scale randomized controlled trials to test whether anesthetic management provides meaningful clinical effects for patients undergoing EVT.
Figure
Reference
-
References
1. Li C, Wu C, Wu L, Zhao W, Chen J, Ren M, et al. Basilar Artery Occlusion Chinese Endovascular Trial: protocol for a prospective randomized controlled study. Int J Stroke. 2022; 17:694–697.2. Tao C, Li R, Zhu Y, Qun S, Xu P, Wang L, et al. Endovascular treatment for acute basilar artery occlusion: a multicenter randomized controlled trial (ATTENTION). Int J Stroke. 2022; 17:815–819.3. Goldhoorn RB, Bernsen MLE, Hofmeijer J, Martens JM, Lingsma HF, Dippel DWJ, et al. Anesthetic management during endovascular treatment of acute ischemic stroke in the MR CLEAN registry. Neurology. 2020; 94:e97–e106.4. Berkhemer OA, van den Berg LA, Fransen PS, Beumer D, Yoo AJ, Lingsma HF, et al. The effect of anesthetic management during intra-arterial therapy for acute stroke in MR CLEAN. Neurology. 2016; 87:656–664.5. Campbell BCV, van Zwam WH, Goyal M, Menon BK, Dippel DWJ, Demchuk AM, et al. Effect of general anaesthesia on functional outcome in patients with anterior circulation ischaemic stroke having endovascular thrombectomy versus standard care: a meta-analysis of individual patient data. Lancet Neurol. 2018; 17:47–53.6. Davis MJ, Menon BK, Baghirzada LB, Campos-Herrera CR, Goyal M, Hill MD, et al. Anesthetic management and outcome in patients during endovascular therapy for acute stroke. Anesthesiology. 2012; 116:396–405.7. Jumaa MA, Zhang F, Ruiz-Ares G, Gelzinis T, Malik AM, Aleu A, et al. Comparison of safety and clinical and radiographic outcomes in endovascular acute stroke therapy for proximal middle cerebral artery occlusion with intubation and general anesthesia versus the nonintubated state. Stroke. 2010; 41:1180–1184.8. Abou-Chebl A, Lin R, Hussain MS, Jovin TG, Levy EI, Liebeskind DS, et al. Conscious sedation versus general anesthesia during endovascular therapy for acute anterior circulation stroke: preliminary results from a retrospective, multicenter study. Stroke. 2010; 41:1175–1179.9. Taqi MA, Suriya SS, Sodhi A, Quadri SA, Farooqui M, Zafar A, et al. Ideal sedation for stroke thrombectomy: a prospective pilot single-center observational study. Neurosurg Focus. 2019; 46:E16.10. Brinjikji W, Pasternak J, Murad MH, Cloft HJ, Welch TL, Kallmes DF, et al. Anesthesia-related outcomes for endovascular stroke revascularization: a systematic review and meta-analysis. Stroke. 2017; 48:2784–2791.11. Schönenberger S, Uhlmann L, Hacke W, Schieber S, Mundiyanapurath S, Purrucker JC, et al. Effect of conscious sedation vs general anesthesia on early neurological improvement among patients with ischemic stroke undergoing endovascular thrombectomy: a randomized clinical trial. JAMA. 2016; 316:1986–1996.12. Simonsen CZ, Rasmussen M, Schönenberger S, Hendén PL, Bösel J, Valentin JB. General anesthesia during endovascular therapy for acute ischemic stroke: benefits beyond better reperfusion? J Neurointerv Surg. 2022; 14:767–771.13. Simonsen CZ, Yoo AJ, Sørensen LH, Juul N, Johnsen SP, Andersen G, et al. Effect of general anesthesia and conscious sedation during endovascular therapy on infarct growth and clinical outcomes in acute ischemic stroke: a randomized clinical trial. JAMA Neurol. 2018; 75:470–477.14. Schönenberger S, Hendén PL, Simonsen CZ, Uhlmann L, Klose C, Pfaff JAR, et al. Association of general anesthesia vs procedural sedation with functional outcome among patients with acute ischemic stroke undergoing thrombectomy: a systematic review and meta-analysis. JAMA. 2019; 322:1283–1293.15. Du H, Tong X, Sun X, Shi Z, Liu B, Gao F, et al. Effect of anesthesia strategy during endovascular therapy on 90-day outcomes in acute basilar artery occlusion: a retrospective observational study. BMC Neurol. 2020; 20:398.16. Skutecki J, Audibert G, Finitsis S, Consoli A, Lapergue B, Blanc R, et al. General anesthesia or conscious sedation for endovascular therapy of basilar artery occlusions: ETIS registry results. Rev Neurol (Paris). 2022; 178:771–779.17. Li F, Wan J, Song J, Yuan J, Kong W, Huang J, et al. Impact of anesthetic strategy on outcomes for patients with acute basilar artery occlusion undergoing mechanical thrombectomy. J Neurointerv Surg. 2022; 14:1073–1076.18. Terceño M, Silva Y, Bashir S, Vera-Monge VA, Cardona P, Molina C, et al. Impact of general anesthesia on posterior circulation large vessel occlusions after endovascular thrombectomy. Int J Stroke. 2021; 16:792–797.19. Jadhav AP, Bouslama M, Aghaebrahim A, Rebello LC, Starr MT, Haussen DC, et al. Monitored anesthesia care vs intubation for vertebrobasilar stroke endovascular therapy. JAMA Neurol. 2017; 74:704–709.20. Weyland CS, Chen M, Potreck A, Jäger LB, Seker F, Schönenberger S, et al. Sedation mode during endovascular stroke treatment in the posterior circulation—is conscious sedation for eligible patients feasible? Front Neurol. 2021; 12:711558.21. Wu L, Jadhav AP, Chen J, Sun C, Ji K, Li W, et al. Local anesthesia vs general anesthesia during endovascular therapy for acute posterior circulation stroke. J Neurol Sci. 2020; 416:117045.22. Hu G, Shi Z, Li B, Shao W, Xu B. General anesthesia versus monitored anesthesia care during endovascular therapy for vertebrobasilar stroke. Am J Transl Res. 2021; 13:1558–1567.23. Liang F, Wu Y, Wang X, Yan L, Zhang S, Jian M, et al. General anesthesia vs conscious sedation for endovascular treatment in patients with posterior circulation acute ischemic stroke: an exploratory randomized clinical trial. JAMA Neurol. 2023; 80:64–72.24. Tao C, Qureshi AI, Yin Y, Li J, Li R, Xu P, et al. Endovascular treatment versus best medical management in acute basilar artery occlusion strokes: results from the ATTENTION multicenter registry. Circulation. 2022; 146:6–17.25. Zaidat OO, Yoo AJ, Khatri P, Tomsick TA, von Kummer R, Saver JL, et al. Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke. 2013; 44:2650–2663.26. von Kummer R, Broderick JP, Campbell BC, Demchuk A, Goyal M, Hill MD, et al. The Heidelberg Bleeding Classification: classification of bleeding events after ischemic stroke and reperfusion therapy. Stroke. 2015; 46:2981–2986.27. Faraone SV. Interpreting estimates of treatment effects: implications for managed care. P T. 2008; 33:700–711.28. Rubin DB. Multiple imputation for nonresponse in surveys. New York: Wiley;1987.29. Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011; 46:399–424.30. Naimi AI, Whitcomb BW. Estimating risk ratios and risk differences using regression. Am J Epidemiol. 2020; 189:508–510.31. Funk MJ, Westreich D, Wiesen C, Stürmer T, Brookhart MA, Davidian M. Doubly robust estimation of causal effects. Am J Epidemiol. 2011; 173:761–767.32. Wagner B, Lorscheider J, Wiencierz A, Blackham K, Psychogios M, Bolliger D, et al. Endovascular treatment for acute ischemic stroke with or without general anesthesia: a matched comparison. Stroke. 2022; 53:1520–1529.33. Dhillon PS, Butt W, Podlasek A, McConachie N, Lenthall R, Nair S, et al. Association between anesthesia modality and clinical outcomes following endovascular stroke treatment in the extended time window. J Neurointerv Surg. 2023; 15:478–482.34. van den Berg LA, Koelman DL, Berkhemer OA, Rozeman AD, Fransen PS, Beumer D, et al. Type of anesthesia and differences in clinical outcome after intra-arterial treatment for ischemic stroke. Stroke. 2015; 46:1257–1262.35. Abou-Chebl A, Zaidat OO, Castonguay AC, Gupta R, Sun CH, Martin CO, et al. North American SOLITAIRE stent-retriever acute stroke registry: choice of anesthesia and outcomes. Stroke. 2014; 45:1396–1401.36. Nguyen TN, Abdalkader M, Jovin TG, Nogueira RG, Jadhav AP, Haussen DC, et al. Mechanical thrombectomy in the era of the COVID-19 pandemic: emergency preparedness for neuroscience teams: a guidance statement from the Society of Vascular and Interventional Neurology. Stroke. 2020; 51:1896–1901.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fusiform “True” Posterior Communicating Artery Aneurysm with Basilar Artery Occlusion: A Case Report
- Locked-in Syndrome Performed Endovascular Treatment for Vertebral Artery Dissection and Basilar Artery Occlusion Caused by a Golf Swing
- Giant fusiform aneurysm at the basilar trunk treated with endovascular coil occlusion following bypass surgery for the flow diversion
- Endovascular Treatment of Giant Basilar Trunk Aneurysm: Case Report
- Impact of Onset-to-Door Time on Endovascular Therapy for Basilar Artery Occlusion