Arch Hand Microsurg.
2023 Sep;28(3):137-149. 10.12790/ahm.23.0016.
Current concepts in traumatic mallet finger management
- Affiliations
-
- 1Department of Orthopedic Surgery, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 2Department of Orthopedic Surgery, Yonsei University School of Medicine, Seoul, Korea
- 3Department of Orthopedic Surgery, Korea University Anam Hospital, Seoul, Korea
- KMID: 2545524
- DOI: http://doi.org/10.12790/ahm.23.0016
Abstract
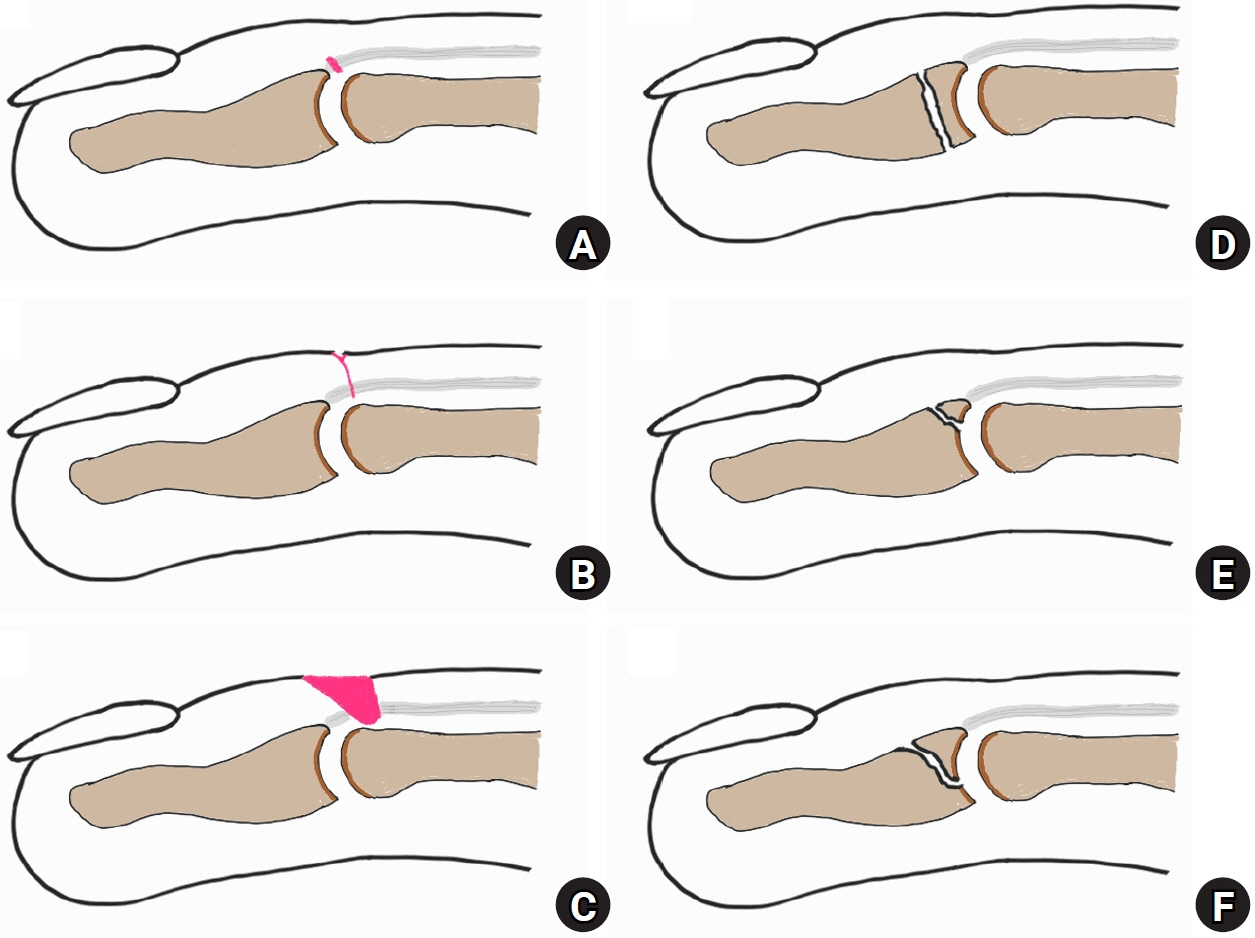
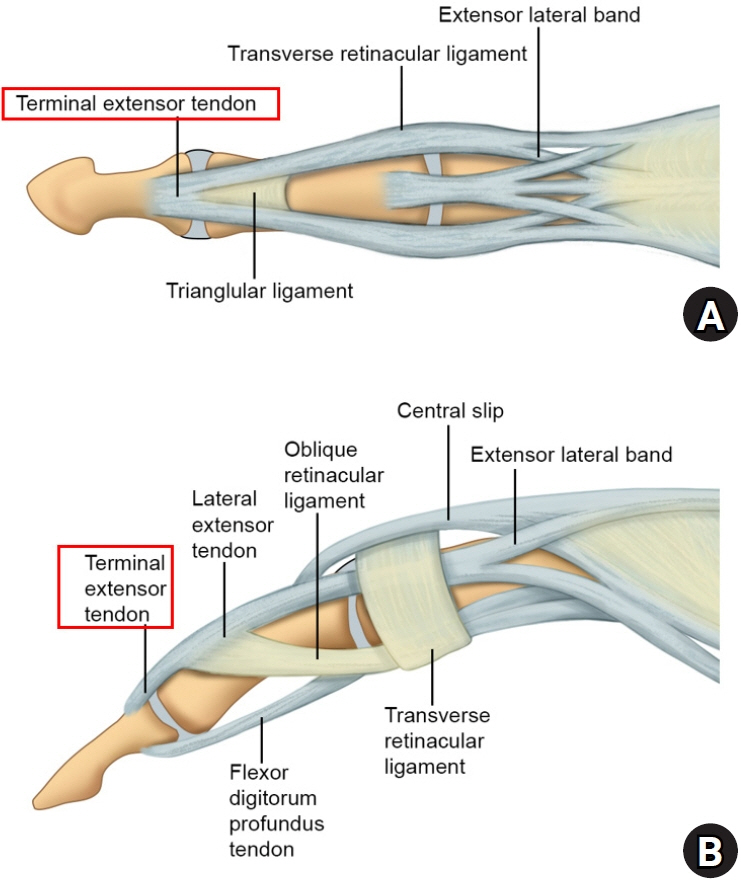
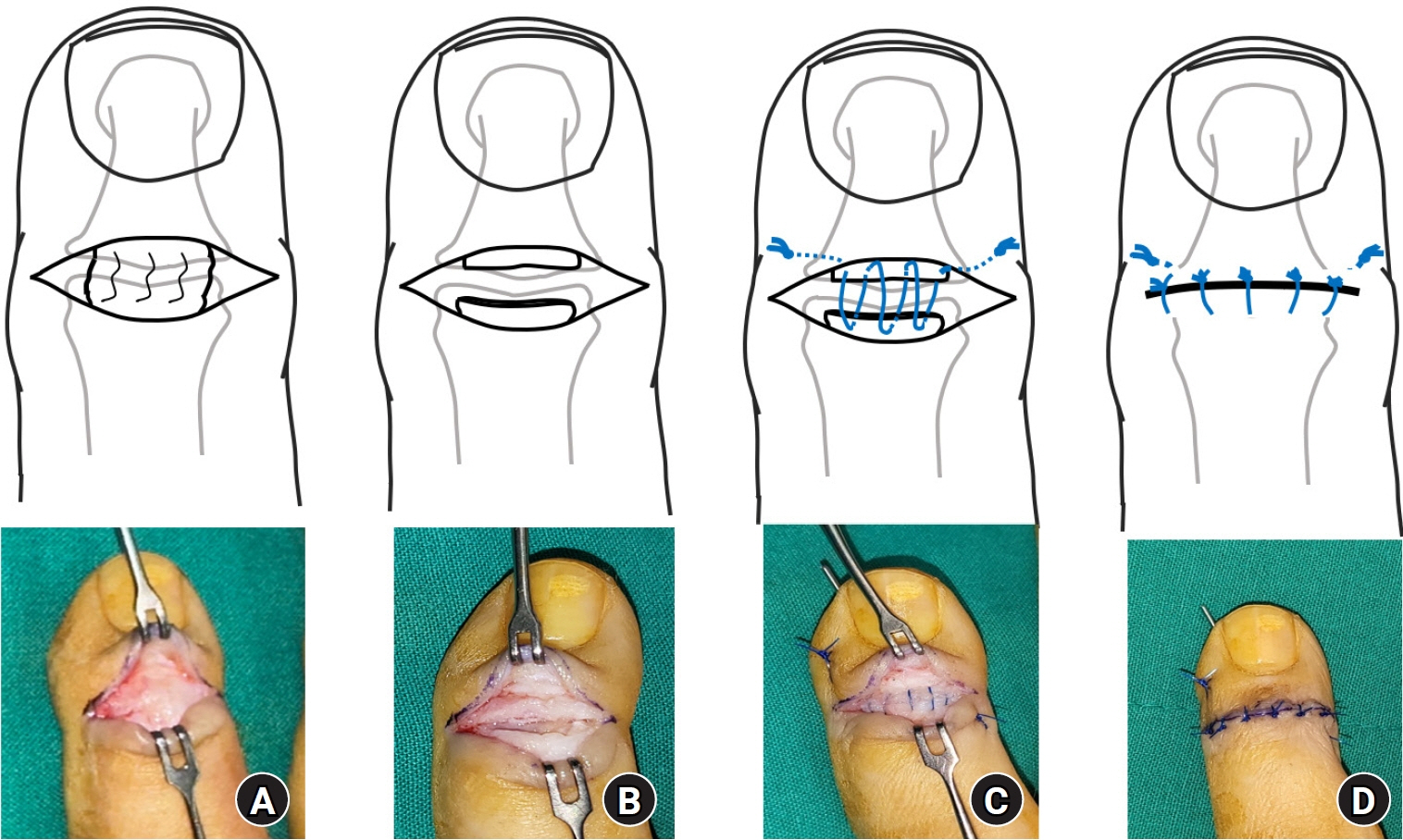
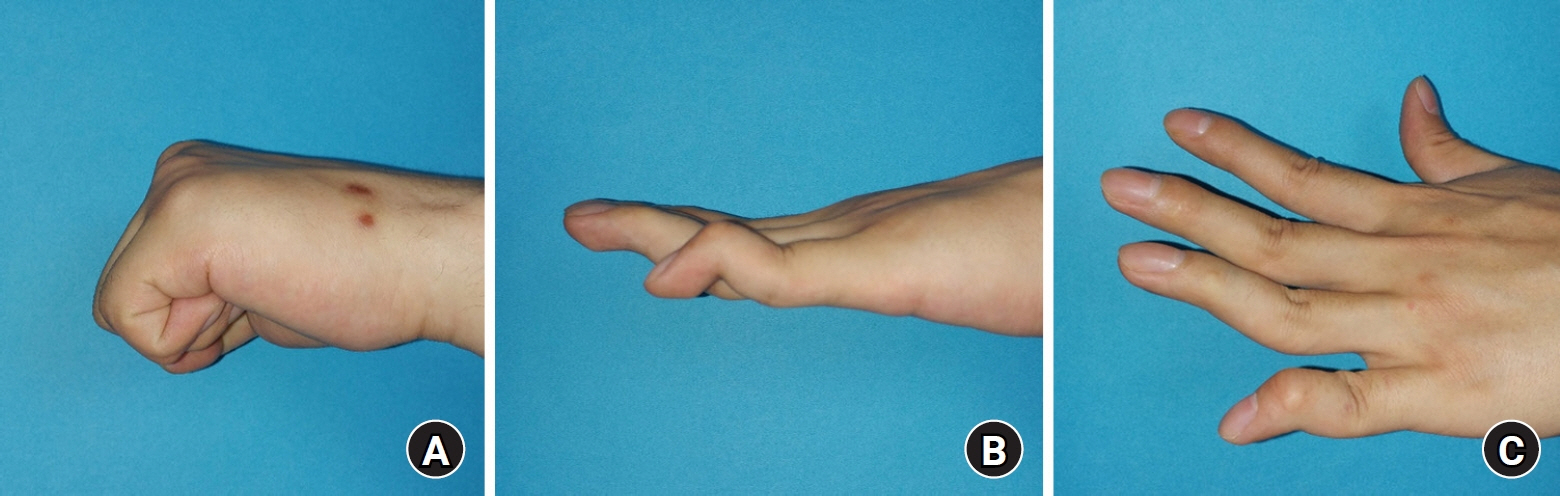
- Mallet finger deformities can be divided into tendinous deformities caused by tendon rupture and bony deformities caused by fracture. In many cases, conservative treatment is possible. The goal of treating traumatic mallet finger deformities is to accurately restore the ruptured tendon or fractured bone to its proper position, correct extension lag or flexion contracture, prevent joint arthritis, and restore the full range of motion through appropriate range of motion exercises at the right time. In cases of tendinous mallet finger, immobilization with a splint or cast for at least 6 weeks in the extended position is required. During this period, flexion at the distal interphalangeal joint should be strictly limited, while movement at the proximal interphalangeal joint is allowed. Patient compliance with the protocol is essential for achieving good treatment outcomes. If conservative treatment fails or if the deformity recurs after initial surgery, satisfactory results can be achieved through tenodermodesis surgery. If the bony mallet finger involves a bone fragment of 3 mm or more or subluxation of the distal phalanx, surgical treatment is recommended. The primary surgical treatment involves closed reduction and percutaneous pinning with the extension block technique.
Keyword
Figure
Reference
-
References
1. Sivakumar BS, Graham DJ, Ledgard JP, Lawson RD. Acute mallet finger injuries: a review. J Hand Surg Am. 2023; 48:283–91.2. Clayton RA, Court-Brown CM. The epidemiology of musculoskeletal tendinous and ligamentous injuries. Injury. 2008; 39:1338–44.
Article3. Strauch RJ. Extensor tendon injury. In : Wolfe SW, Pederson WC, Kozin SH, Cohen MS, editors. Green's operative hand surgery. 8th ed. Philadelphia, PA: Elsevier Health Sciences;2021. p. 182–211.4. King HJ, Shin SJ, Kang ES. Complications of operative treatment for mallet fractures of the distal phalanx. J Hand Surg Br. 2001; 26:28–31.
Article5. Facca S, Nonnenmacher J, Liverneaux P. Treatment of mallet finger with dorsal nail glued splint: retrospective analysis of 270 cases. Rev Chir Orthop Reparatrice Appar Mot. 2007; 93:682–9.6. Giddins G. Mallet finger: two different injuries. Hand Clin. 2022; 38:281–8.7. Peng C, Huang RW, Chen SH, et al. Comparative outcomes between surgical treatment and orthosis splint for mallet finger: a systematic review and meta-analysis. J Plast Surg Hand Surg. 2023; 57:54–63.
Article8. Salazar Botero S, Hidalgo Diaz JJ, Benaïda A, Collon S, Facca S, Liverneaux PA. Review of acute traumatic closed mallet finger injuries in adults. Arch Plast Surg. 2016; 43:134–44.
Article9. Schweitzer TP, Rayan GM. The terminal tendon of the digital extensor mechanism: part I, anatomic study. J Hand Surg Am. 2004; 29:898–902.
Article10. Schweitzer TP, Rayan GM. The terminal tendon of the digital extensor mechanism: part II, kinematic study. J Hand Surg Am. 2004; 29:903–8.
Article11. Shum C, Bruno RJ, Ristic S, Rosenwasser MP, Strauch RJ. Examination of the anatomic relationship of the proximal germinal nail matrix to the extensor tendon insertion. J Hand Surg Am. 2000; 25:1114–7.
Article12. Pike J, Mulpuri K, Metzger M, Ng G, Wells N, Goetz T. Blinded, prospective, randomized clinical trial comparing volar, dorsal, and custom thermoplastic splinting in treatment of acute mallet finger. J Hand Surg Am. 2010; 35:580–8.
Article13. Nashi N, Sebastin SJ. A pragmatic and evidence-based approach to mallet finger. J Hand Surg Asian Pac Vol. 2021; 26:319–32.
Article14. Hong IT, Baek E, Ha C, Han SH. Long-term Stack splint immobilization for closed tendinous Mallet Finger. Handchir Mikrochir Plast Chir. 2020; 52:170–5.
Article15. Brush M, Dick NR, Rohman EM, Bohn DC. Comparison of orthosis management failure rates for mallet injuries. J Hand Surg Glob Online. 2022; 4:220–5.
Article16. Duarte A. Optimising the conservative management of closed tendinous mallet finger injury. Emerg Nurse. 2020; 28:35–40.
Article17. Toci GR, Tecce ER, Katt BM, Aita D, Beredjiklian PK, Fletcher D. Splinting versus percutaneous pinning for the treatment of soft tissue mallet finger: a retrospective cohort analysis. J Hand Surg Asian Pac Vol. 2022; 27:952–6.
Article18. Lucchina S, Meroni M, Molitor M, Guidi M. Finger amputation after pinning of the distal interphalangeal joint for acute closed tendinous mallet finger: a rare but devastating complication. J Hand Surg Asian Pac Vol. 2022; 27:590–3.
Article19. Velez ML, Medina MA, Lopez RP, Morales HL, Ordoñez RH. Stack splinting versus Kirschner wire treatment in acute closed mallet finger Doyle I. Plast Surg (Oakv). 2022; 30:117–21.
Article20. Garberman SF, Diao E, Peimer CA. Mallet finger: results of early versus delayed closed treatment. J Hand Surg Am. 1994; 19:850–2.
Article21. Iselin F, Levame J, Godoy J. A simplified technique for treating mallet fingers: tenodermodesis. J Hand Surg Am. 1977; 2:118–21.
Article22. Kon M, Bloem JJ. Treatment of mallet fingers by tenodermodesis. Hand. 1982; 14:174–5.
Article23. Sorene ED, Goodwin DR. Tenodermodesis for established mallet finger deformity. Scand J Plast Reconstr Surg Hand Surg. 2004; 38:43–5.
Article24. Kardestuncer T, Bae DS, Waters PM. The results of tenodermodesis for severe chronic mallet finger deformity in children. J Pediatr Orthop. 2008; 28:81–5.
Article25. Foucher G, Binhamer P, Cange S, Lenoble E. Long-term results of splintage for mallet finger. Int Orthop. 1996; 20:129–31.26. Feehan LM, Sheps SB. Incidence and demographics of hand fractures in British Columbia, Canada: a population-based study. J Hand Surg Am. 2006; 31:1068–74.
Article27. Lange RH, Engber WD. Hyperextension mallet finger. Orthopedics. 1983; 6:1426–31.
Article28. Husain SN, Dietz JF, Kalainov DM, Lautenschlager EP. A biomechanical study of distal interphalangeal joint subluxation after mallet fracture injury. J Hand Surg Am. 2008; 33:26–30.
Article29. Wehbé MA, Schneider LH. Mallet fractures. J Bone Joint Surg Am. 1984; 66:658–69.
Article30. Okafor B, Mbubaegbu C, Munshi I, Williams DJ. Mallet deformity of the finger: five-year follow-up of conservative treatment. J Bone Joint Surg Br. 1997; 79:544–7.31. Trickett RW, Brock J, Shewring DJ. The non-operative management of bony mallet injuries. J Hand Surg Eur Vol. 2021; 46:460–5.
Article32. Handoll HH, Vaghela MV. Interventions for treating mallet finger injuries. Cochrane Database Syst Rev. 2004; (3):CD004574.
Article33. Niechajev IA. Conservative and operative treatment of mallet finger. Plast Reconstr Surg. 1985; 76:580–5.
Article34. Thillemann JK, Thillemann TM, Kristensen PK, Foldager-Jensen AD, Munk B. Splinting versus extension-block pinning of bony mallet finger: a randomized clinical trial. J Hand Surg Eur Vol. 2020; 45:574–81.35. Ishiguro T, Inoue K, Matsubayashi T, Ito T, Hashizume N. A new method of closed reduction for mallet fractures. J Jpn Soc Surg Hand. 1988; 5:444–7.36. Lee YH, Kim JY, Chung MS, Baek GH, Gong HS, Lee SK. Two extension block Kirschner wire technique for mallet finger fractures. J Bone Joint Surg Br. 2009; 91:1478–81.
Article37. Lee SK, Kim KJ, Yang DS, Moon KH, Choy WS. Modified extension-block K-wire fixation technique for the treatment of bony mallet finger. Orthopedics. 2010; 33:728.
Article38. Yamanaka K, Sasaki T. Treatment of mallet fractures using compression fixation pins. J Hand Surg Br. 1999; 24:358–60.
Article39. Lee SH, Lee JE, Lee KH, Pyo SH, Kim MB, Lee YH. Supplemental method for reduction of irreducible mallet finger fractures by the 2-extension block technique: the dorsal counterforce technique. J Hand Surg Am. 2019; 44:695.
Article40. Suzuki T, Iwamoto T, Matsumura N, et al. Causes of procedural failures of closed reductions using an extension-block pin for bony mallet finger. J Hand Microsurg. 2021; 13:69–74.
Article41. Pegoli L, Toh S, Arai K, Fukuda A, Nishikawa S, Vallejo IG. The Ishiguro extension block technique for the treatment of mallet finger fracture: indications and clinical results. J Hand Surg Br. 2003; 28:15–7.42. Wang WC, Hsu CE, Yeh CW, Ho TY, Chiu YC. Functional outcomes and complications of hook plate for bony mallet finger: a retrospective case series study. BMC Musculoskelet Disord. 2021; 22:281.
Article43. Lin JS, Samora JB. Surgical and nonsurgical management of mallet finger: a systematic review. J Hand Surg Am. 2018; 43:146–63.
Article44. Lamaris GA, Matthew MK. The diagnosis and management of mallet finger injuries. Hand (N Y). 2017; 12:223–8.
Article45. Takase F, Yamasaki K, Kokubu T, Mifune Y, Inui A, Kuroda R. Treatment of chronic bony mallet fingers by dorsal extension block pinning with percutaneous curettage. Case Rep Orthop. 2018; 2018:7297951.
Article46. Murray PM. Treatment of the osteoarthritic hand and thumb. In : Wolfe SW, Pederson WC, Kozin SH, Cohen MS, editors. Green's operative hand surgery. 8th ed. Philadelphia, PA: Elsevier Health Sciences;2021. p. 345–72.47. Han SH, Cha YS, Song WT. Arthrodesis of distal interphalangeal joints in the hand with interosseous wiring and intramedullary K-wire fixation. Clin Orthop Surg. 2014; 6:401–4.
Article48. Lee JK, Lee S, Choi S, et al. Distal interphalangeal joint arthrodesis using only Kirschner wires in small distal phalanges. Handchir Mikrochir Plast Chir. 2021; 53:462–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multiple Bony Mallet on the Same Hand
- Prognostic Factors of the Extension Block Technique for the Bony Mallet Finger
- The Surgical Treatment of the Mallet Finger Deformity Due to Extensor Tendon Injury in Children
- "Delta(Delta) wire Technique" for Bony Mallet Finger: Surgical Technique
- Review of Acute Traumatic Closed Mallet Finger Injuries in Adults