Cost-Effectiveness of Active Surveillance Compared to Early Surgery of Small Papillary Thyroid Cancer: A Retrospective Study on a Korean Population
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Surgery, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Healthcare Group, Lee & Ko, Seoul, Korea
- 4Department of Family Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2545542
- DOI: http://doi.org/10.3346/jkms.2023.38.e264
Abstract
- Background
Recently, active surveillance (AS) has been introduced as an alternative to early surgery (ES) for the management of papillary thyroid microcarcinoma (PTMC), because of its indolent features and low mortality. However, its cost effects have not been determined and the findings of current studies differ, according to each country’s medical system.
Methods
A Markov model was constructed to compare the cost-effectiveness of AS and ES, based on a reference case of a 40-year-old patient diagnosed with PTMC. Costs and transition probabilities were derived from previous clinical studies in Korean populations, and the incremental cost-effectiveness ratio (ICER) and net monetary benefit (NMB) were calculated. The willingness-to-pay (WTP) threshold was set at USD 100,000 per quality-adjusted life year (QALY) gained. Sensitivity analyses were conducted to address the uncertainties in the model’s variables.
Results
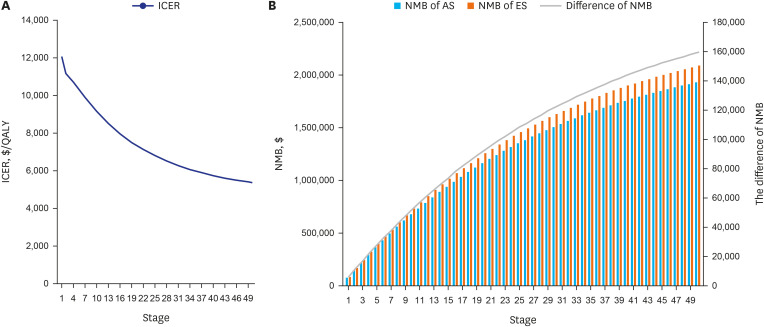
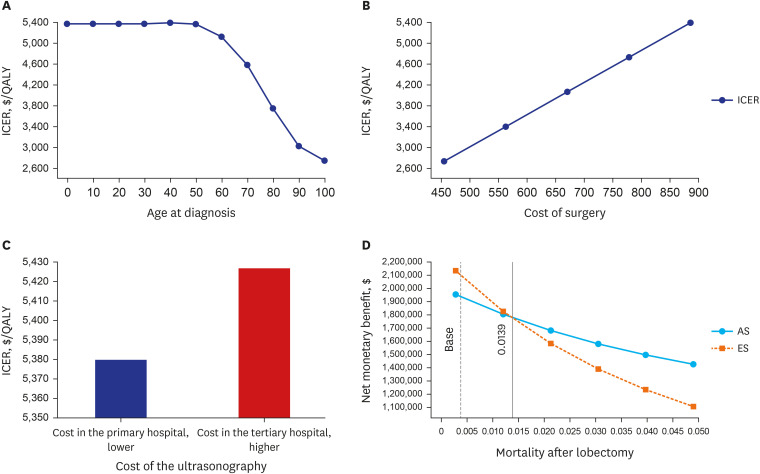
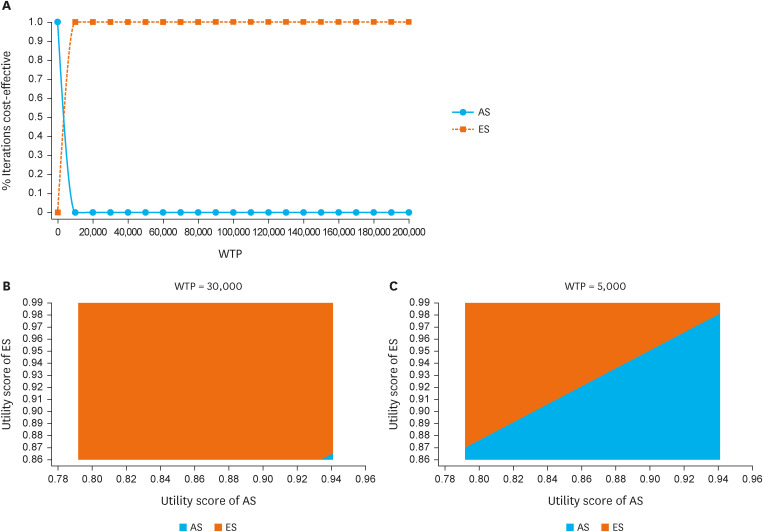
From the base scenario, the cumulative costs and effectiveness were both higher in ES than AS. The ICER for ES, compared with AS, was USD 6,619.86/QALY, lower than the set WTP. The NMB difference between AS and ES increased across the stages (USD 5,980 at the first stage and USD 159,667 at the last stage). The ICER increased along with decreasing age and increasing cost of surgery. The higher the ES utility score and the lower that of AS, the more cost-effective ES, with WTP set at USD 30,000.
Conclusion
In the current Korean medical system, ES is more cost-effective than AS. ES is more cost-effective as it is diagnosed at young age and followed-up for a long time.
Keyword
Figure
Cited by 3 articles
-
Cost-Utility Analysis of Early Detection with Ultrasonography of Differentiated Thyroid Cancer: A Retrospective Study on a Korean Population
Han-Sang Baek, Jeonghoon Ha, Kwangsoon Kim, Ja Seong Bae, Jeong Soo Kim, Sungju Kim, Dong-Jun Lim, Chul-Min Kim
Endocrinol Metab. 2024;39(2):310-323. doi: 10.3803/EnM.2023.1870.Korean Thyroid Association Management Guidelines for Patients with Thyroid Nodules 2024
Young Joo Park, Eun Kyung Lee, Young Shin Song, Su Hwan Kang, Bon Seok Koo, Sun Wook Kim, Dong Gyu Na, Seung-Kuk Baek, So Won Oh, Min Kyoung Lee, Sang-Woo Lee, Young Ah Lee, Yong Sang Lee, Ji Ye Lee, Dong-Jun Lim, Leehi Joo, Yuh-Seog Jung, Chan Kwon Jung, Yoon Young Cho, Yun Jae Chung, Won Bae Kim, Ka Hee Yi, Ho-Cheol Kang, Do Joon Park
Int J Thyroidol. 2024;17(1):208-244. doi: 10.11106/ijt.2024.17.1.208.Korean Thyroid Association Guidelines on the Management of Differentiated Thyroid Cancers; Part I. Initial Management of Differentiated Thyroid Cancers - Chapter 2. Surgical Management of Thyroid Cancer 2024
Yoon Young Cho, Cho Rok Lee, Ho-Cheol Kang, Bon Seok Koo, Hyungju Kwon, Sun Wook Kim, Won Woong Kim, Jung-Han Kim, Dong Gyu Na, Young Joo Park, Kyorim Back, Young Shin Song, Seung Hoon Woo, Ho-Ryun Won, Chang Hwan Ryu, Jee Hee Yoon, Min Kyoung Lee, Eun Kyung Lee, Joon-Hyop Lee, Ji Ye Lee, Dong-Jun Lim, Jae-Yol Lim, Yun Jae Chung, Chan Kwon Jung, Jun-Ook Park, Hee Kyung Kim
Int J Thyroidol. 2024;17(1):30-52. doi: 10.11106/ijt.2024.17.1.30.
Reference
-
1. Hong S, Won YJ, Park YR, Jung KW, Kong HJ, Lee ES, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2017. Cancer Res Treat. 2020; 52(2):335–350. PMID: 32178489.
Article2. Davies L, Welch HG. Current thyroid cancer trends in the United States. JAMA Otolaryngol Head Neck Surg. 2014; 140(4):317–322. PMID: 24557566.
Article3. Choi YM, Lee J, Kwak MK, Jeon MJ, Kim TY, Hong EG, et al. Recent changes in the incidence of thyroid cancer in Korea between 2005 and 2018: analysis of Korean national data. Endocrinol Metab (Seoul). 2022; 37(5):791–799. PMID: 36220137.
Article4. Jeon EJ, Jeong YJ, Park SH, Cho CH, Shon HS, Jung ED. Ultrasonographic characteristics of the follicular variant papillary thyroid cancer according to the tumor size. J Korean Med Sci. 2016; 31(3):397–402. PMID: 26955240.
Article5. Uppal N, Cunningham Nee Lubitz C, James B. The cost and financial burden of thyroid cancer on patients in the US: a review and directions for future research. JAMA Otolaryngol Head Neck Surg. 2022; 148(6):568–575. PMID: 35511135.
Article6. Ito Y, Miyauchi A, Kihara M, Higashiyama T, Kobayashi K, Miya A. Patient age is significantly related to the progression of papillary microcarcinoma of the thyroid under observation. Thyroid. 2014; 24(1):27–34. PMID: 24001104.
Article7. Ahn HS, Kim HJ, Welch HG. Korea’s thyroid-cancer “epidemic”--screening and overdiagnosis. N Engl J Med. 2014; 371(19):1765–1767. PMID: 25372084.
Article8. Jung CK, Bae JS, Park YJ. Re-increasing trends in thyroid cancer incidence after a short period of decrease in Korea: reigniting the debate on ultrasound screening. Endocrinol Metab (Seoul). 2022; 37(5):816–818. PMID: 36220136.
Article9. Baek HS, Jeong CH, Ha J, Bae JS, Kim JS, Lim DJ, et al. Cost-effectiveness analysis of active surveillance compared to early surgery in small papillary thyroid cancer: a systemic review. Cancer Manag Res. 2021; 13:6721–6730. PMID: 34471385.
Article10. Boltz MM, Hollenbeak CS, Schaefer E, Goldenberg D, Saunders BD. Attributable costs of differentiated thyroid cancer in the elderly Medicare population. Surgery. 2013; 154(6):1363–1369. PMID: 23973115.
Article11. Kim K, Choi JY, Kim SJ, Lee EK, Lee YK, Ryu JS, et al. Active surveillance versus immediate surgery for low-risk papillary thyroid microcarcinoma patients in South Korea: a cost-minimization analysis from the MAeSTro study. Thyroid. 2022; 32(6):648–656. PMID: 35570657.
Article12. Gupta N, Verma R, Dhiman RK, Rajsekhar K, Prinja S. Cost-effectiveness analysis and decision modelling: a tutorial for clinicians. J Clin Exp Hepatol. 2020; 10(2):177–184. PMID: 32189934.
Article13. Kuntz K, Sainfort F, Butler M, Taylor B, Kulasingam S, Gregory S, et al. Decision and Simulation Modeling in Systematic Reviews. Methods Research Report. (Prepared by the University of Minnesota Evidence-based Practice Center under Contract No. 290-2007-10064-I.) AHRQ Publication No. 11(13)-EHC037-EF. Rockville, MD, USA: Agency for Healthcare Research and Quality;2013.14. Korea National Cancer Center. Cancer statistics according to age. Accessed January 30, 2023. https://www.cancer.go.kr/ .15. Zhang HS, Lee EK, Jung YS, Nam BH, Jung KW, Kong HJ, et al. Total thyroidectomy’s association with survival in papillary thyroid cancers and the high proportion of total thyroidectomy in low-risk patients: analysis of Korean nationwide data. Surgery. 2019; 165(3):629–636. PMID: 30342774.
Article16. Korea National Statistics Office. Life table. Updated 2022. Accessed January 30, 2023. https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B42&conn_path=I2 .17. Health Insurance Review & Assessment Service. 2021 Economic evaluation guidelines in medicine and drugs. Updated 2021. Accessed January 30, 2023. https://www.hira.or.kr/ebooksc/ebook_630/ebook_630_202103150917443810.pdf .18. Bertram MY, Lauer JA, De Joncheere K, Edejer T, Hutubessy R, Kieny MP, et al. Cost-effectiveness thresholds: pros and cons. Bull World Health Organ. 2016; 94(12):925–930. PMID: 27994285.
Article19. Health Insurance Review & Assessment Service. Medical fee schedule of health service in Korea under national health insurance coverage. Updated 2021. Accessed January 30, 2023. https://www.hira.or.kr/bbsDummy.do?pgmid=HIRAA020002000100&brdScnBltNo=4&brdBltNo=9105 .20. Kwon H, Jeon MJ, Kim WG, Park S, Kim M, Song DE, et al. A comparison of lobectomy and total thyroidectomy in patients with papillary thyroid microcarcinoma: a retrospective individual risk factor-matched cohort study. Eur J Endocrinol. 2017; 176(4):371–378. PMID: 28089996.
Article21. Jeon YW, Gwak HG, Lim ST, Schneider J, Suh YJ. Long-term prognosis of unilateral and multifocal papillary thyroid microcarcinoma after unilateral lobectomy versus total thyroidectomy. Ann Surg Oncol. 2019; 26(9):2952–2958. PMID: 31264119.
Article22. Kim SK, Park I, Woo JW, Lee JH, Choe JH, Kim JH, et al. Total thyroidectomy versus lobectomy in conventional papillary thyroid microcarcinoma: analysis of 8,676 patients at a single institution. Surgery. 2017; 161(2):485–492. PMID: 27593085.
Article23. Oh HS, Ha J, Kim HI, Kim TH, Kim WG, Lim DJ, et al. Active surveillance of low-risk papillary thyroid microcarcinoma: a multi-center cohort study in Korea. Thyroid. 2018; 28(12):1587–1594. PMID: 30226447.
Article24. Houten R, Fleeman N, Kotas E, Boland A, Lambe T, Duarte R. A systematic review of health state utility values for thyroid cancer. Qual Life Res. 2021; 30(3):675–702. PMID: 33098494.
Article25. Jones E, Epstein D, García-Mochón L. A procedure for deriving formulas to convert transition rates to probabilities for multistate Markov models. Med Decis Making. 2017; 37(7):779–789. PMID: 28379779.
Article26. Pyo J, Ock M, Park B, Kim NE, Choi EJ, Park H, et al. Meaning and status of health-related quality of life recognized by medical professionals: a qualitative study. J Korean Med Sci. 2021; 36(3):e20. PMID: 33463094.
Article27. Lang BH, Wong CK. A cost-effectiveness comparison between early surgery and non-surgical approach for incidental papillary thyroid microcarcinoma. Eur J Endocrinol. 2015; 173(3):367–375. PMID: 26104754.
Article28. Venkatesh S, Pasternak JD, Beninato T, Drake FT, Kluijfhout WP, Liu C, et al. Cost-effectiveness of active surveillance versus hemithyroidectomy for micropapillary thyroid cancer. Surgery. 2017; 161(1):116–126. PMID: 27839930.
Article29. White C, Weinstein MC, Fingeret AL, Randolph GW, Miyauchi A, Ito Y, et al. Is less more? A microsimulation model comparing cost-effectiveness of the revised American Thyroid Association’s 2015 to 2009 guidelines for the management of patients with thyroid nodules and differentiated thyroid cancer. Ann Surg. 2020; 271(4):765–773. PMID: 30339630.
Article30. Oda H, Miyauchi A, Ito Y, Sasai H, Masuoka H, Yabuta T, et al. Comparison of the costs of active surveillance and immediate surgery in the management of low-risk papillary microcarcinoma of the thyroid. Endocr J. 2017; 64(1):59–64. PMID: 27667647.
Article31. Lin JF, Jonker PK, Cunich M, Sidhu SB, Delbridge LW, Glover AR, et al. Surgery alone for papillary thyroid microcarcinoma is less costly and more effective than long term active surveillance. Surgery. 2020; 167(1):110–116. PMID: 31543327.
Article32. Youssef MR, Attia AS, Omar M, Aboueisha M, Freeman MN, Shama M, et al. Thyroid lobectomy as a cost-effective approach in low-risk papillary thyroid cancer versus active surveillance. Surgery. 2022; 171(1):190–196. PMID: 34384606.
Article33. Ernst R. Indirect costs and cost-effectiveness analysis. Value Health. 2006; 9(4):253–261. PMID: 16903995.
Article34. Neumann PJ, Cohen JT, Weinstein MC. Updating cost-effectiveness--the curious resilience of the $50,000-per-QALY threshold. N Engl J Med. 2014; 371(9):796–797. PMID: 25162885.
Article35. Jeon MJ, Lee YM, Sung TY, Han M, Shin YW, Kim WG, et al. Quality of life in patients with papillary thyroid microcarcinoma managed by active surveillance or lobectomy: a cross-sectional study. Thyroid. 2019; 29(7):956–962. PMID: 31038017.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Review of Active Surveillance of Papillary Thyroid Microcarcinoma
- Active Surveillance of Papillary Thyroid Microcarcinoma: A Mini-Review from Korea
- Active Surveillance for Low-Risk Papillary Thyroid Carcinoma as an Acceptable Management Option with Additional Benefits: A Comprehensive Systematic Review
- Active Surveillance of Papillary Thyroid Cancer: Past, Present, and Future
- Risk Factors for Tumor Size Increase During Active Surveillance of Papillary Thyroid Cancer: Meta-Analysis and Systematic Review