Obstet Gynecol Sci.
2023 Sep;66(5):347-363. 10.5468/ogs.22165.
Possible cognition changes in women with polycystic ovary syndrome: a narrative review
- Affiliations
-
- 1Reproductive Endocrinology Research Center, Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- 2Reproductive Health Research Center, Department of Obstetrics & Gynecology, Al-zahra Hospital, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran
- 3Skull Base Research Center, Loghman Hakim Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- 4Department of Nursing, Asadabad School of Medical Sciences, Asadabad, Iran
- 5Mother and Child Welfare Research Center, Hormozgan University of Medical Sciences, Bandar Abbas, Iran
- 6Midwifery and Reproductive Health Research Center, Department of Midwifery and Reproductive Health, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- KMID: 2545883
- DOI: http://doi.org/10.5468/ogs.22165
Abstract
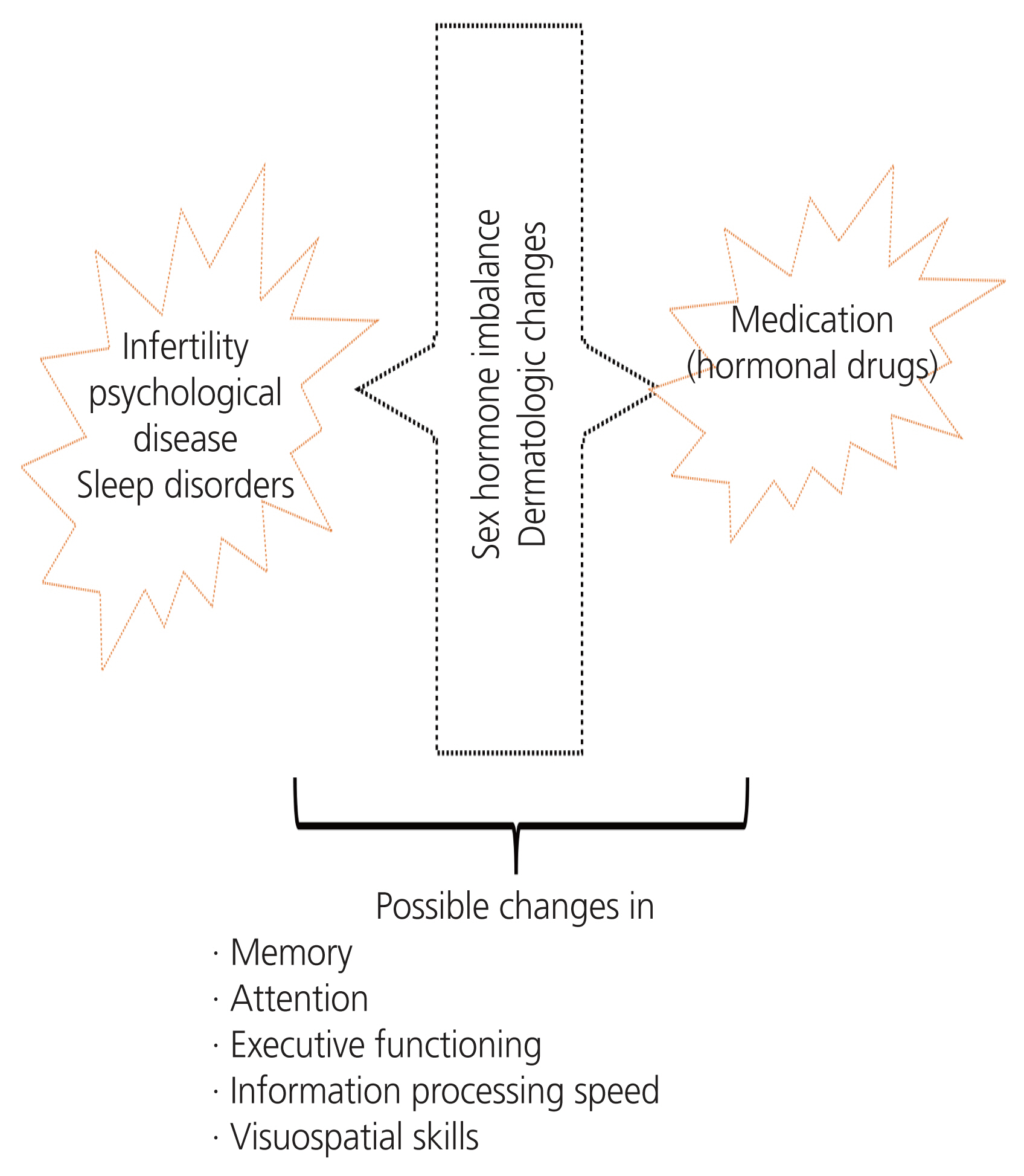
- Nowadays, polycystic ovary syndrome (PCOS) and cognitive dysfunction are major health problems among female. This narrative review aimed to investigate cognitive dysfunction in female with PCOS. English and Persian articles published in PubMed, Scopus, Web of Science, Google Scholar, PsycINFO, Scientific Information Database, and Cochrane Database of Systematic Reviews until May 2022 were searched. Sixteen studies involving 850 female with PCOS and 974 controls were assessed. In these studies, the association between biochemical factors and symptoms of PCOS and memory, attention, executive functioning, information processing speed, and visuospatial skills was evaluated. The literature review revealed the possible cognitive changes in female with PCOS. This study summarized the different aspects of cognitive function in female with PCOS due to medication, psychological problems (mood disorders caused by disease symptoms and complications), and biochemical markers, such as metabolic and sex hormone abnormalities. Considering the existing scientific gap regarding the possibility of cognitive complications in female with PCOS, further biological studies should be conducted to evaluate the potential mechanisms involved.
Figure
Reference
-
References
1. Wolf WM, Wattick RA, Kinkade ON, Olfert MD. Geographical prevalence of polycystic ovary syndrome as determined by region and race/ethnicity. Int J Environ Res Public Health. 2018; 15:2589.2. Ding T, Hardiman PJ, Petersen I, Wang FF, Qu F, Baio G. The prevalence of polycystic ovary syndrome in reproductive-aged women of different ethnicity: a systematic review and meta-analysis. Oncotarget. 2017; 8:96351–8.3. Naz MSG, Tehrani FR, Majd HA, Ahmadi F, Ozgoli G, Fakari FR, et al. The prevalence of polycystic ovary syndromein adolescents: a systematic review andmeta-analysis. Int J Reprod Biomed. 2019; 17:533–42.4. Riestenberg C, Jagasia A, Azziz R. Pregnancy-related economic burden of polycystic ovary syndrome (PCOS). Fertil Steril. 2019; 112:e43.5. Azziz R, Marin C, Hoq L, Badamgarav E, Song P. Health care-related economic burden of the polycystic ovary syndrome during the reproductive life span. J Clin Endocrinol Metab. 2005; 90:4650–8.6. Sulaiman MA, Al-Farsi YM, Al-Khaduri MM, Waly MI, Saleh J, Al-Adawi S. Psychological burden among women with polycystic ovarian syndrome in Oman: a case-control study. Int J Womens Health. 2017; 9:897–904.7. Saei Ghare Naz M, Ramezani Tehrani F, Behroozi Lak T, Mohammadzadeh F, Nasiri M, Kholosi Badr F, et al. Quality of life and emotional states of depression, anxiety and stress in adolescents with polycystic ovary syndrome: a cross-sectional study. Psychol Res Behav Manag. 2020; 13:203–9.8. Franik G, Krysta K, Witkowska A, Dudek A, Krzystanek M, Madej P. The impact of sex hormones and metabolic markers on depressive symptoms and cognitive functioning in PCOS patients. Gynecol Endocrinol. 2019; 35:965–9.9. Udiawar M. Cardiometabolic and neuroimaging correlates of cognitive function in polycystic ovary syndrome. Cardiff University;2017. Jul. 31. [Epub]. https://orca.cardiff.ac.uk/id/eprint/103000 .10. Barnard L, Balen AH, Ferriday D, Tiplady B, Dye L. Cognitive functioning in polycystic ovary syndrome. Psychoneuroendocrinology. 2007; 32:906–14.11. Fisher GG, Chacon M, Chaffee DS. Theories of Cognitive Aging and Work. Baltes BB, Rudolph CW, Zacher H, editors. Work Across the Lifespan. Cambridge (MA): Elsevier Academic Press;2019. p. 17–45.12. Vos SJB, van Boxtel MPJ, Schiepers OJG, Deckers K, de Vugt M, Carrière I, et al. Modifiable risk factors for prevention of dementia in midlife, late life and the oldest-old: validation of the LIBRA index. J Alzheimers Dis. 2017; 58:537–47.13. Livingston G, Sommerlad A, Orgeta V, Costafreda SG, Huntley J, Ames D, et al. Dementia prevention, intervention, and care. Lancet. 2017; 390:2673–734.14. World Health Organization. Dementia [Internet]. Geneva (CH): World Health Organization;c2022. [cited 2022 May 1]. Available from: https://www.who.int/health-topics/dementia .15. Patterson C. World Alzheimer report 2018 [Internet]. London (UK): Alzheimer’s Disease International;c2018. [cited 2022 May 22]. Available from: https://www.alz.co.uk/research/world-report-2018.AsDIWarF .16. Nichols E, Szoeke CEI, Vollset SE, Abbasi N, Abd-Allah F, Abdela J, et al. Global, regional, and national burden of Alzheimer’s disease and other dementias, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019; 18:88–106.17. Guoqing Z, Fang S, Lihui D, Bing Y, Qiaoling P, Yingting W, et al. Cerebral white matter lesions and silent cerebral infarcts in postmenopausal women with polycystic ovary syndrome. Gynecol Endocrinol. 2016; 32:655–8.18. Harvey RJ, Skelton-Robinson M, Rossor MN. The prevalence and causes of dementia in people under the age of 65 years. J Neurol Neurosurg Psychiatry. 2003; 74:1206–9.19. Hughes TF, Ganguli M. Modifiable midlife risk factors for late-life cognitive impairment and dementia. Curr Psychiatry Rev. 2009; 5:73–92.20. Bove RM, Brick DJ, Healy BC, Mancuso SM, Gerweck AV, Bredella MA, et al. Metabolic and endocrine correlates of cognitive function in healthy young women. Obesity (Silver Spring). 2013; 21:1343–9.21. Birdsall MA, Farquhar CM. Polycystic ovaries in pre and post-menopausal women. Clin Endocrinol (Oxf). 1996; 44:269–76.22. Elting MW, Korsen TJ, Rekers-Mombarg LT, Schoemaker J. Women with polycystic ovary syndrome gain regular menstrual cycles when ageing. Hum Reprod. 2000; 15:24–8.23. Brown ZA, Louwers YV, Fong SL, Valkenburg O, Birnie E, de Jong FH, et al. The phenotype of polycystic ovary syndrome ameliorates with aging. Fertil Steril. 2011; 96:1259–65.24. Noble H, Smith J. Reviewing the literature: choosing a review design. Evid Based Nurs. 2018; 21:39–41.25. Collins JA, Fauser BC. Balancing the strengths of systematic and narrative reviews. Hum Reprod Update. 2005; 11:103–4.26. Chaney MA. So you want to write a narrative review article? J Cardiothorac Vasc Anesth. 2021; 35:3045–9.27. Baethge C, Goldbeck-Wood S, Mertens S. SANRA-a scale for the quality assessment of narrative review articles. Res Integr Peer Rev. 2019; 4:5.28. Dumitrescu R, Mehedintu C, Briceag I, Purcarea VL, Hudita D. The polycystic ovary syndrome: an update on metabolic and hormonal mechanisms. J Med Life. 2015; 8:142–5.29. Walters KA, Gilchrist RB, Ledger WL, Teede HJ, Handelsman DJ, Campbell RE. New perspectives on the pathogenesis of PCOS: neuroendocrine origins. Trends Endocrinol Metab. 2018; 29:841–52.30. Upadhayay N, Guragain S. Comparison of cognitive functions between male and female medical students: a pilot study. J Clin Diagn Res. 2014; 8:BC12–5.31. Ciocca G, Limoncin E, Carosa E, Di Sante S, Gravina GL, Mollaioli D, et al. Is testosterone a food for the brain? Sex Med Rev. 2016; 4:15–25.32. Pintzka CW, Evensmoen HR, Lehn H, Håberg AK. Changes in spatial cognition and brain activity after a single dose of testosterone in healthy women. Behav Brain Res. 2016; 298:78–90.33. Rees DA, Udiawar M, Berlot R, Jones DK, O’Sullivan MJ. White matter microstructure and cognitive function in young women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2016; 101:314–23.34. McEwen BS, Alves SE. Estrogen actions in the central nervous system. Endocr Rev. 1999; 20:279–307.35. Leeners B, Kruger THC, Geraedts K, Tronci E, Mancini T, Ille F, et al. Lack of associations between female hormone levels and visuospatial working memory, divided attention and cognitive bias across two consecutive menstrual cycles. Front Behav Neurosci. 2017; 11:120.36. Sundström Poromaa I, Gingnell M. Menstrual cycle influence on cognitive function and emotion processing-from a reproductive perspective. Front Neurosci. 2014; 8:380.37. Pessoa L. Emotion and cognition and the amygdala: from “what is it?” to “what’s to be done?”. Neuropsychologia. 2010; 48:3416–29.38. Barry JA, Parekh HS, Hardiman PJ. Visual-spatial cognition in women with polycystic ovarian syndrome: the role of androgens. Hum Reprod. 2013; 28:2832–7.39. Lei Y, Renyuan Z. Effects of androgens on the amyloid-β protein in Alzheimer’s disease. Endocrinology. 2018; 159:3885–94.40. Chen GF, Xu TH, Yan Y, Zhou YR, Jiang Y, Melcher K, et al. Amyloid beta: structure, biology and structure-based therapeutic development. Acta Pharmacol Sin. 2017; 38:1205–35.41. Schattmann L, Sherwin BB. Testosterone levels and cognitive functioning in women with polycystic ovary syndrome and in healthy young women. Horm Behav. 2007; 51:587–96.42. Kara O, Kaymaz N, Uzun ME. The effect of hyperandrogenism and obesity on mindfulness and metacognition in adolescents with polycystic ovary syndrome. Arch Womens Ment Health. 2022; 25:911–21.43. Lai W, Li X, Zhu H, Zhu X, Tan H, Feng P, et al. Plasma luteinizing hormone level affects the brain activity of patients with polycystic ovary syndrome. Psychoneuroendocrinology. 2020; 112:104535.44. Rao CV. Involvement of luteinizing hormone in Alzheimer disease development in elderly women. Reprod Sci. 2017; 24:355–68.45. Ali SA, Begum T, Reza F. Hormonal influences on cognitive function. Malays J Med Sci. 2018; 25:31–41.46. Jamil AS, Alalaf SK, Al-Tawil NG, Al-Shawaf T. Comparison of clinical and hormonal characteristics among four phenotypes of polycystic ovary syndrome based on the Rotterdam criteria. Arch Gynecol Obstet. 2016; 293:447–56.47. Cooney LG, Lee I, Sammel MD, Dokras A. High prevalence of moderate and severe depressive and anxiety symptoms in polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod. 2017; 32:1075–91.48. Sukhapure M. Androgens and the female brain: the relationship between testosterone levels, depression, anxiety, cognitive function, and emotion processing in females with polycystic ovarian syndrome [Internet]. Dunedin (NZ): University of Otago;c2019. [cited 2022 May 1]. Available from: https://ourarchive.otago.ac.nz/bitstream/handle/10523/9347/SukhapureMayouri2018PhD.pdf?sequence=1&isAllowed=y .49. Mehrabadi S, Jahanian Sadatmahalleh S, Kazemnejad A. Association of depression and anxiety with cognitive function in patients with polycystic ovary syndrome. J Mazandaran Univ Med Sci. 2017; 27:159–70.50. Llewellyn DJ, Lang IA, Langa KM, Huppert FA. Cognitive function and psychological well-being: findings from a population-based cohort. Age Ageing. 2008; 37:685–9.51. Marin MF, Lord C, Andrews J, Juster RP, Sindi S, Arsenault-Lapierre G, et al. Chronic stress, cognitive functioning and mental health. Neurobiol Learn Mem. 2011; 96:583–95.52. Cooney LG, Dokras A. Beyond fertility: polycystic ovary syndrome and long-term health. Fertil Steril. 2018; 110:794–809.53. Kahal H, Kyrou I, Uthman OA, Brown A, Johnson S, Wall PDH, et al. The prevalence of obstructive sleep apnoea in women with polycystic ovary syndrome: a systematic review and meta-analysis. Sleep Breath. 2020; 24:339–50.54. Garvey JF, Pengo MF, Drakatos P, Kent BD. Epidemiological aspects of obstructive sleep apnea. J Thorac Dis. 2015; 7:920–9.55. Krysta K, Bratek A, Zawada K, Stepańczak R. Cognitive deficits in adults with obstructive sleep apnea compared to children and adolescents. J Neural Transm (Vienna). 2017; 124:187–201.56. Karapin P, Šiarnik P, Suchá B, Jurík M, Tedla M, Poddaný M, et al. Cognition in patients with sleep-disordered breathing: can obstructive and central apneic pauses play a different role in cognitive impairment? Life (Basel). 2022; 12:1180.57. Lajoie AC, Lafontaine AL, Kimoff RJ, Kaminska M. Obstructive sleep apnea in neurodegenerative disorders: current evidence in support of benefit from sleep apnea treatment. J Clin Med. 2020; 9:297.58. Harrington YA, Parisi JM, Duan D, Rojo-Wissar DM, Holingue C, Spira AP. Sex hormones, sleep, and memory: interrelationships across the adult female lifespan. Front Aging Neurosci. 2022; 14:800278.59. Moura HH, Costa DL, Bagatin E, Sodré CT, Manela-Azulay M. Polycystic ovary syndrome: a dermatologic approach. An Bras Dermatol. 2011; 86:111–9.60. Deveci E, Öztürk A, Kırpınar I, Koyuncu A, Engin I, Melikoğlu M, et al. Neurocognition in patients with acne vulgaris. J Psychiatry. 2014. Apr. 30. [Epub]. https://doi.org/10.4172/Psychiatry.1000121 .61. Mehrabadi S, Jahanian Sadatmahalleh SH, Kazemnejad A. The relationship between acne and cognitive function in patients with polycystic ovary syndrome and healthy women. J Guilan Univ of Med Sci. 2018; 27:37–42.62. Golchai J, Khani SH, Heidarzadeh A, Eshkevari SS, Alizade N, Eftekhari H. Comparison of anxiety and depression in patients with acne vulgaris and healthy individuals. Indian J Dermatol. 2010; 55:352–4.63. Yazici K, Baz K, Yazici A, Köktürk A, Tot S, Demirseren D, et al. Disease-specific quality of life is associated with anxiety and depression in patients with acne. J Eur Acad Dermatol Venereol. 2004; 18:435–9.64. Perini G, Cotta Ramusino M, Sinforiani E, Bernini S, Petrachi R, Costa A. Cognitive impairment in depression: recent advances and novel treatments. Neuropsychiatr Dis Treat. 2019; 15:1249–58.65. Jafferany M, Patel A. Understanding psychocutaneous disease: psychosocial & psychoneuroimmunologic perspectives. Int J Dermatol. 2020; 59:8–15.66. Mashayekhi Goyonlo V, Sardabi MS, Tavalaei AM, Khoshnevisan Z, Razmara M. Cognitive behavioral therapy as an adjuvant therapy in acne excoriée: a randomized controlled clinical trial. J Dermatolog Treat. 2022; 33:782–8.67. Tavares A, Rêgo Barros RC. The prevalence of metabolic syndrome in the different phenotypes of polycystic ovarian syndrome. Rev Bras Ginecol Obstet. 2019; 41:37–43.68. Pillai BP, Kumar H, Jayakumar RV, Alur V, Sheejamol VS. The prevalence of metabolic syndrome in polycystic ovary syndrome in a South Indian population and the use of neck circumference in defining metabolic syndrome. Int J Diabetes Dev Ctries. 2015; 35:469–75.69. Yates KF, Sweat V, Yau PL, Turchiano MM, Convit A. Impact of metabolic syndrome on cognition and brain: a selected review of the literature. Arterioscler Thromb Vasc Biol. 2012; 32:2060–7.70. Lujan ME, Mergler R. Cognitive function in women with polycystic ovary syndrome (PCOS): impact of reproductive and metabolic factors. Fertil Steril. 2015; 104:E129.71. Neergaard JS, Dragsbæk K, Christiansen C, Nielsen HB, Brix S, Karsdal MA, et al. Metabolic syndrome, insulin resistance, and cognitive dysfunction: does your metabolic profile affect your brain? Diabetes. 2017; 66:1957–63.72. van Gemert T, Wölwer W, Weber KS, Hoyer A, Strassburger K, Bohnau NT, et al. Cognitive function is impaired in patients with recently diagnosed type 2 diabetes, but not type 1 diabetes. J Diabetes Res. 2018; 2018:1470476.73. Castellano CA, Baillargeon JP, Nugent S, Tremblay S, Fortier M, Imbeault H, et al. Regional brain glucose hypometabolism in young women with polycystic ovary syndrome: possible link to mild insulin resistance. PLoS One. 2015; 10:e0144116.74. Jarrett BY, Vantman N, Mergler RJ, Brooks ED, Pierson RA, Chizen DR, et al. Dysglycemia, not altered sex steroid hormones, affects cognitive function in polycystic ovary syndrome. J Endocr Soc. 2019; 3:1858–68.75. Zheng F, Yan L, Yang Z, Zhong B, Xie W. HbA1c, diabetes and cognitive decline: the English Longitudinal Study of Ageing. Diabetologia. 2018; 61:839–48.76. Janssen J, van den Berg E, Zinman B, Espeland MA, Geijselaers SLC, Mattheus M, et al. HbA1c, insulin resistance, and β-cell function in relation to cognitive function in type 2 diabetes: the CAROLINA cognition substudy. Diabetes Care. 2019; 42:e1–3.77. Huang Y, Wang A. Cognitive disorder in women with polycystic ovary syndrome: a remote complication. J Pediatr Adolesc Gynecol. 2014; 27:240–1.78. Lim SS, Davies MJ, Norman RJ, Moran LJ. Overweight, obesity and central obesity in women with polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update. 2012; 18:618–37.79. Cook RL, O’Dwyer NJ, Donges CE, Parker HM, Cheng HL, Steinbeck KS, et al. Relationship between obesity and cognitive function in young women: the food, mood and mind study. J Obes. 2017; 2017:5923862.80. Hou Q, Guan Y, Yu W, Liu X, Wu L, Xiao M, et al. Associations between obesity and cognitive impairment in the Chinese elderly: an observational study. Clin Interv Aging. 2019; 14:367–73.81. Nguyen JC, Killcross AS, Jenkins TA. Obesity and cognitive decline: role of inflammation and vascular changes. Front Neurosci. 2014; 8:375.82. Li G, Hu J, Zhang S, Fan W, Wen L, Wang G, et al. Changes in resting-state cerebral activity in women with polycystic ovary syndrome: a functional mr imaging study. Front Endocrinol (Lausanne). 2020; 11:603279.83. Mehrabadi S, Sadatmahalleh SJ, Kazemnejad A, Moini A. Association of acne, hirsutism, androgen, anxiety, and depression on cognitive performance in polycystic ovary syndrome: a cross-sectional study. Int J Reprod Biomed. 2020; 18:1049–58.84. Sukhapure M, Eggleston K, Douglas K, Fenton A, Frampton C, Porter RJ. Free testosterone is related to aspects of cognitive function in women with and without polycystic ovary syndrome. Arch Womens Ment Health. 2022; 25:87–94.85. Shi Y, Cui Y, Sun X, Ma G, Ma Z, Gao Q, et al. Hypertension in women with polycystic ovary syndrome: prevalence and associated cardiovascular risk factors. Eur J Obstet Gynecol Reprod Biol. 2014; 173:66–70.86. Joham AE, Boyle JA, Zoungas S, Teede HJ. Hypertension in reproductive-aged women with polycystic ovary syndrome and association with obesity. Am J Hypertens. 2015; 28:847–51.87. Iadecola C, Yaffe K, Biller J, Bratzke LC, Faraci FM, Gorelick PB, et al. Impact of hypertension on cognitive function: a scientific statement from the American Heart Association. Hypertension. 2016; 68:e67–94.88. Birns J, Kalra L. Cognitive function and hypertension. J Hum Hypertens. 2009; 23:86–96.89. Read SL, Grundy EMD. Fertility history and cognition in later life. J Gerontol B Psychol Sci Soc Sci. 2017; 72:1021–31.90. Saenz JL, Díaz-Venegas C, Crimmins EM. Fertility history and cognitive function in late life: the case of Mexico. J Gerontol B Psychol Sci Soc Sci. 2021; 76:e140–52.91. Palomba S, Santagni S, Falbo A, La Sala GB. Complications and challenges associated with polycystic ovary syndrome: current perspectives. Int J Womens Health. 2015; 7:745–63.92. Karim R, Dang H, Henderson VW, Hodis HN, StJohn J, Brinton RD, et al. Effect of reproductive history and exogenous hormone use on cognitive function in mid- and late life. J Am Geriatr Soc. 2016; 64:2448–56.93. Prince MJ, Acosta D, Guerra M, Huang Y, Jimenez-Velazquez IZ, Llibre Rodriguez JJ, et al. Reproductive period, endogenous estrogen exposure and dementia incidence among women in Latin America and China; a 10/66 population-based cohort study. PLoS One. 2018; 13:e0192889.94. Peterson A, Tom SE. A lifecourse perspective on female sex-specific risk factors for later life cognition. Curr Neurol Neurosci Rep. 2021; 21:46.95. Xu XL, Deng SL, Lian ZX, Yu K. Estrogen receptors in polycystic ovary syndrome. Cells. 2021; 10:459.96. Schelbaum E, Loughlin L, Jett S, Zhang C, Jang G, Malviya N, et al. Association of reproductive history with brain MRI biomarkers of dementia risk in midlife. Neurology. 2021; 97:e2328–39.97. Leeners B, Krüger T, Geraedts K, Tronci E, Mancini T, Ille F, et al. Cognitive function in association with high estradiol levels resulting from fertility treatment. Horm Behav. 2021; 130:104951.98. Legro RS, Arslanian SA, Ehrmann DA, Hoeger KM, Murad MH, Pasquali R, et al. Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2013; 98:4565–92.99. Warren AM, Gurvich C, Worsley R, Kulkarni J. A systematic review of the impact of oral contraceptives on cognition. Contraception. 2014; 90:111–6.100. Botsali A, Kocyigit P, Uran P. The effects of isotretinoin on affective and cognitive functions are disparate in adolescent acne vulgaris patients. J Dermatolog Treat. 2020; 31:734–8.101. Soleman RS, Kreukels BPC, Veltman DJ, Cohen-Kettenis PT, Hompes PGA, Drent ML, et al. Does polycystic ovary syndrome affect cognition? A functional magnetic resonance imaging study exploring working memory. Fertil Steril. 2016; 105:1314–21e1.102. Schattmann L, Sherwin BB. Effects of the pharmacologic manipulation of testosterone on cognitive functioning in women with polycystic ovary syndrome: a randomized, placebo-controlled treatment study. Horm Behav. 2007; 51:579–86.103. Alzaid A, Tourkmani A, Alsahaby A, Robert A, Bin Rsheed A, Alabood A, et al. Metformin therapy improves cognitive function in women with polycystic ovary syndrome (PCOS). Diabetologia. 2017; 60(Suppl 1):581–2.104. Liu J, Wu Q, Hao Y, Jiao M, Wang X, Jiang S, et al. Measuring the global disease burden of polycystic ovary syndrome in 194 countries: Global Burden of Disease Study 2017. Hum Reprod. 2021; 36:1108–19.105. Park CH, Chun S. Influence of combined oral contraceptives on polycystic ovarian morphology-related parameters in Korean women with polycystic ovary syndrome. Obstet Gynecol Sci. 2020; 63:80–6.106. Moradi N, Bidgoli SA, Chaichian S. Ovarian cysts disappear after 14-day oral regimen of Korean red ginseng extract in letrozole-induced polycystic ovarian syndrome. Obstet Gynecol Sci. 2021; 64:874–83.107. Pasquali R. Contemporary approaches to the management of polycystic ovary syndrome. Ther Adv Endocrinol Metab. 2018; 9:123–34.108. Sanchez-Garrido MA, Tena-Sempere M. Metabolic dysfunction in polycystic ovary syndrome: pathogenic role of androgen excess and potential therapeutic strategies. Mol Metab. 2020; 35:100937.109. Van Duinkerken E, Snoek FJ, de Wit M. The cognitive and psychological effects of living with type 1 diabetes: a narrative review. Diabet Med. 2020; 37:555–63.110. Sutin AR, Stephan Y, Terracciano A. Psychological distress, self-beliefs, and risk of cognitive impairment and dementia. J Alzheimers Dis. 2018; 65:1041–50.111. Guicciardi M, Crisafulli A, Doneddu A, Fadda D, Lecis R. Effects of metabolic syndrome on cognitive performance of adults during exercise. Front Psychol. 2019; 10:1845.112. Kim B, Feldman EL. Insulin resistance as a key link for the increased risk of cognitive impairment in the metabolic syndrome. Exp Mol Med. 2015; 47:e149.113. Ozgen Saydam B, Yildiz BO. Polycystic ovary syndrome and brain: an update on structural and functional studies. J Clin Endocrinol Metab. 2020; 106:e430–41.114. Gaspar JM, Baptista FI, Macedo MP, Ambrósio AF. Inside the diabetic brain: role of different players involved in cognitive decline. ACS Chem Neurosci. 2016; 7:131–42.115. Rocha AL, Oliveira FR, Azevedo RC, Silva VA, Peres TM, Candido AL, et al. Recent advances in the understanding and management of polycystic ovary syndrome. F1000Res. 2019. Apr. 26. [Epub]. https://doi.org/10.12688/f1000research.15318.1 .116. Boivin MJ, Fatehi F, Phillips-Chan AE, Richardson JR, Summers AN, Foley SA. Exploratory study of a screening measure for polycystic ovarian syndrome, quality of life assessment, and neuropsychological evaluation. BMC Womens Health. 2020; 20:132.117. Teede HJ, Misso ML, Costello MF, Dokras A, Laven J, Moran L, et al. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Hum Reprod. 2018; 33:1602–18.118. Barry JA. Psychological aspects of polycystic ovary syndrome. London (UK): Palgrave Macmillan;2019.119. Ranjbar F, Moazeni F, Abdi M, Khoshnou H, Khademi E, Amiri S, et al. Evaluation of spatial memory in women with polycystic ovary syndrome. Iran J Obstet Gynecol Infertil. 2020; 23:1–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Studies on Fibrinolytic System Behavior in Women with Polycystic Ovary Syndrome
- Medical diagnosis and treatment of polycystic ovary syndrome
- Epidemiology and Diagnostic Criteria of Polycystic Ovary Syndrome
- Inter-ovarian differences in ultrasound markers of ovarian size in women with polycystic ovary syndrome
- Polycystic Ovary Syndrome and Women Health