Ann Hepatobiliary Pancreat Surg.
2023 Aug;27(3):264-270. 10.14701/ahbps.23-002.
Unconventional shunt surgery for non-cirrhotic portal hypertension in patients not suitable for proximal splenorenal shunt
- Affiliations
-
- 1Department of Surgical Gastroenterology, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry, India
- KMID: 2545720
- DOI: http://doi.org/10.14701/ahbps.23-002
Abstract
- Backgrounds/Aims
Proximal splenorenal shunt (PSRS) is a commonly performed procedure to decompress portal hypertension, in patients with refractory variceal bleed, especially in non-cirrhotic portal hypertension (NCPH). If conventional methods are hindered by any technical or pathological factors, alternative surgical techniques may be required. This study analyzes the effectiveness of various unconventional shunt surgeries performed for NCPH.
Methods
A retrospective analysis of NCPH patients who underwent unconventional shunt surgeries during the period July 2011 to June 2022 was conducted. All patients were followed up for a minimum of 12 months with doppler study of the shunt to assess shunt patency, and upper gastrointestinal endoscopy to evaluate the regression of varices.
Results
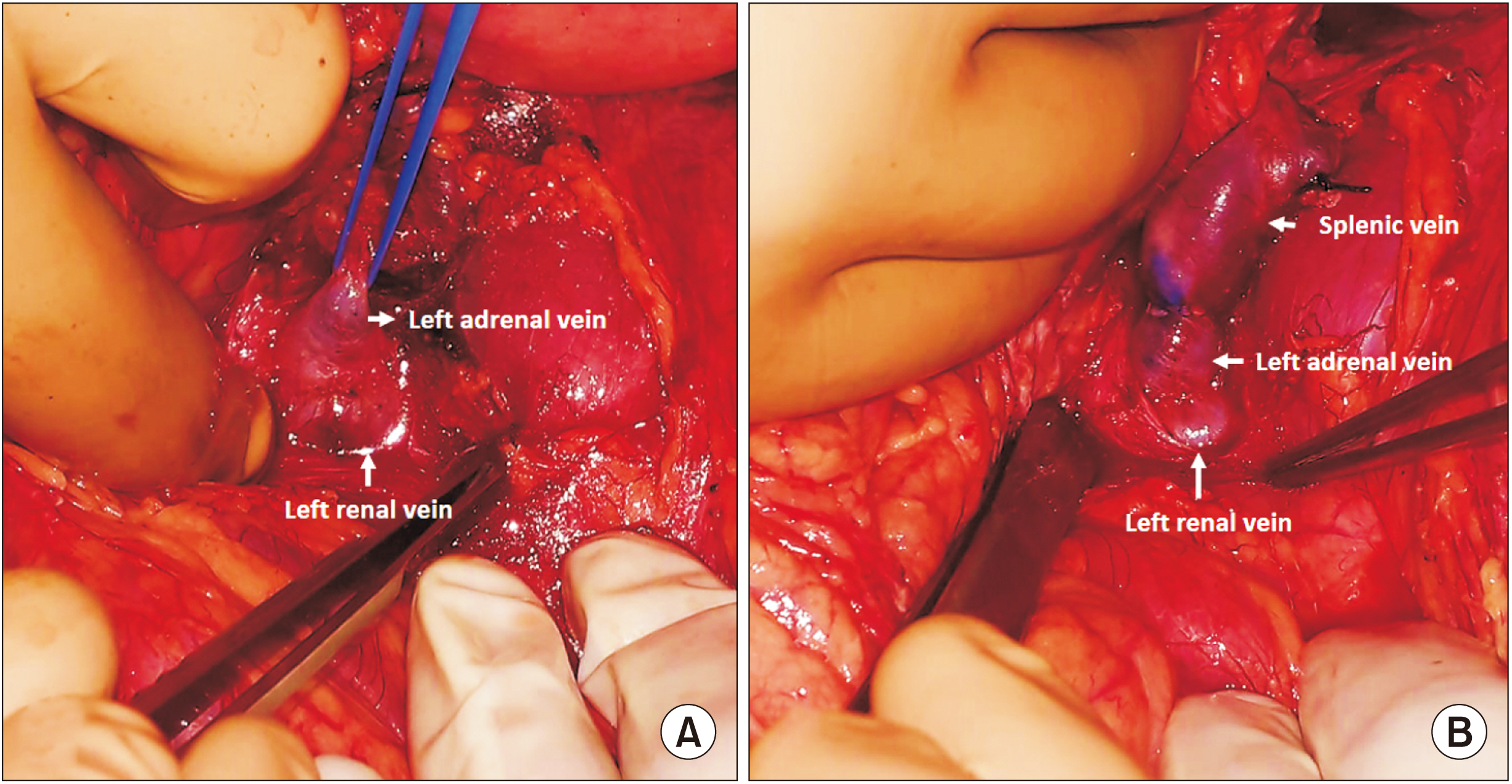
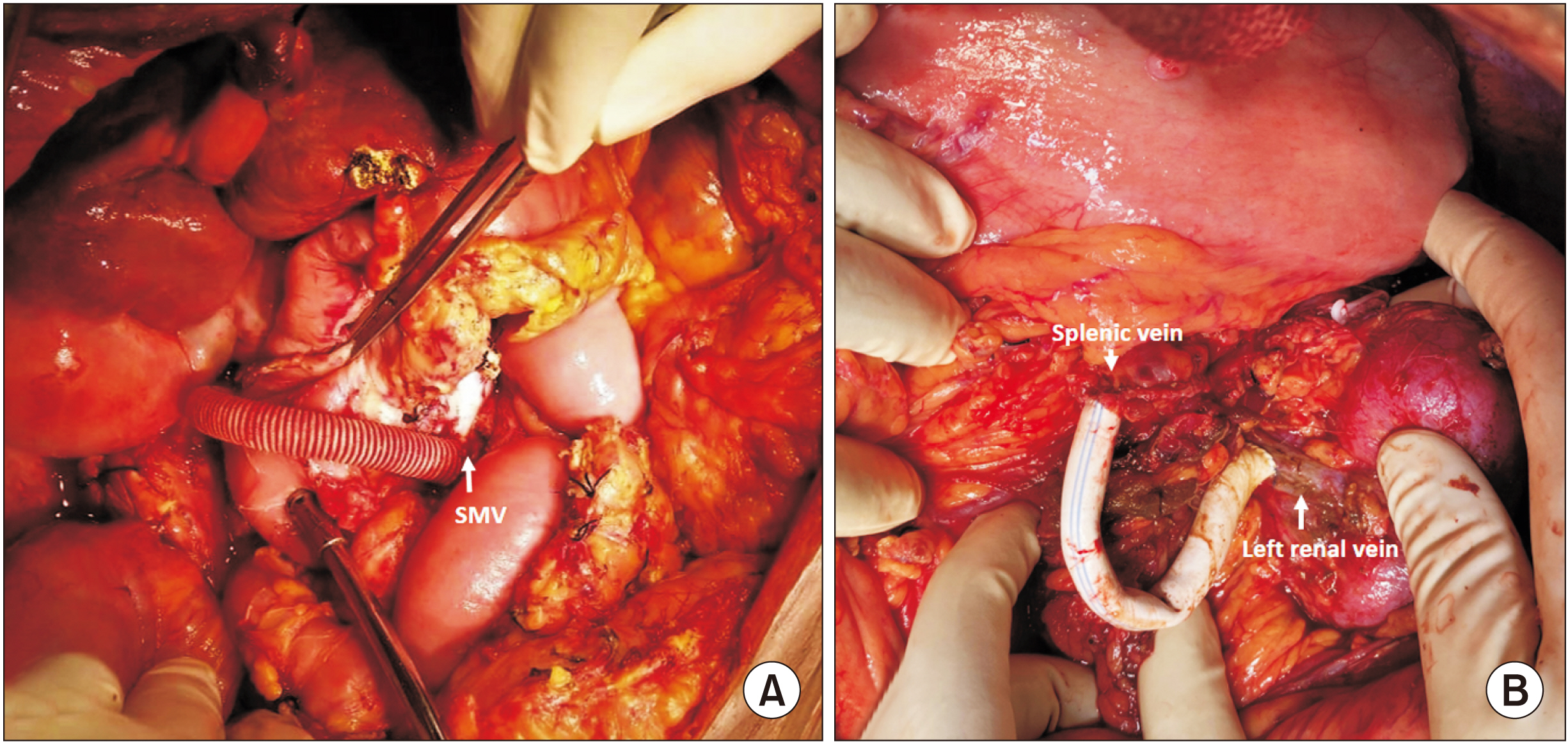
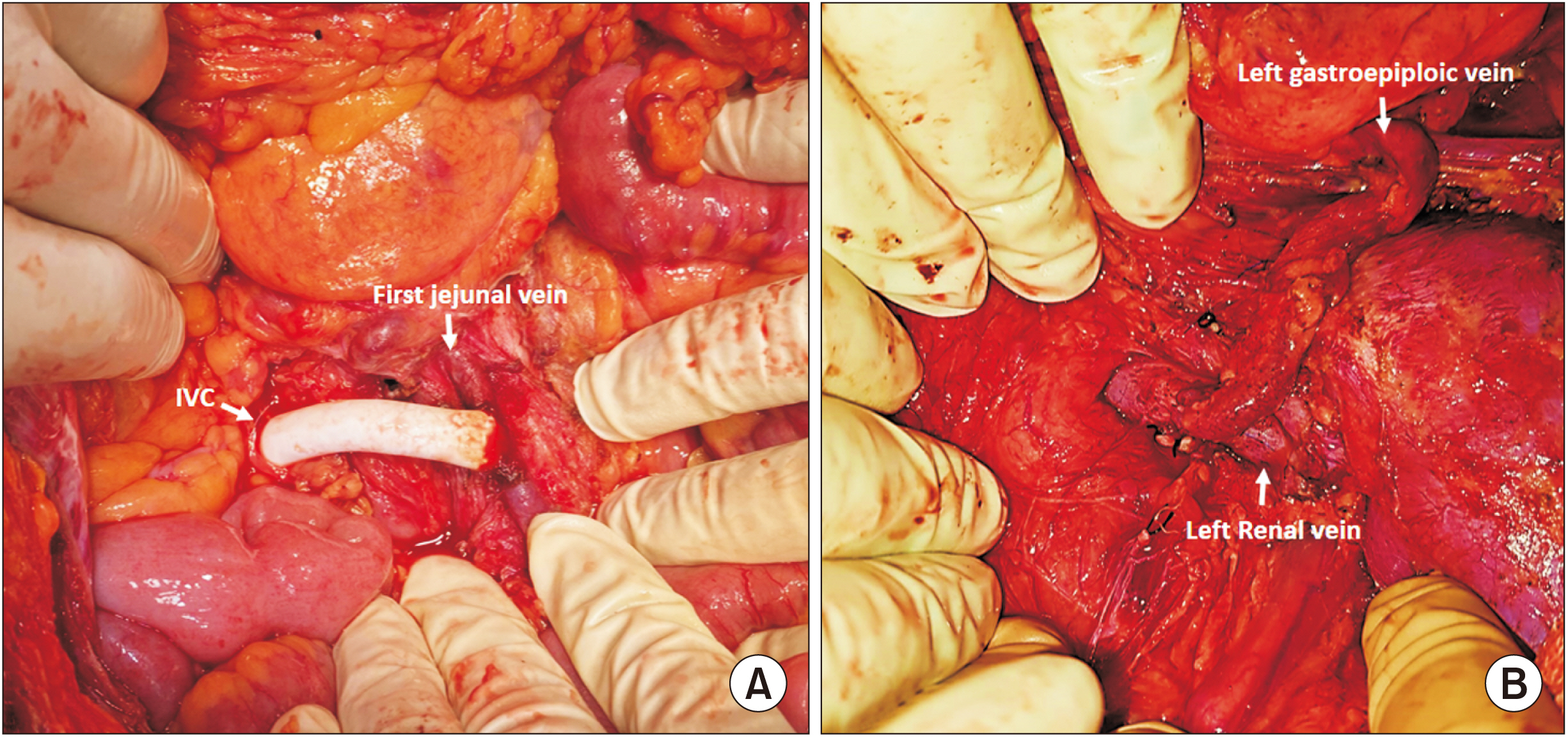
During the study period, 130 patients underwent shunt surgery; among these, 31 underwent unconventional shunts (splenoadrenal shunt [SAS], 12; interposition mesocaval shunt [iMCS], 8; interposition PSRS [iPSRS], 6; jejunal vein-cava shunt [JCS], 3; left gastroepiploic–renal shunt [LGERS], 2). The main indications for unconventional shunts were left renal vein aberration (SAS, 8/12), splenic vein narrowing (iMCS, 5/8), portalhypertensive vascular changes (iPSRS, 6/6), and portomesenteric thrombosis (JCS, 3/3). The median fall in portal pressure was more in SAS (12.1 mm Hg), and operative time more in JCS, 8.4 hours (range, 5–9 hours). During a median follow-up of 36 months (6–54 months), shunt thrombosis had been reported in all cases of LGERS, and less in SAS (3/12). Variceal regression rate was high in SAS, and least in LGERS. Hypersplenism had reversed in all patients, and 6/31 patients had a recurrent bleed.
Conclusions
Unconventional shunt surgery is effective in patients unsuited for other shunts, especially PSRS, and it achieves the desired effects in a significant proportion of patients.
Keyword
Figure
Reference
-
1. Sarin SK, Sachdev G, Nanda R. 1986; Follow-up of patients after variceal eradication. A comparison of patients with cirrhosis, noncirrhotic portal fibrosis, and extrahepatic obstruction. Ann Surg. 204:78–82. DOI: 10.1097/00000658-198607000-00011. PMID: 3729586. PMCID: PMC1251226.2. Poddar U, Thapa BR, Rao KL, Singh K. 2008; Etiological spectrum of esophageal varices due to portal hypertension in Indian children: is it different from the West? J Gastroenterol Hepatol. 23:1354–1357. DOI: 10.1111/j.1440-1746.2007.05102.x. PMID: 17683492.3. Prasad AS, Gupta S, Kohli V, Pande GK, Sahni P, Nundy S. 1994; Proximal splenorenal shunts for extrahepatic portal venous obstruction in children. Ann Surg. 219:193–196. DOI: 10.1097/00000658-199402000-00011. PMID: 8129490. PMCID: PMC1243121.4. Gupta S, Pottakkat B, Verma SK, Kalayarasan R, Chandrasekar A S, Pillai AA. 2020; Pathological abnormalities in splenic vasculature in non-cirrhotic portal hypertension: its relevance in the management of portal hypertension. World J Gastrointest Surg. 12:1–8. DOI: 10.4240/wjgs.v12.i1.1. PMID: 31984119. PMCID: PMC6943091.5. Linton RR, Jones CM, Volwiler W. 1947; Portal hypertension; the treatment by splenectomy and splenorenal anastomosis with preservation of the kidney. Surg Clin North Am. 27:1162–1170. DOI: 10.1016/S0039-6109(16)32244-7. PMID: 20266148.6. Mazariegos GV, Reyes J. 1998; A technique for distal splenoadrenal shunting in pediatric portal hypertension. J Am Coll Surg. 187:634–636. DOI: 10.1016/S1072-7515(98)00244-0. PMID: 9849740.7. Gu S, Chang S, Chu J, Xu M, Yan Z, Liu DC, et al. 2012; Spleno-adrenal shunt: a novel alternative for portosystemic decompression in children with portal vein cavernous transformation. J Pediatr Surg. 47:2189–2193. DOI: 10.1016/j.jpedsurg.2012.09.007. PMID: 23217874.8. Gupta S, Srinivas GV, Chandrasekar AS, Kalayarasan R, Pottakkat B. 2019; Splenoadrenal shunt for noncirrhotic portal hypertension. Indian J Surg. 81:28–31. DOI: 10.1007/s12262-017-1706-z.9. Drapanas T. 1972; Interposition mesocaval shunt for treatment of portal hypertension. Ann Surg. 176:435–448. DOI: 10.1097/00000658-197210000-00001. PMID: 4263236. PMCID: PMC1355426.10. Drapanas T, LoCicero J 3rd, Dowling JB. 1975; Hemodynamics of the interposition mesocaval shunt. Ann Surg. 181:523–533. DOI: 10.1097/00000658-197505000-00004. PMID: 124159. PMCID: PMC1345527.11. Nyman UR, Semba CP, Chang H, Hoffman C, Dake MD. 1996; Percutaneous creation of a mesocaval shunt. J Vasc Interv Radiol. 7:769–773. DOI: 10.1016/S1051-0443(96)70847-3. PMID: 8897349.12. Moriarty JM, Kokabi N, Kee ST. 2012; Transvenous creation of a mesocaval shunt: report of use in the management of extrahepatic portal vein occlusion. J Vasc Interv Radiol. 23:565–567. DOI: 10.1016/j.jvir.2011.09.023. PMID: 22464719.13. Barman AA, Batiuchok W, Chaudry SS, Creedon JJ. 1981; Use of interposed polytetrafluorethylene (PTFE) graft in distal splenorenal shunt. Cardiovasc Dis. 8:555–557. PMID: 15216183. PMCID: PMC288001.14. Biju P, Midha K, Gupta S, Kalayarasan R, Gnanasekaran S. 2019; proximal splenorenal shunt in a rare renal vein anomaly: a case report. Cureus. 25:e4754. DOI: 10.7759/cureus.4754. PMID: 31363436. PMCID: PMC6663117.15. Sarfeh IJ, Rypins EB, Conroy RM, Mason GR. 1983; Portacaval H-graft: relationships of shunt diameter, portal flow patterns and encephalopathy. Ann Surg. 197:422–426. DOI: 10.1097/00000658-198304000-00008. PMID: 6600914. PMCID: PMC1352755.16. Ellis DS, Linton RR, Jones CM. 1956; Effect of venous-shunt surgery on liver function in patients with portal hypertension; a follow-up study of 125 patients operated on in the last ten years. N Engl J Med. 254:931–936. DOI: 10.1056/NEJM195605172542002. PMID: 13322188.17. Warren WD, Henderson JM, Millikan WJ, Galambos JT, Bryan FC. 1988; Management of variceal bleeding in patients with noncirrhotic portal vein thrombosis. Ann Surg. 207:623–634. DOI: 10.1097/00000658-198805000-00017. PMID: 3259859. PMCID: PMC1493505.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Distal pancreatectomy with splenorenal shunt to preserve spleen in a cirrhotic patient
- Epidural Analgesia in a Parturient following Splenorenal Shunt Operation for Liver Cirrhosis
- Use of caudal pancreatectomy as a novel adjunct procedure to proximal splenorenal shunt in patients with noncirrhotic portal hypertension: A retrospective cohort study
- Analysis of a Distal Splenorenal Shunt for Treatment of Variceal Bleeding
- Splenectomy with endotherapy in non-cirrhotic portal fibrosis related portal hypertension: Can it be an alternative to proximal spleno-renal shunt?