Korean J Sports Med.
2023 Sep;41(3):119-129. 10.5763/kjsm.2023.41.3.119.
The Emerging Role of Exercise and Optimal Exercise Prescription for Improving the Symptoms of Long COVID
- Affiliations
-
- 1Department of Sport Science, University of Seoul, Seoul, Korea
- 2Diabetes Research Centre, Leicester General Hospital, University of Leicester, Leicester, UK
- 3Division of Urban Social Health, Graduate School of Urban Public Health, University of Seoul, Seoul, Korea
- 4Department of Urban Big Data Convergence, University of Seoul, Seoul, Korea
- KMID: 2545826
- DOI: http://doi.org/10.5763/kjsm.2023.41.3.119
Abstract
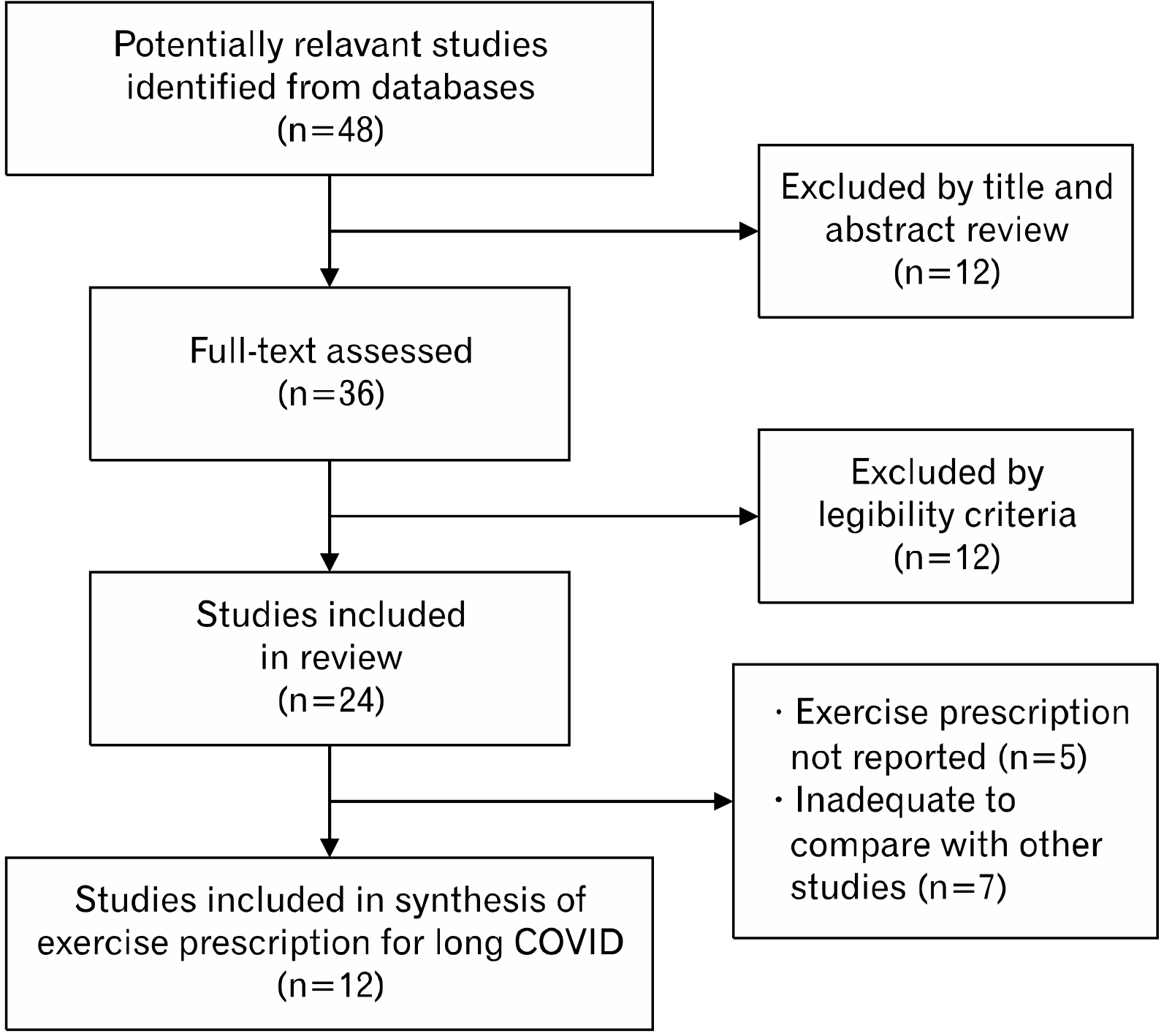
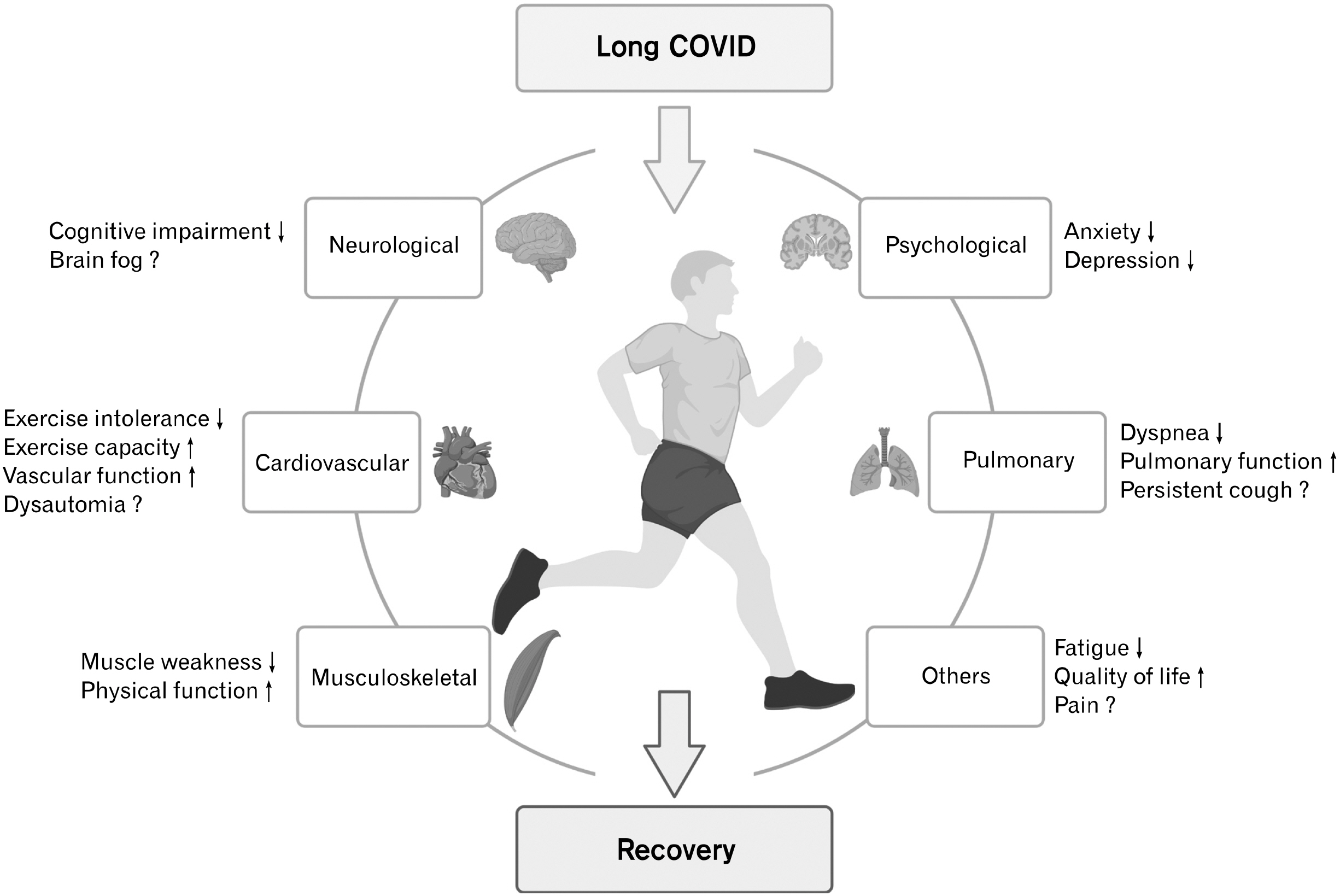
- Long COVID has emerged as a global medical challenge, characterized by persistent symptoms such as fatigue, dyspnea, and exercise intolerance following a coronavirus disease 19 (COVID-19) infection. The protracted nature of these symptoms necessitates the development of effective therapeutic approaches to alleviate the burden on individuals’ well-being and the healthcare system at large. While current pharmacological interventions offer limited efficacy, the exploration of alternative strategies becomes imperative. Exercise training has demonstrated promise in ameliorating long COVID symptoms, yet consensus regarding the optimal exercise modalities remains elusive. In light of this, the present review aims to elucidate the impact of exercise on long COVID symptoms and shed light on exercise prescriptions that have exhibited proven efficacy in the treatment and management of this syndrome.
Figure
Reference
-
1. Soriano JB, Murthy S, Marshall JC, Relan P, Diaz JV. WHO Clinical Case Definition Working Group on Post-COVID-19 Condition. 2022; A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect Dis. 22:e102–7. DOI: 10.1016/S1473-3099(21)00703-9. PMID: 34951953. PMCID: PMC8691845.
Article2. Chen C, Haupert SR, Zimmermann L, Shi X, Fritsche LG, Mukherjee B. 2022; Global Prevalence of post-coronavirus disease 2019 (COVID-19) condition or long COVID: a meta-analysis and systematic review. J Infect Dis. 226:1593–607. DOI: 10.1093/infdis/jiac136. PMID: 35429399. PMCID: PMC9047189.
Article3. Lopez-Leon S, Wegman-Ostrosky T, Perelman C, et al. 2021; More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. Sci Rep. 11:16144. DOI: 10.1038/s41598-021-95565-8. PMID: 34373540. PMCID: PMC8352980.
Article4. Nasserie T, Hittle M, Goodman SN. 2021; Assessment of the frequency and variety of persistent symptoms among patients with COVID-19: a systematic review. JAMA Netw Open. 4:e2111417. DOI: 10.1001/jamanetworkopen.2021.11417. PMID: 34037731. PMCID: PMC8155823.5. Jiang DH, Roy DJ, Gu BJ, Hassett LC, McCoy RG. 2021; Post-acute sequelae of severe acute respiratory syndrome corona-virus 2 infection: a state-of-the-art review. JACC Basic Transl Sci. 6:796–811. DOI: 10.1016/j.jacbts.2021.07.002. PMID: 34541421. PMCID: PMC8442719.
Article6. Tran VT, Porcher R, Pane I, Ravaud P. 2022; Course of post COVID-19 disease symptoms over time in the ComPaRe long COVID prospective e-cohort. Nat Commun. 13:1812. DOI: 10.1038/s41467-022-29513-z. PMID: 35383197. PMCID: PMC8983754.7. Wulf Hanson S, Abbafati C, et al. Global Burden of Disease Long COVID Collaborators. 2022; Estimated global proportions of individuals with persistent fatigue, cognitive, and respiratory symptom clusters following symptomatic COVID-19 in 2020 and 2021. JAMA. 328:1604–15. DOI: 10.1001/jama.2022.18931. PMID: 36215063. PMCID: PMC9552043.8. Davis HE, Assaf GS, McCorkell L, et al. 2021; Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine. 38:101019. DOI: 10.1016/j.eclinm.2021.101019. PMID: 34308300. PMCID: PMC8280690.
Article9. Nguyen NN, Hoang VT, Dao TL, Dudouet P, Eldin C, Gautret P. 2022; Clinical patterns of somatic symptoms in patients suffering from post-acute long COVID: a systematic review. Eur J Clin Microbiol Infect Dis. 41:515–45. DOI: 10.1007/s10096-022-04417-4. PMID: 35142947. PMCID: PMC8830952.
Article10. Sudre CH, Murray B, Varsavsky T, et al. 2021; Attributes and predictors of long COVID. Nat Med. 27:626–31. DOI: 10.1038/s41591-021-01292-y. PMID: 33692530. PMCID: PMC7611399.
Article11. Selvakumar J, Havdal LB, Drevvatne M, et al. 2023; Prevalence and characteristics associated with post-COVID-19 condition among nonhospitalized adolescents and young adults. JAMA Netw Open. 6:e235763. DOI: 10.1001/jamanetworkopen.2023.5763. PMID: 36995712. PMCID: PMC10064252.
Article12. Mogensen I, Ekström S, Hallberg J, et al. 2023; Post COVID-19 symptoms are common, also among young adults in the general population. Sci Rep. 13:11300. DOI: 10.1038/s41598-023-38315-2. PMID: 37438424. PMCID: PMC10338459.
Article13. Yelin D, Moschopoulos CD, Margalit I, et al. 2022; ESCMID rapid guidelines for assessment and management of long COVID. Clin Microbiol Infect. 28:955–72. DOI: 10.1016/j.cmi.2022.02.018. PMID: 35182760. PMCID: PMC8849856.
Article14. Mehandru S, Merad M. 2022; Pathological sequelae of long-haul COVID. Nat Immunol. 23:194–202. DOI: 10.1038/s41590-021-01104-y. PMID: 35105985. PMCID: PMC9127978.
Article15. Desai AD, Lavelle M, Boursiquot BC, Wan EY. 2022; Long-term complications of COVID-19. Am J Physiol Cell Physiol. 322:C1–11. DOI: 10.1152/ajpcell.00375.2021. PMID: 34817268. PMCID: PMC8721906.
Article16. Khazaal S, Harb J, Rima M, et al. 2022; The pathophysiology of long COVID throughout the renin-angiotensin system. Molecules. 27:2903. DOI: 10.3390/molecules27092903. PMID: 35566253. PMCID: PMC9101946.
Article17. Chee YJ, Fan BE, Young BE, Dalan R, Lye DC. 2023; Clinical trials on the pharmacological treatment of long COVID: a systematic review. J Med Virol. 95:e28289. DOI: 10.1002/jmv.28289. PMID: 36349400. PMCID: PMC9878018.
Article18. Greenhalgh T, Knight M, A'Court C, Buxton M, Husain L. 2020; Management of post-acute covid-19 in primary care. BMJ. 370:m3026. DOI: 10.1136/bmj.m3026. PMID: 32784198.
Article19. Ayoubkhani D, Khunti K, Nafilyan V, et al. 2021; Post-covid syndrome in individuals admitted to hospital with covid-19: retrospective cohort study. BMJ. 372:n693. DOI: 10.1136/bmj.n693. PMID: 33789877. PMCID: PMC8010267.
Article20. Bushman BA. 2019; Physical activity guidelines for Americans: the relationship between physical activity and health. ACSMs Health Fit J. 23:5–9. DOI: 10.1249/FIT.0000000000000472.21. Posadzki P, Pieper D, Bajpai R, et al. 2020; Exercise/physical activity and health outcomes: an overview of Cochrane systematic reviews. BMC Public Health. 20:1724. DOI: 10.1186/s12889-020-09855-3. PMID: 33198717. PMCID: PMC7670795.
Article22. Garber CE, Blissmer B, Deschenes MR, et al. 2011; American College of Sports Medicine position stand: quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 43:1334–59. DOI: 10.1249/MSS.0b013e318213fefb. PMID: 21694556.23. Fiuza-Luces C, Garatachea N, Berger NA, Lucia A. 2013; Exercise is the real polypill. Physiology (Bethesda). 28:330–58. DOI: 10.1152/physiol.00019.2013. PMID: 23997192.
Article24. Lee SW, Lee J, Moon SY, et al. 2022; Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: a nationwide cohort study. Br J Sports Med. 56:901–12. DOI: 10.1136/bjsports-2021-104203. PMID: 34301715.
Article25. Jimeno-Almazán A, Pallarés JG, Buendía-Romero Á, et al. 2021; Post-COVID-19 syndrome and the potential benefits of exercise. Int J Environ Res Public Health. 18:5329. DOI: 10.3390/ijerph18105329. PMID: 34067776. PMCID: PMC8156194.
Article26. World Health Organization (WHO). 2023. Clinical management of COVID-19: living guideline, 13 January 2023 [Internet]. WHO;Available from: https://apps.who.int/iris/bitstream/handle/10665/365580/WHO-2019-nCoV-clinical-2023.1-eng.pdf. cited 2023 Jun 30.27. Shah W, Hillman T, Playford ED, Hishmeh L. 2021; Managing the long term effects of COVID-19: summary of NICE, SIGN, and RCGP rapid guideline. BMJ. 372:n136. DOI: 10.1136/bmj.n136. PMID: 33483331.
Article28. Halabchi F, Selk-Ghaffari M, Tazesh B, Mahdaviani B. 2022; The effect of exercise rehabilitation on COVID-19 outcomes: a systematic review of observational and intervention studies. Sport Sci Health. 18:1201–19. DOI: 10.1007/s11332-022-00966-5. PMID: 35789736. PMCID: PMC9244056.
Article29. Chen H, Shi H, Liu X, Sun T, Wu J, Liu Z. 2022; Effect of pulmonary rehabilitation for patients with post-COVID-19: a systematic review and meta-analysis. Front Med (Lausanne). 9:837420. DOI: 10.3389/fmed.2022.837420. PMID: 35265644. PMCID: PMC8899076.
Article30. Rudroff T, Fietsam AC, Deters JR, Bryant AD, Kamholz J. 2020; Post-COVID-19 fatigue: potential contributing factors. Brain Sci. 10:1012. DOI: 10.3390/brainsci10121012. PMID: 33352638. PMCID: PMC7766297.
Article31. Ceban F, Ling S, Lui LM, et al. 2022; Fatigue and cognitive impairment in post-COVID-19 syndrome: a systematic review and meta-analysis. Brain Behav Immun. 101:93–135. DOI: 10.1016/j.bbi.2021.12.020. PMID: 34973396. PMCID: PMC8715665.
Article32. Soares MN, Eggelbusch M, Naddaf E, et al. 2022; Skeletal muscle alterations in patients with acute COVID-19 and post-acute sequelae of Covid-19. J Cachexia Sarcopenia Muscle. 13:11–22. DOI: 10.1002/jcsm.12896. PMID: 34997689. PMCID: PMC8818659.
Article33. Jimeno-Almazán A, Franco-López F, Buendía-Romero Á, et al. 2022; Rehabilitation for post-COVID-19 condition through a supervised exercise intervention: a randomized controlled trial. Scand J Med Sci Sports. 32:1791–801. DOI: 10.1111/sms.14240. PMID: 36111386. PMCID: PMC9538729.34. Albu S, Rivas Zozaya N, Murillo N, García-Molina A, Figueroa Chacón CA, Kumru H. 2022; Multidisciplinary outpatient rehabilitation of physical and neurological sequelae and persistent symptoms of covid-19: a prospective, observational cohort study. Disabil Rehabil. 44:6833–40. DOI: 10.1080/09638288.2021.1977398. PMID: 34559592.
Article35. Calvo-Paniagua J, Díaz-Arribas MJ, Valera-Calero JA, et al. 2022; A tele-health primary care rehabilitation program improves self-perceived exertion in COVID-19 survivors experiencing Post-COVID fatigue and dyspnea: a quasi-experimental study. PLoS One. 17:e0271802. DOI: 10.1371/journal.pone.0271802. PMID: 35926004. PMCID: PMC9352012.
Article36. Nalbandian A, Desai AD, Wan EY. 2023; Post-COVID-19 condition. Annu Rev Med. 74:55–64. DOI: 10.1146/annurev-med-043021-030635. PMID: 35914765.
Article37. Long Q, Li J, Hu X, Bai Y, Zheng Y, Gao Z. 2021; Follow-ups on persistent symptoms and pulmonary function among post-acute COVID-19 patients: a systematic review and meta-analysis. Front Med (Lausanne). 8:702635. DOI: 10.3389/fmed.2021.702635. PMID: 34540862. PMCID: PMC8448290.
Article38. McNarry MA, Berg RM, Shelley J, et al. 2022; Inspiratory muscle training enhances recovery post-COVID-19: a randomised controlled trial. Eur Respir J. 60:2103101. DOI: 10.1183/13993003.03101-2021. PMID: 35236727. PMCID: PMC8900538.
Article39. Bouteleux B, Henrot P, Ernst R, et al. 2021; Respiratory rehabilitation for Covid-19 related persistent dyspnoea: a one-year experience. Respir Med. 189:106648. DOI: 10.1016/j.rmed.2021.106648. PMID: 34689061. PMCID: PMC8511554.
Article40. Soril LJ, Damant RW, Lam GY, et al. 2022; The effectiveness of pulmonary rehabilitation for post-COVID symptoms: a rapid review of the literature. Respir Med. 195:106782. DOI: 10.1016/j.rmed.2022.106782. PMID: 35272262. PMCID: PMC8887973.
Article41. Mazza MG, Palladini M, De Lorenzo R, et al. 2021; Persistent psychopathology and neurocognitive impairment in COVID-19 survivors: effect of inflammatory biomarkers at three-month follow-up. Brain Behav Immun. 94:138–47. DOI: 10.1016/j.bbi.2021.02.021. PMID: 33639239. PMCID: PMC7903920.
Article42. Tabacof L, Tosto-Mancuso J, Wood J, et al. 2022; Post-acute COVID-19 syndrome negatively impacts physical function, cognitive function, health-related quality of life, and participation. Am J Phys Med Rehabil. 101:48–52. DOI: 10.1097/PHM.0000000000001910. PMID: 34686631. PMCID: PMC8667685.
Article43. Daynes E, Gerlis C, Chaplin E, Gardiner N, Singh SJ. 2021; Early experiences of rehabilitation for individuals post-COVID to improve fatigue, breathlessness exercise capacity and cognition: a cohort study. Chron Respir Dis. 18:14799731211015691. DOI: 10.1177/14799731211015691. PMID: 33957805. PMCID: PMC8114752.44. Compagno S, Palermi S, Pescatore V, et al. 2022; Physical and psychological reconditioning in long COVID syndrome: results of an out-of-hospital exercise and psychological - based rehabilitation program. Int J Cardiol Heart Vasc. 41:101080. DOI: 10.1016/j.ijcha.2022.101080. PMID: 35854691. PMCID: PMC9286763.
Article45. Del Corral T, Fabero-Garrido R, Plaza-Manzano G, Fernández-de-Las-Peñas C, Navarro-Santana M, López-de-Uralde-Villanueva I. 2023; Home-based respiratory muscle training on quality of life and exercise tolerance in long-term post-COVID-19: randomized controlled trial. Ann Phys Rehabil Med. 66:101709. DOI: 10.1016/j.rehab.2022.101709. PMID: 36191860. PMCID: PMC9708524.
Article46. Durstenfeld MS, Sun K, Tahir P, et al. 2022; Use of cardiopulmonary exercise testing to evaluate long COVID-19 symptoms in adults: a systematic review and meta-analysis. JAMA Netw Open. 5:e2236057. DOI: 10.1001/jamanetworkopen.2022.36057. PMID: 36223120. PMCID: PMC9557896.47. Smer A, Squires RW, Bonikowske AR, Allison TG, Mainville RN, Williams MA. 2023; Cardiac complications of COVID-19 infection and the role of physical activity. J Cardiopulm Rehabil Prev. 43:8–14. DOI: 10.1097/HCR.0000000000000701. PMID: 35839441. PMCID: PMC9828583.
Article48. Gluckman TJ, Bhave NM, et al. Writing Committee. 2022; 2022 ACC expert consensus decision pathway on cardiovascular sequelae of COVID-19 in adults: myocarditis and other myocardial involvement, post-acute sequelae of SARS-CoV-2 infection, and return to play: a report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 79:1717–56. DOI: 10.1016/j.jacc.2022.02.003. PMID: 35307156. PMCID: PMC8926109.49. Blair SN, Kampert JB, Kohl HW 3rd, et al. 1996; Influences of cardiorespiratory fitness and other precursors on cardiovascular disease and all-cause mortality in men and women. JAMA. 276:205–10. DOI: 10.1001/jama.1996.03540030039029. PMID: 8667564.
Article50. Barbara C, Clavario P, De Marzo V, et al. 2022; Effects of exercise rehabilitation in patients with long coronavirus disease 2019. Eur J Prev Cardiol. 29:e258–60. DOI: 10.1093/eurjpc/zwac019. PMID: 35078233. PMCID: PMC8807301.
Article51. Teixeira DO Amaral V, Viana AA, et al. 2022; Cardiovascular, respiratory, and functional effects of home-based exercise training after COVID-19 hospitalization. Med Sci Sports Exerc. 54:1795–803. DOI: 10.1249/MSS.0000000000002977. PMID: 35714077.
Article52. Hayden MC, Limbach M, Schuler M, et al. 2021; Effectiveness of a three-week inpatient pulmonary rehabilitation program for patients after COVID-19: a prospective observational study. Int J Environ Res Public Health. 18:9001. DOI: 10.3390/ijerph18179001. PMID: 34501596. PMCID: PMC8430843.
Article53. Ahmed I, Inam AB, Belli S, Ahmad J, Khalil W, Jafar MM. 2022; Effectiveness of aerobic exercise training program on cardiorespiratory fitness and quality of life in patients recovered from COVID-19. Eur J Physiother. 24:358–63. DOI: 10.1080/21679169.2021.1909649.
Article54. Nopp S, Moik F, Klok FA, et al. 2022; Outpatient pulmonary rehabilitation in patients with long COVID improves exercise capacity, functional status, dyspnea, fatigue, and quality of life. Respiration. 101:593–601. DOI: 10.1159/000522118. PMID: 35203084. PMCID: PMC9059007.
Article55. Jimeno-Almazán A, Buendía-Romero Á, Martínez-Cava A, et al. 2023; Effects of a concurrent training, respiratory muscle exercise, and self-management recommendations on recovery from post-COVID-19 conditions: the RECOVE trial. J Appl Physiol (1985). 134:95–104. DOI: 10.1152/japplphysiol.00489.2022. PMID: 36476156. PMCID: PMC9829459.
Article56. Del Valle MF, Valenzuela J, Marzuca-Nassr GN, et al. 2022; Eight weeks of supervised pulmonary rehabilitation are effective in improving resting heart rate and heart rate recovery in severe COVID-19 patient survivors of mechanical ventilation. Medicina (Kaunas). 58:514. DOI: 10.3390/medicina58040514. PMID: 35454353. PMCID: PMC9028941.
Article57. Liu K, Zhang W, Yang Y, Zhang J, Li Y, Chen Y. 2020; Respiratory rehabilitation in elderly patients with COVID-19: a randomized controlled study. Complement Ther Clin Pract. 39:101166. DOI: 10.1016/j.ctcp.2020.101166. PMID: 32379637. PMCID: PMC7118596.
Article58. Hockele LF, Sachet Affonso JV, Rossi D, Eibel B. 2022; Pulmonary and functional rehabilitation improves functional capacity, pulmonary function and respiratory muscle strength in post COVID-19 patients: pilot clinical trial. Int J Environ Res Public Health. 19:14899. DOI: 10.3390/ijerph192214899. PMID: 36429613. PMCID: PMC9691070.
Article59. Palau P, Domínguez E, Gonzalez C, et al. 2022; Effect of a home-based inspiratory muscle training programme on functional capacity in postdischarged patients with long COVID: the InsCOVID trial. BMJ Open Respir Res. 9:e001439. DOI: 10.1136/bmjresp-2022-001439. PMID: 36549786. PMCID: PMC9791108.
Article60. Spruit MA, Singh SJ, Garvey C, et al. 2013; An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 188:e13–64. DOI: 10.1164/rccm.201308-1509ST. PMID: 24083859.61. Twomey R, DeMars J, Franklin K, Culos-Reed SN, Weatherald J, Wrightson JG. 2022; Chronic fatigue and postexertional malaise in people living with long COVID: an observational study. Phys Ther. 102:pzac005. DOI: 10.1093/ptj/pzac005. PMID: 35079817. PMCID: PMC9383197.
Article62. Chu L, Valencia IJ, Garvert DW, Montoya JG. 2018; Deconstructing post-exertional malaise in myalgic encephalomyelitis/chronic fatigue syndrome: a patient-centered, cross-sectional survey. PLoS One. 13:e0197811. DOI: 10.1371/journal.pone.0197811. PMID: 29856774. PMCID: PMC5983853.63. Fairbank R. 2023; Long COVID exercise trials proposed by NIH raise alarm. Nature. 616:228–9. DOI: 10.1038/d41586-023-00900-w. PMID: 37002390.
Article64. Wright J, Astill SL, Sivan M. 2022; The relationship between physical activity and long COVID: a cross-sectional study. Int J Environ Res Public Health. 19:5093. DOI: 10.3390/ijerph19095093. PMID: 35564488. PMCID: PMC9105041.
Article65. Larun L, Brurberg KG, Odgaard-Jensen J, Price JR. 2019; Exercise therapy for chronic fatigue syndrome. Cochrane Database Syst Rev. 10:CD003200. DOI: 10.1002/14651858.CD011040.pub2. PMCID: PMC6517214. PMID: 28444695.
Article66. DeMars J, Brown DA, Angelidis I, et al. 2023; What is safe long COVID rehabilitation? J Occup Rehabil. 33:227–30. DOI: 10.1007/s10926-022-10075-2. PMID: 36315323. PMCID: PMC9628454.
Article