J Cerebrovasc Endovasc Neurosurg.
2023 Sep;25(3):288-296. 10.7461/jcen.2023.E2022.11.005.
The impact of collateral status on cerebral vasospasm and delayed cerebral ischemia in subarachnoid hemorrhage
- Affiliations
-
- 1Department of Neurosurgery, Adnan Menderes University Faculty of Medicine, Aydın, Tükiye
- 2Department of Neurology, Adnan Menderes University Faculty of Medicine, Aydın, Tükiye
- 3Department of Neurosurgery, Soonchunhyang University College of Medicine, Bucheon, Korea
- KMID: 2546165
- DOI: http://doi.org/10.7461/jcen.2023.E2022.11.005
Abstract
Objective
Cerebral collateral circulation may affect subarachnoid hemorrhage (SAH) induced cerebral vasospasm and delayed cerebral ischemia. In this study our aim was to investigate the relationship between collateral status, vasospasm and delayed cerebral ischemia (DCI) in both aneurysmal and nonaneurysmal SAH.
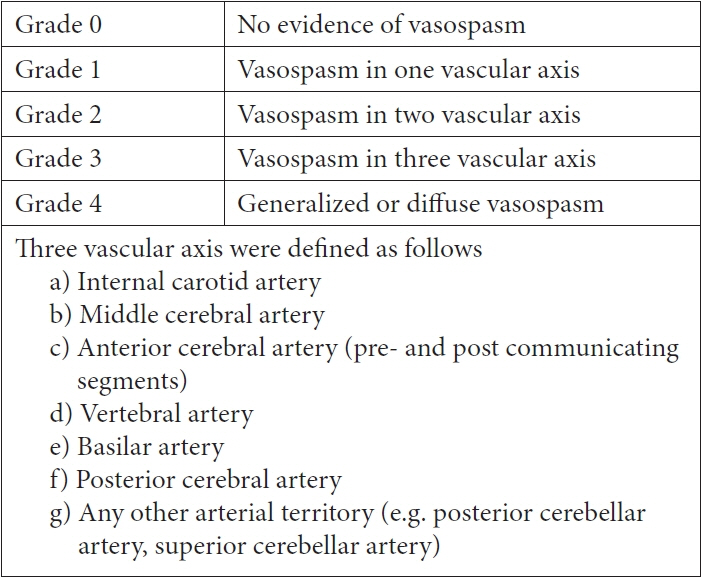
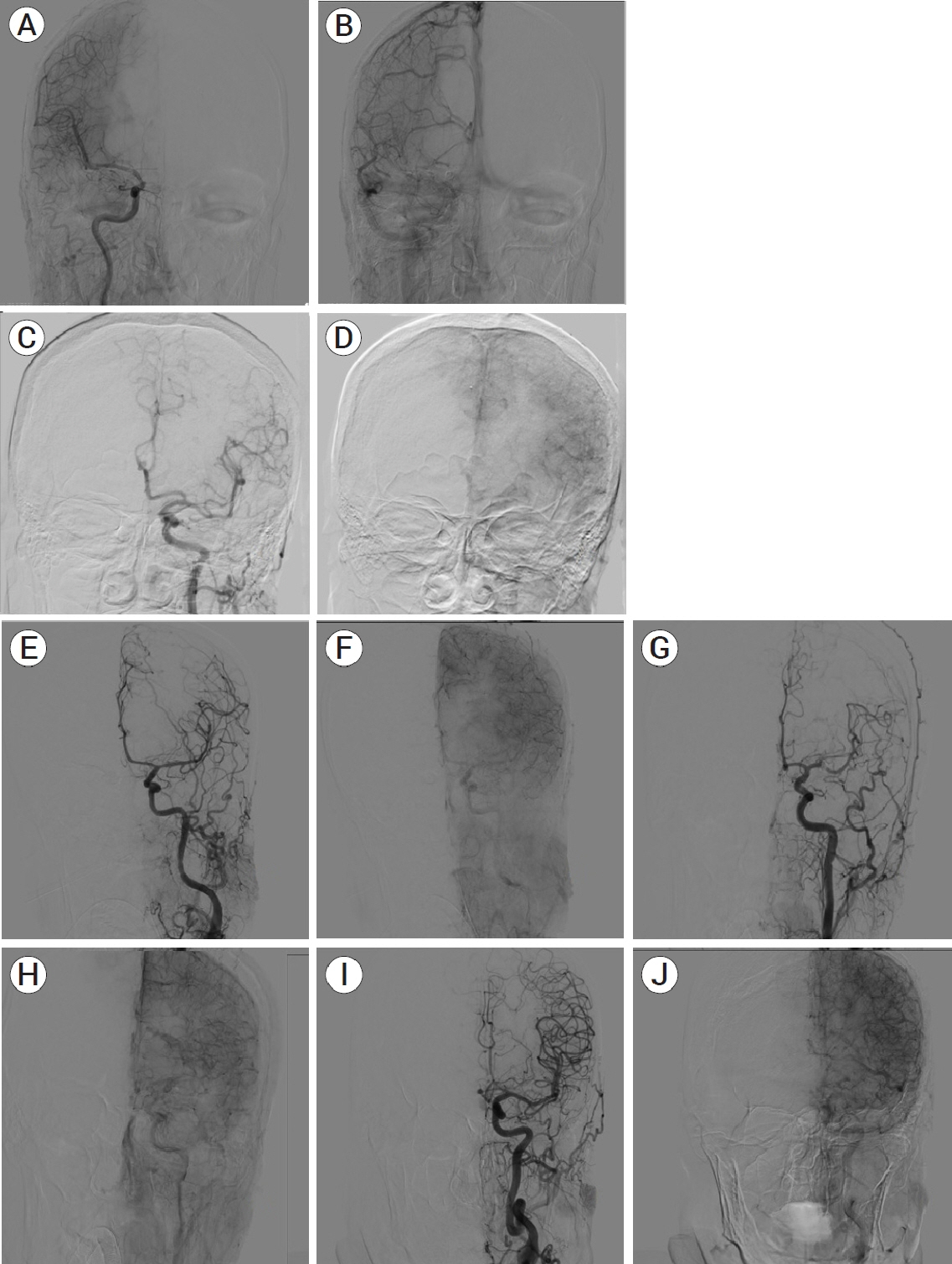
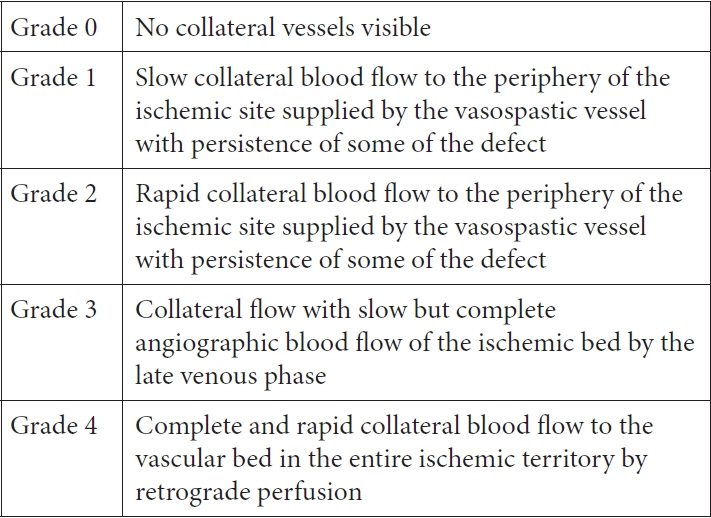
Methods
Patients diagnosed as SAH with and without aneurysm were included and their data investigated retrospectively. After the patients diagnosed as SAH according to cerebral computed tomography (CT)/magnetic resonance imaging (MRI), they underwent cerebral angiography to check for cerebral aneurysm. The diagnosis of DCI was made according to the neurological examination and control CT/MRI. All the patients had their control cerebral angiography on days 7 to 10 in order to assess vasospasm and also collateral circulation. The American Society of Interventional and Therapeutic Neuroradiology/Society of Interventional Radiology (ASITN/SIR) Collateral Flow Grading System was modified to measure collateral circulation.
Results
A total of 59 patients data were analyzed. Patients with aneurysmal SAH had higher Fisher scores and DCI was more common. Although there was no statistically significant difference between the patients with and without DCI in terms of demographics and mortality, patients with DCI had worse collateral circulation and more severe vasospasm. These patients had higher Fisher scores and more cerebral aneurysm overall.
Conclusions
According to our data, patients with higher Fisher scores, more severe vasospasm, and poor cerebral collateral circulation may experience DCI more frequently. Additionally aneurysmal SAH had higher Fisher scores and DCI was seen more common. To improve the clinical results for SAH patients, we believe that physicians should be aware of the DCI risk factors.
Keyword
Figure
Reference
-
1. Al-Mufti F, Witsch J, Manning N, Crimmins M, Amuluru K, Agarwal S, Park S, et al. Severity of cerebral vasospasm associated with development of collaterals following aneurysmal subarachnoid hemorrhage. J Neurointerv Surg. 2018; Jul. 10(7):638–43.2. Burrell C, Avalon NE, Siegel J, Pizzi M, Dutta T, Charlesworth MC, et al. Precision medicine of aneurysmal subarachnoid hemorrhage, vasospasm and delayed cerebral ischemia. Expert Rev Neurother. 2016; Nov. 16(11):1251–62.3. Cahill J, Zhang JH. Pre-vasospasm: Early brain injury. Acta Neurochir Suppl. 2008; 104:7–10.4. Connolly ES Jr, Rabinstein AA, Carhuapoma JR, Derdeyn CP, Dion J, Higashida RT, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2012; Jun. 43(6):1711–37.5. Doczi TP. Impact of cerebral microcirculatory changes on cerebral blood flow during cerebral vasospasm after aneurysmal subarachnoid hemorrhage. Stroke. 2001; 32(3):817.6. Dorsch NW. Cerebral arterial spasm–A clinical review. Br J Neurosurg. 1995; 9(3):403–12.7. Endo S, Branson PJ, Alksne JF. Experimental model of symptomatic vasospasm in rabbits. Stroke. 1988; Nov. 19(11):1420–5.8. Friedrich V, Flores R, Muller A, Sehba FA. Escape of intraluminal platelets into brain parenchyma after subarachnoid hemorrhage. Neuroscience. 2010; Feb. 165(3):968–75.9. Higashida RT, Furlan AJ, Roberts H, Tomsick T, Connors B, Barr J, et al. Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke. 2003; Aug. 34(8):e109–37.10. Jansen IGH, Berkhemer OA, Yoo AJ, Vos JA, Lycklama À Nijeholt GJ, Sprengers MES, et al. Comparison of CTA- and DSA-based collateral flow assessment in patients with anterior circulation stroke. AJNR Am J Neuroradiol. 2016; Nov. 37(11):2037–42.11. Kidd VJ. Proteolytic activities that mediate apoptosis. Annu Rev Physiol. 1998; 60:533–73.12. Kole MJ, Shea P, Albrecht JS, Cannarsa GJ, Wessell AP, Miller TR, et al. Utility of the Hsum score in predicting risk of aneurysm in patients with subarachnoid hemijdra orrhage: A single-center experience with 550 patients. Neurosurgery. 2020; Jun. 86(6):783–91.13. Konczalla J, Platz J, Schuss P, Vatter H, Seifert V, Güresir E. Non-aneurysmal non-traumatic subarachnoid hemorrhage: Patient characteristics, clinical outcome and prognostic factors based on a single-center experience in 125 patients. BMC Neurol. 2014; Jul. 14:140.14. Kumar G, Alexandrov AV. Vasospasm surveillance with transcranial doppler sonography in subarachnoid hemorrhage. J Ultrasound Med. 2015; Aug. 34(8):1345–50.15. Kumar G, Dumitrascu OM, Chiang CC, O’Carroll CB, Alexandrov AV. Prediction of delayed cerebral ischemia with cerebral angiography: A meta-analysis. Neurocrit Care. 2019; Feb. 30(1):62–71.16. Macdonald RL, Higashida RT, Keller E, Mayer SA, Molyneux A, Raabe A, et al. Clazosentan, an endothelin receptor antagonist, in patients with aneurysmal subarachnoid haemorrhage undergoing surgical clipping: A randomised, double-blind, placebo-controlled phase 3 trial (CONSCIOUS-2). Lancet Neurol. 2011; Jul. 10(7):618–25.17. Macdonald RL, Higashida RT, Keller E, Mayer SA, Molyneux A, Raabe A, et al. Randomized trial of clazosentan in patients with aneurysmal subarachnoid hemorrhage undergoing endovascular coiling. Stroke. 2012; Jun. 43(6):1463–9.18. Moftakhar P, Cooke DL, Fullerton HJ, Ko NU, Amans MR, Narvid JA, et al. Extent of collateralization predicting symptomatic cerebral vasospasm among pediatric patients: Correlations among angiography, transcranial Doppler ultrasonography, and clinical findings. J Neurosurg Pediatr. 2015; Mar. 15(3):282–90.19. Nathal E, Loopez-Gonza´lez F, Rios C. Angiographic scale for evaluation of cerebral vasospasm. Acta Neurochir Suppl. 2008; 104:225–8.20. Orakcioglu B, Fiebach JB, Steiner T, Kollmar R, Jüttler E, Becker K, et al. Evolution of early perihemorrhagic changes – ischemia vs. edema: An MRI study in rats. Exp Neurol. 2005; Jun. 193(2):369–76.21. Ostrowski RP, Colohan AR, Zhang JH. Mechanisms of hyperbaric oxygen-induced neuroprotection in a rat model of subarachnoid hemorrhage. J Cereb Blood Flow Metab. 2005; May. 25(5):554–71.22. Park S, Yamaguchi M, Zhou C, Calvert JW, Tang J, Zhang JH. Neurovascular protection reduces early brain injury after subarachnoid hemorrhage. Stroke. 2004; Oct. 35(10):2412–7.23. Peerless SJ, Fox AJ, Komatsu K, Hunter IG. Angiographic study of vasospasm following subarachnoid hemorrhage in monkeys. Stroke. 1982; Jul-Aug. 13(4):473–9.24. Philchenkov A. Caspases: Potential targets for regulating cell death. J Cell Mol Med. 2004; Oct-Dec. 8(4):432–44.25. Tsermoulas G, Flett L, Gregson B, Mitchell P. Immediate coma and poor outcome in subarachnoid haemorrhage are independently associated with an aneurysmal origin. Clin Neurol Neurosurg. 2013; Aug. 115(8):1362–5.26. van Loo G, Saelens X, van Gurp M, MacFarlane M, Martin SJ, Vandenabeele P. The role of mitochondrial factors in apoptosis: A Russian roulette with more than one bullet. Cell Death Differ. 2002; Oct. 9(10):1031–42.27. Vergouwen MD, Vermeulen M, van Gijn J, Rinkel GJ, Wijdicks EF, Muizelaar JP, et al. Definition of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage as an outcome event in clinical trials and observational studies: Proposal of a multidisciplinary research group. Stroke. 2010; Oct. 41(10):2391–5.28. Wartenberg KE. Update on the management of subarachnoid hemorrhage. Future Neurology. 2013; 8(2):205–24.29. Yilmaz A, Ozkul A. Demographic and clinical features of subarachnoid hemorrhages with and without cerebral aneurysm. Turkish Journal of Cerebrovascular Diseases. 2017; 23(2):56–61.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relation between Thromboembolism and Delayed Ischemic Neurological Deficits in Aneurysmal Subarachnoid Hemorrhage
- Transcranial Doppler Monitoring in Subarachnoid Hemorrhage
- Thromboembolism: Another substantial cause of delayed ischemic neurologic deficits after aneurysmal subarachnoid hemorrhage
- The Relationship Between CT Findings and Cerebral Vasospasm in Cerebral Aneursms
- Effects of Antiplatelet Agents on Cerebral Vasospasm and Delayed Cerebral Ischemia in Aneurysmal Subarachnoid Hemorrhage Patients Treated with Coil Embolization