J Korean Med Sci.
2023 Sep;38(37):e279. 10.3346/jkms.2023.38.e279.
Clinical Characteristics of Gynecologic Problems During Childhood in the Korean Population
- Affiliations
-
- 1Department of Obstetrics & Gynecology, Samsung Medical Center, Sungkyunkwan University of Medicine, Seoul, Korea
- KMID: 2546198
- DOI: http://doi.org/10.3346/jkms.2023.38.e279
Abstract
- Background
This study analyzed common gynecologic problems among Korean patients younger than ten years.
Methods
We performed a retrospective analysis of medical records of patients younger than ten years who visited the Pediatric and Adolescent Gynecology Clinic at Samsung Medical Center between 1995 and 2020.
Results
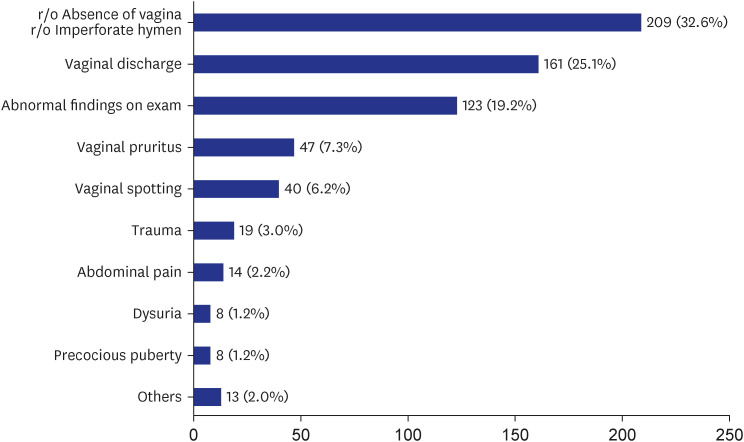
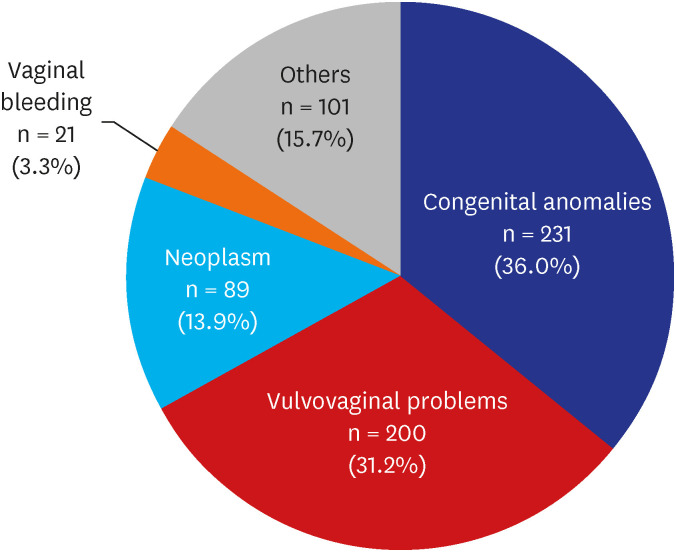
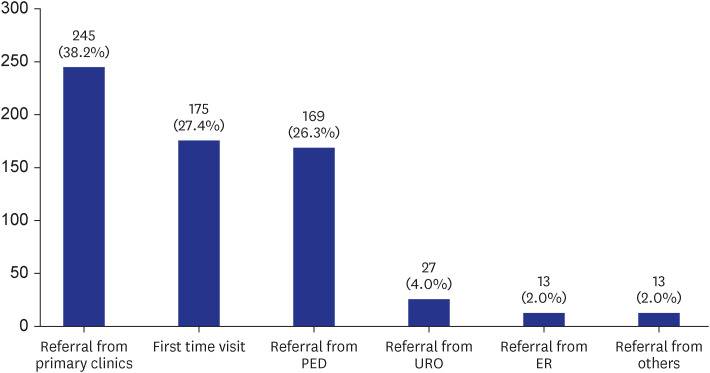
Among the 6,605 patients who visited the Pediatric and Adolescent Gynecology Clinic, data from 642 patients younger than ten years were analyzed in this study. The most common chief complaint was genital anomalies, followed by increased vaginal discharge and abnormal findings on clinical examinations. The most common disease entity was agglutination of the labia minora, which was commonly discovered incidentally during routine screenings. Vulvovaginitis, the second most common disease, was identified by symptoms of vaginal discharge, pruritus, and vaginal spotting. Neoplasm, issues with vaginal bleeding, and “other causes” were additional categories of gynecologic problems. 245 patients (38.2%) were referred from primary care sources, 175 patients (27.4%) sought care directly at the clinic, 169 patients (26.3%) were referrals from the institution’s pediatric department, and the remainder were referrals from other departments.
Conclusion
This study provides information about the gynecologic problems most frequently encountered in pediatric patients. The study provides helpful insight for primary care physicians into the proper management and timing of referrals for these gynecologic problems of pediatric patients.
Keyword
Figure
Reference
-
1. World Health Organization. Adolescent Health. Updated 2023. Accessed May 9, 2023. https://www.who.int/health-topics/adolescent-health#tab=tab_1 .2. Williams CE, Creighton SM. Menstrual disorders in adolescents: review of current practice. Horm Res Paediatr. 2012; 78(3):135–143. PMID: 23051587.
Article3. Seo MY, Kim SH, Juul A, Park MJ. Trend of menarcheal age among Korean girls. J Korean Med Sci. 2020; 35(49):e406. PMID: 33350182.
Article4. Bacon JL, Romano ME, Quint EH. Clinical recommendation: labial adhesions. J Pediatr Adolesc Gynecol. 2015; 28(5):405–409. PMID: 26162697.
Article5. Kass-Wolff JH, Wilson EE. Pediatric gynecology: assessment strategies and common problems. Semin Reprod Med. 2003; 21(4):329–338. PMID: 14724766.
Article6. Melek E, Kılıçbay F, Sarıkaş NG, Bayazıt AK. Labial adhesion and urinary tract problems: The importance of genital examination. J Pediatr Urol. 2016; 12(2):111.e1–111.e5.
Article7. Loveless M, Myint O. Vulvovaginitis- presentation of more common problems in pediatric and adolescent gynecology. Best Pract Res Clin Obstet Gynaecol. 2018; 48:14–27. PMID: 28927766.
Article8. McCaskill A, Inabinet CF, Tomlin K, Burgis J. Prepubertal genital bleeding: examination and differential diagnosis in pediatric female patients. J Emerg Med. 2018; 55(4):e97–100. PMID: 30170834.
Article9. Heo SH, Kim JW, Shin SS, Jeong SI, Lim HS, Choi YD, et al. Review of ovarian tumors in children and adolescents: radiologic-pathologic correlation. Radiographics. 2014; 34(7):2039–2055. PMID: 25384300.
Article10. Casey JT, Bjurlin MA, Cheng EY. Pediatric genital injury: an analysis of the National Electronic Injury Surveillance System. Urology. 2013; 82(5):1125–1130. PMID: 23953603.
Article11. Fan SM, Grigorian A, Chaudhry HH, Allen A, Sun B, Jasperse N, et al. Female pediatric and adolescent genitalia trauma: a retrospective analysis of the National Trauma Data Bank. Pediatr Surg Int. 2020; 36(10):1235–1241. PMID: 32851470.
Article12. Jang SY, Seo SR, Park SW, Kim DK. The Prevalence of marfan syndrome in Korea. J Korean Med Sci. 2017; 32(4):576–580. PMID: 28244281.
Article13. Lee DY, Hyun HS, Huh R, Jin DK, Kim DK, Yoon BK, et al. Estrogen-mediated height control in girls with marfan syndrome. J Korean Med Sci. 2016; 31(2):275–279. PMID: 26839483.
Article14. Kim SE, Lee DY, Kim MS, Cho SY, Jin DK, Choi D. Appropriate age for height control treatment in patients with marfan syndrome. Front Endocrinol (Lausanne). 2021; 12:708931. PMID: 34744997.
Article15. McGreal S, Wood PL. A study of paediatric and adolescent gynaecology services in a British district general hospital. BJOG. 2010; 117(13):1643–1650. PMID: 21078058.
Article16. Bedei I, Bumbuliene Z, Sirakov M, Mahmood T, Wood PL. European Association of Paediatric and Adolescent Gynaecology. Provision of paediatric and adolescent gynaecology in Europe today: A joint review by the European Association of Paediatric and Adolescent Gynaecology (EURAPAG) and European Board and College of Obstetrics and Gynaecology (EBCOG). Eur J Obstet Gynecol Reprod Biol. 2019; 235:116–120. PMID: 30826159.
Article17. Stankovic ZB, Tridenti G, Liassides M, Wood PL, Roos EJ. European Association of Paediatric and Adolescent Gynaecology (EURAPAG) and European Board And College of Obstetrics and Gynaecology (EBCOG). The future of paediatric and adolescent gynaecology in Europe. Eur J Obstet Gynecol Reprod Biol. 2019; 235:121–124. PMID: 30361166.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Gynecologic Disorders in the Older Adults
- A new perspective on cholesterol in pediatric health: association of vitamin D metabolism, respiratory diseases, and mental health problems
- Recommendations of Pharmacological Treatment inChildhood and Adolescents Obesity
- Parental Survey for Children with Feeding Problems
- A Case Report of a Child who has Attention Deficit Hyperactivity Disorder, Mental Retardation, and Mania