Clin Endosc.
2023 Sep;56(5):633-649. 10.5946/ce.2022.201.
Evaluation of the mechanical properties of current biliary self-expandable metallic stents: axial and radial force, and axial force zero border
- Affiliations
-
- 1Department of Gastroenterology, Graduate School of Medicine, Juntendo University, Tokyo, Japan
- 2Department of Hepato-Biliary-Pancreatic Medicine, Cancer Institute Hospital of Japanese Foundation for Cancer Research, Tokyo, Japan
- 3Department of Gastroenterology, Graduate School of Medicine, The University of Tokyo, Tokyo, Japan
- 4Department of Endoscopy and Endoscopic Surgery, Graduate School of Medicine, The University of Tokyo, Tokyo, Japan
- 5Medical Laboratory, Research & Development Center, Zeon Corporation, Toyama, Japan
- KMID: 2546142
- DOI: http://doi.org/10.5946/ce.2022.201
Abstract
- Background/Aims
Mechanical properties (MPs) and axial and radial force (AF and RF) may influence the efficacy and complications of self-expandable metallic stent (SEMS) placement. We measured the MPs of various SEMSs and examined their influence on the SEMS clinical ability.
Methods
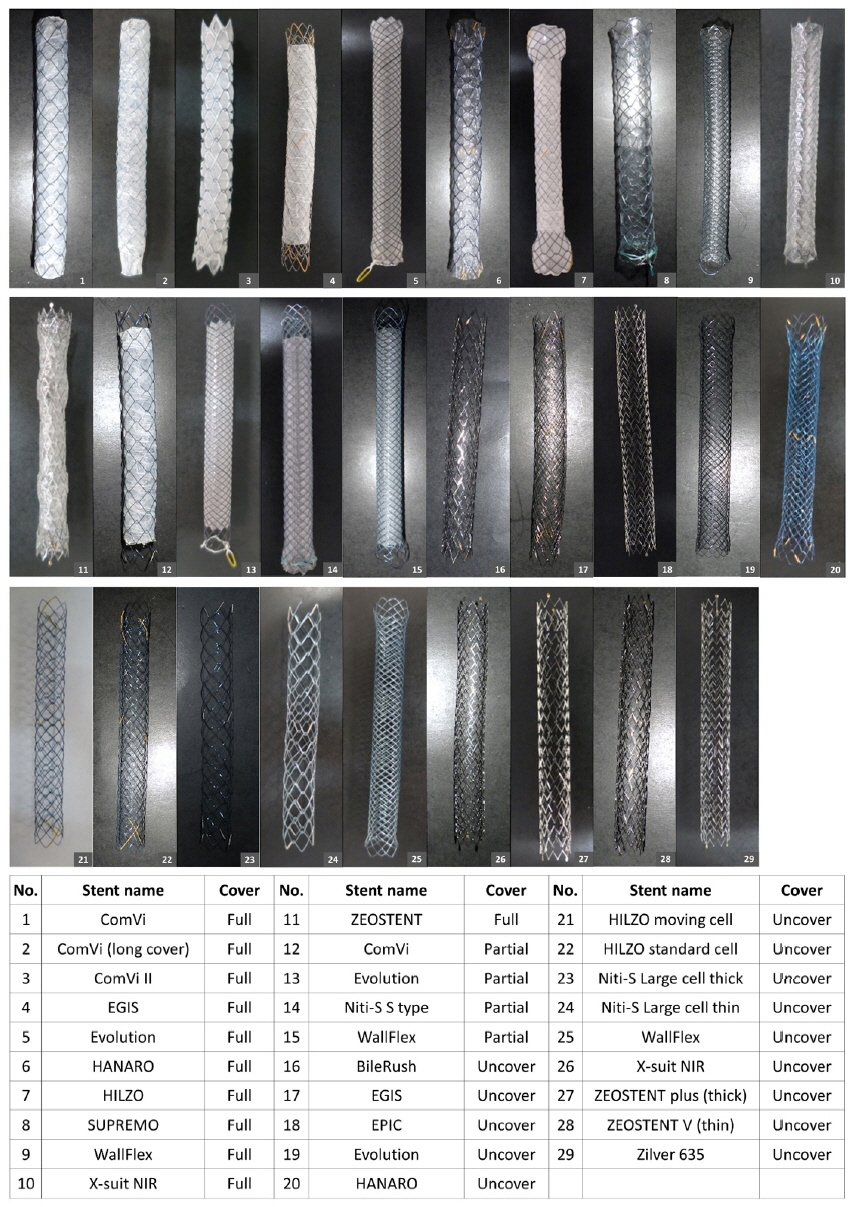
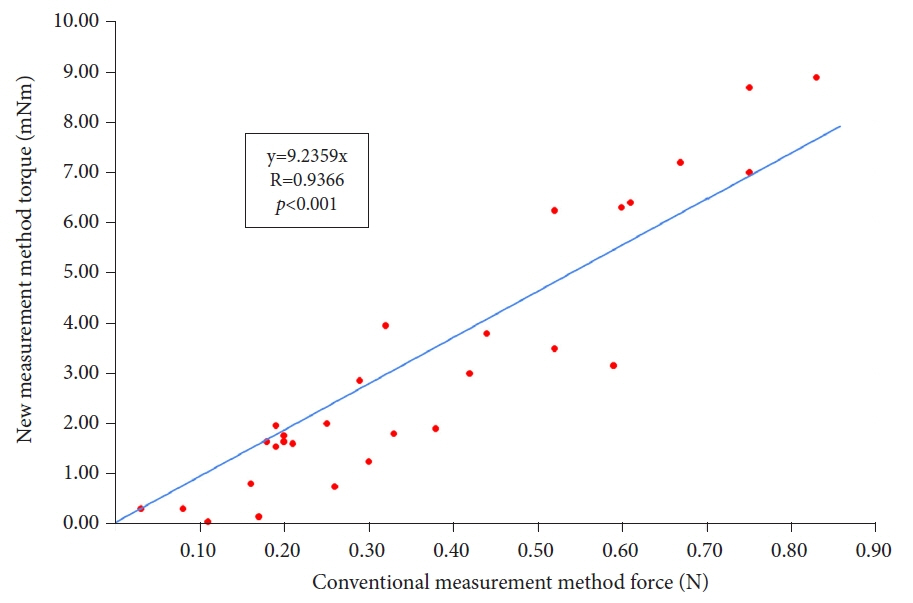
We evaluated the MPs of 29 types of 10-mm SEMSs. RF was measured using a conventional measurement device. AF was measured using the conventional and new methods, and the correlation between the methods was evaluated.
Results
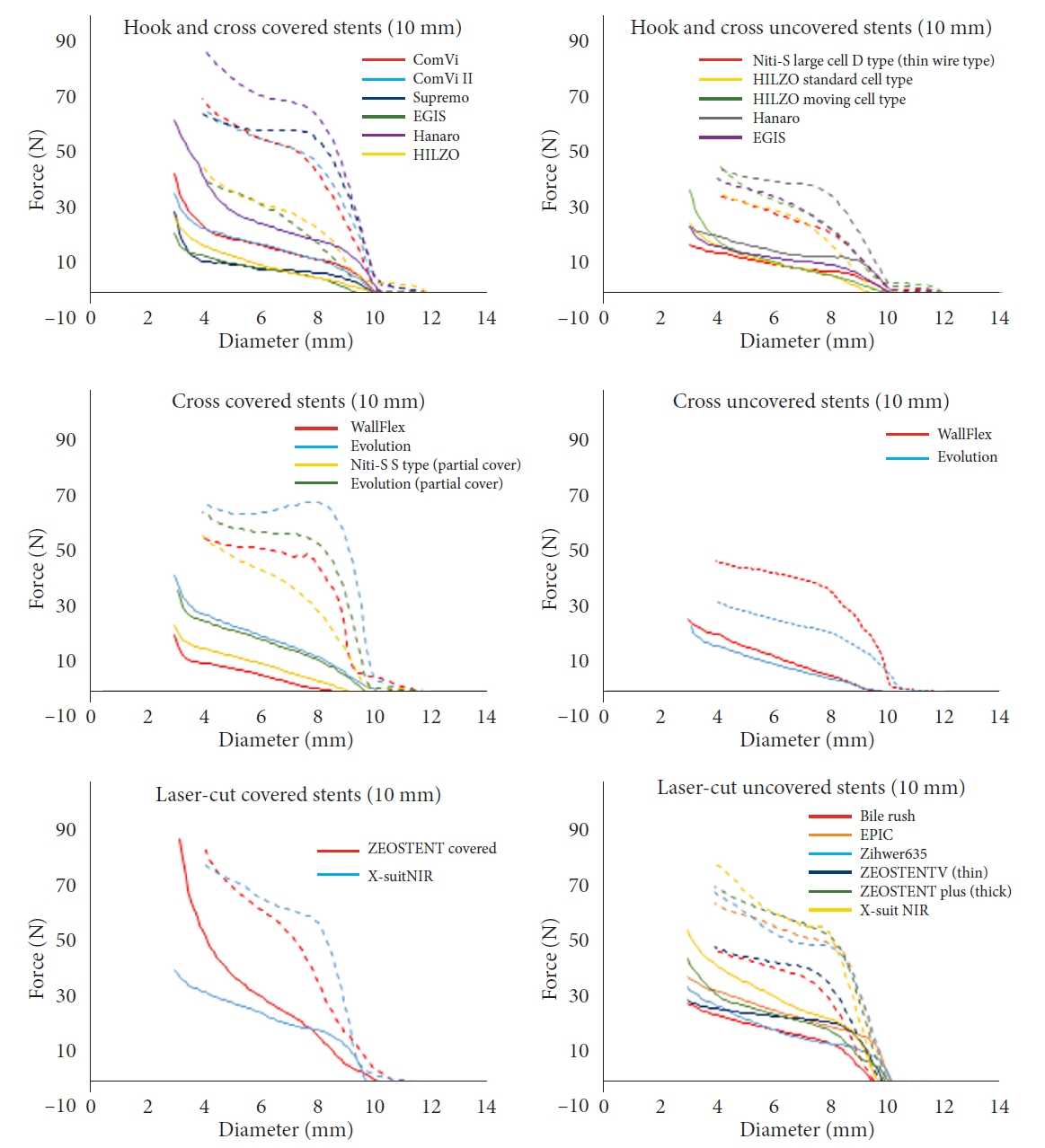
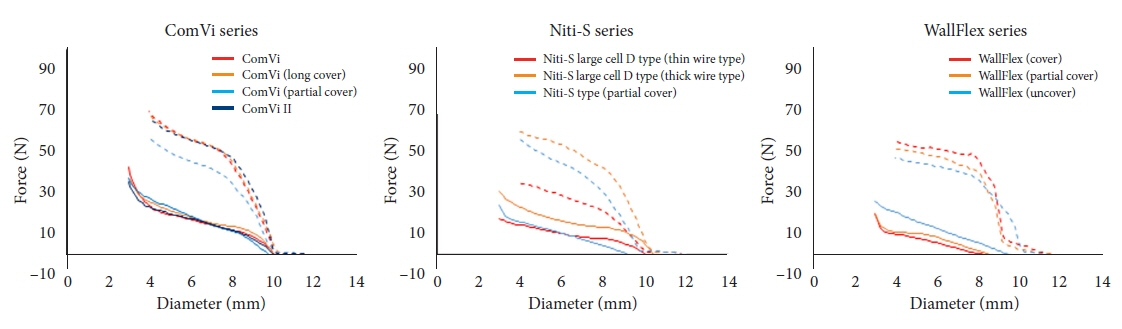
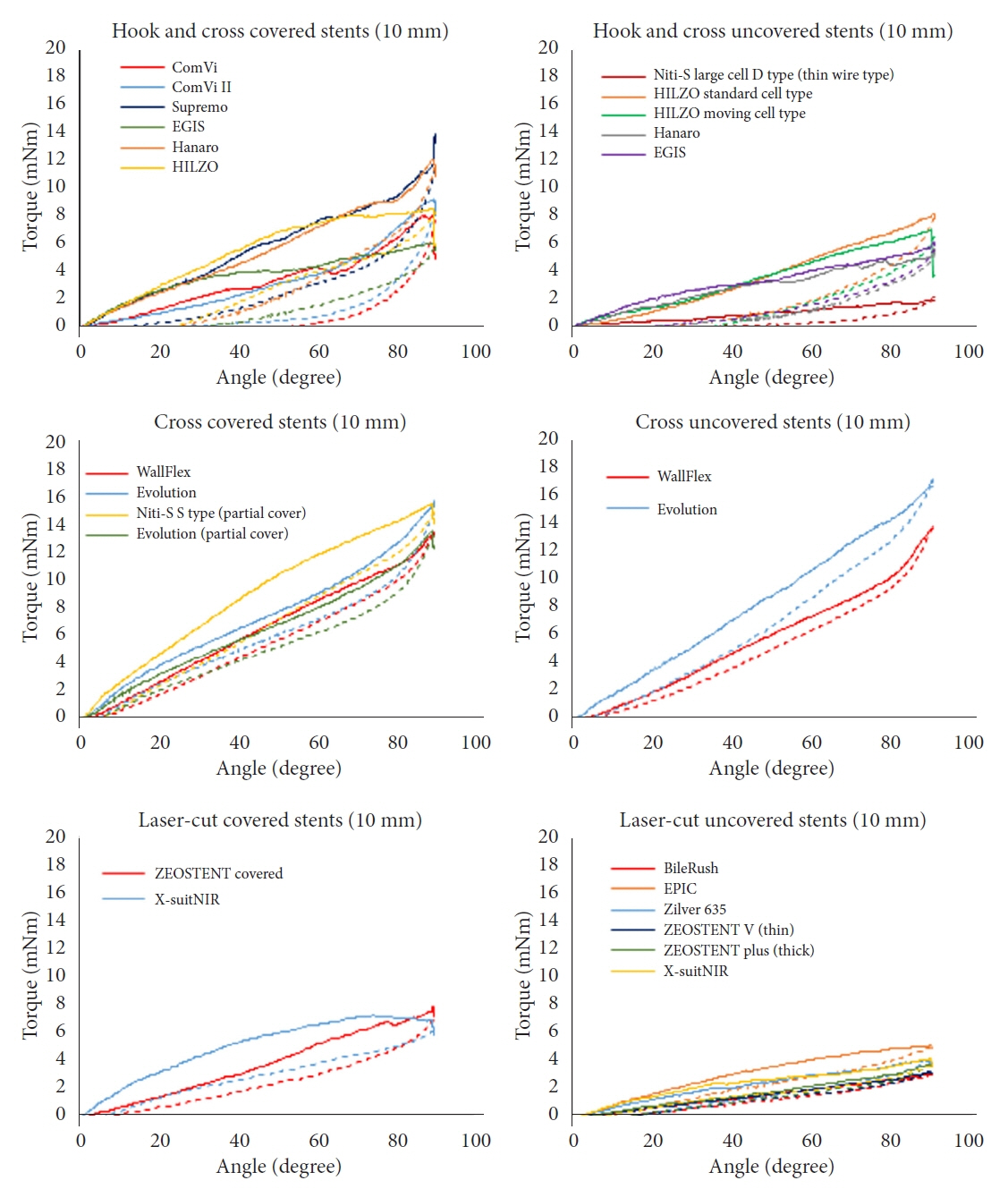
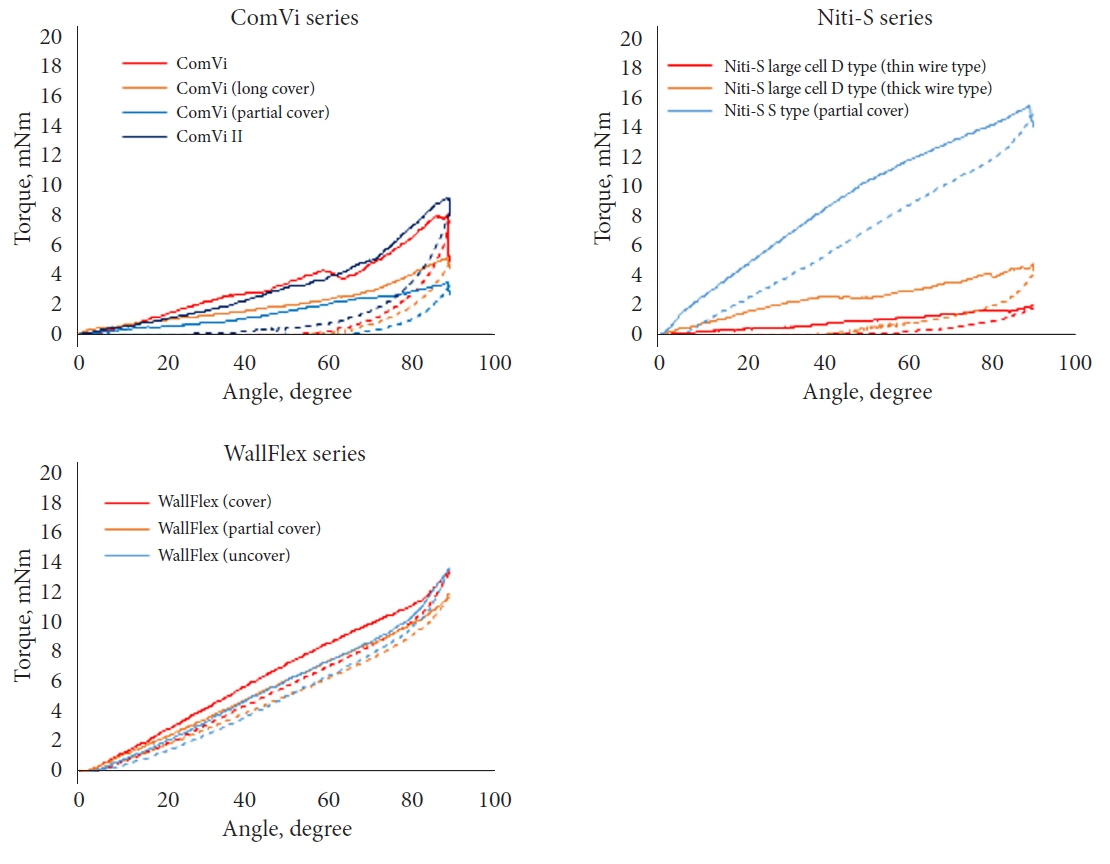
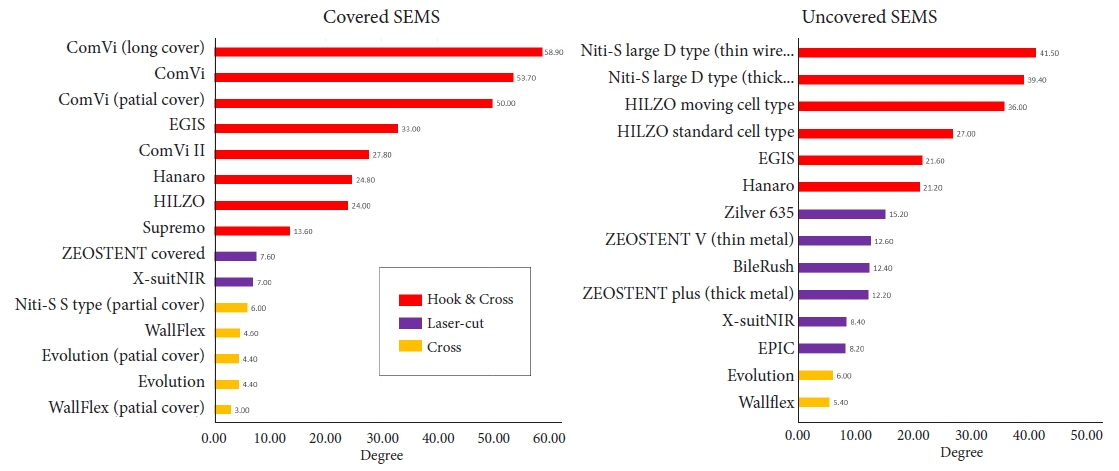
A high correlation in AFs was observed, as measured by the new and conventional manual methods. AF and RF scatterplots divided the SEMSs into three subgroups according to structure: hook-and-cross-type (low AF and RF), cross-type (high AF and low RF), and laser-cut-type (intermediate AF and high RF). The hook-and-cross-type had the largest axial force zero border (>20°), followed by the laser-cut and cross types.
Conclusions
MPs were related to stent structure. Hook-and-cross-type SEMSs had a low AF and high axial force zero border and were considered safest because they caused minimal stress on the biliary wall. However, the increase in RF must be overcome.
Keyword
Figure
Cited by 1 articles
-
How to reduce fistula formation after self-expandable metallic stent insertion for treating malignant esophageal stricture?
Kwang Bum Cho
Clin Endosc. 2023;56(6):735-737. doi: 10.5946/ce.2023.257.
Reference
-
1. Conio M, Mangiavillano B, Caruso A, et al. Covered versus uncovered self-expandable metal stent for palliation of primary malignant extrahepatic biliary strictures: a randomized multicenter study. Gastrointest Endosc. 2018; 88:283–291.2. Sawas T, Al Halabi S, Parsi MA, et al. Self-expandable metal stents versus plastic stents for malignant biliary obstruction: a meta-analysis. Gastrointest Endosc. 2015; 82:256–267.3. Lam R, Muniraj T. Fully covered metal biliary stents: a review of the literature. World J Gastroenterol. 2021; 27:6357–6373.4. Kitagawa K, Mitoro A, Ozutsumi T, et al. Laser-cut-type versus braided-type covered self-expandable metallic stents for distal biliary obstruction caused by pancreatic carcinoma: a retrospective comparative cohort study. Clin Endosc. 2022; 55:434–442.5. Isayama H, Mukai T, Itoi T, et al. Comparison of partially covered nitinol stents with partially covered stainless stents as a historical control in a multicenter study of distal malignant biliary obstruction: the WATCH study. Gastrointest Endosc. 2012; 76:84–92.6. Saito H, Sakurai Y, Takamura A, et al. [Biliary endoprosthesis using Gore-Tex covered expandable metallic stents: preliminary clinical evaluation]. Nihon Igaku Hoshasen Gakkai Zasshi. 1994; 54:180–182.7. Hori Y, Hayashi K, Yoshida M, et al. Novel characteristics of traction force in biliary self-expandable metallic stents. Dig Endosc. 2017; 29:347–352.8. U.S. Department of Health and Human Services, Food and Drug Administration. Center for Devices and Radiological Health. Metal expandable biliary stents: premarket notification (510(k)) submissions. Silver Spring: Center for Drug Evaluation and Research;2019.9. Isayama H, Nakai Y, Toyokawa Y, et al. Measurement of radial and axial forces of biliary self-expandable metallic stents. Gastrointest Endosc. 2009; 70:37–44.10. Katsinelos P, Lazaraki G, Gkagkalis S, et al. A fully covered self-expandable metal stent anchored by a 10-Fr double pigtail plastic stent: an effective anti-migration technique. Ann Gastroenterol. 2017; 30:114–117.11. Isayama H, Nakai Y, Hamada T, et al. Understanding the mechanical forces of self-expandable metal stents in the biliary ducts. Curr Gastroenterol Rep. 2016; 18:64.12. Nakai Y, Isayama H, Kawakubo K, et al. Metallic stent with high axial force as a risk factor for cholecystitis in distal malignant biliary obstruction. J Gastroenterol Hepatol. 2014; 29:1557–1562.13. Jang S, Stevens T, Parsi M, et al. Association of covered metallic stents with cholecystitis and stent migration in malignant biliary stricture. Gastrointest Endosc. 2018; 87:1061–1070.14. Kawakubo K, Isayama H, Nakai Y, et al. Risk factors for pancreatitis following transpapillary self-expandable metal stent placement. Surg Endosc. 2012; 26:771–776.15. Takeda T, Sasaki T, Mie T, et al. Novel risk factors for recurrent biliary obstruction and pancreatitis after metallic stent placement in pancreatic cancer. Endosc Int Open. 2020; 8:E1603–E1610.16. Nakai Y, Isayama H, Kogure H, et al. Risk factors for covered metallic stent migration in patients with distal malignant biliary obstruction due to pancreatic cancer. J Gastroenterol Hepatol. 2014; 29:1744–1749.17. Sasaki T, Ishibashi R, Yoshida S, et al. Comparing the mechanical properties of a self-expandable metallic stent for colorectal obstruction: proposed measurement method of axial force using a new measurement machine. Dig Endosc. 2021; 33:170–178.18. Rodrigues-Pinto E, Morais R, Sousa-Pinto B, et al. Development of an online app to predict post-endoscopic retrograde cholangiopancreatography adverse events using a single-center retrospective cohort. Dig Dis. 2021; 39:283–293.19. Ida Bagus B. A rare clinical presentation of third part duodenal perforation due to post-endoscopic retrograde cholangiopancreatography stent migration on advanced stage peri-ampullary tumor. JGH Open. 2021; 5:968–970.20. Mukai T, Yasuda I, Isayama H, et al. Comparison of axial force and cell width of self-expandable metallic stents: which type of stent is better suited for hilar biliary strictures? J Hepatobiliary Pancreat Sci. 2011; 18:646–652.21. Weaver M, Lang G, Das K, et al. Metal biliary stent erosion through the common bile duct leading to obstructive jaundice and cholangitis. Am J Gastroenterol. 2021; 116:1372.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mechanical Property and Problems of the Self-expandable Metal Stent in Pancreaticobiliary Cancer
- Mechanical Characteristics of Self-expandable Metallic Stents: In Vitro Study with Three of Stress
- Metallic EndoCoilTM Stent Application for Patients with Malignant Obstructive Jaundice
- Basic Knowledge about Metal Stent Development
- Mechanical Characterization of Self-Expandable Esophageal Metal Stents