J Korean Neurosurg Soc.
2023 Sep;66(5):591-597. 10.3340/jkns.2022.0190.
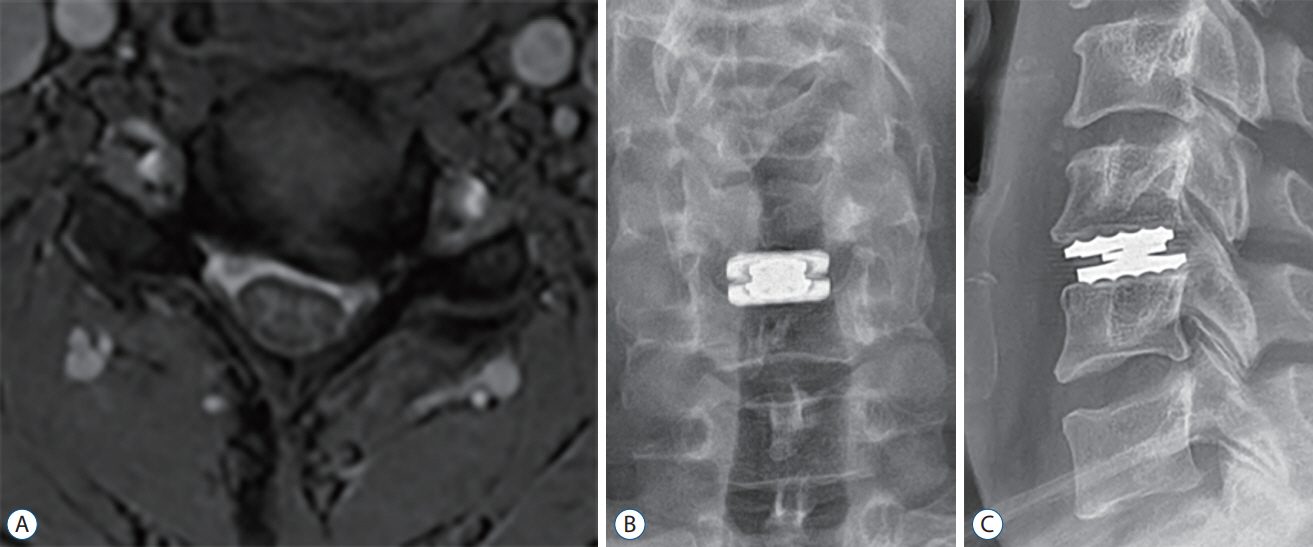
Cervical Myelopathy Induced by Posterior Vertebral Body Osteolysis after Cervical Disc Arthroplasty
- Affiliations
-
- 1Department of Neurosurgery, Kyung Hee University Hospital, Kyung Hee University College of Medicine, Seoul, Korea
- KMID: 2545350
- DOI: http://doi.org/10.3340/jkns.2022.0190
Abstract
- Cervical disc arthroplasty (CDA) has become more widespread and diverges from the conventional technique used in anterior cervical fusion for cervical degenerative disc disease. As arthroplasty has become a popular treatment option, few complications have been reported in the literature. These include subsidence, expulsion, posterior avulsion fractures, heterotopic ossification, and osteolysis. One of the critical complications is osteolysis, but current studies on this subject are limited in terms of not elucidating the incidence, etiology, and consequences. The authors present two cases, who presented with clinical signs of gradually worsening myelopathy induced by posterior vertebral body osteolysis, 2 years after CDA. Subsequently, the patient underwent posterior decompression and fusion without prosthesis removal. Postoperatively, the clinical symptoms gradually resolved, with no severe deficits. The present rare cases highlight the osteolysis that occurs after CDA, which can cause cervical myelopathy, and suggest spine surgeons to be alert to this fatal complication.
Keyword
Figure
Reference
-
References
1. Chang PY, Wu JC, Mayo BC, Massel DH, Wang MY. Heterotopic ossification in cervical disc arthroplasty. Contemp Spine Surg. 18:1–5. 2017.2. Chen TY, Chen WH, Tzeng CY, Huang CW, Yang CC, Chen HT, et al. Anterior bone loss after cervical Bryan disc arthroplasty: insight into the biomechanics following total disc replacement. Spine J. 20:1211–1218. 2020.3. Gao F, Mao T, Sun W, Guo W, Wang Y, Li Z, et al. An updated meta-analysis comparing artificial cervical disc arthroplasty (CDA) versus anterior cervical discectomy and fusion (ACDF) for the treatment of cervical degenerative disc disease (CDDD). Spine (Phila Pa 1976). 40:1816–1823. 2015.4. Gawkrodger DJ. Metal sensitivities and orthopaedic implants revisited: the potential for metal allergy with the new metal-on-metal joint prostheses. Br J Dermatol. 148:1089–1093. 2003.5. Granchi D, Cenni E, Giunti A, Baldini N. Metal hypersensitivity testing in patients undergoing joint replacement: a systematic review. J Bone Joint Surg Br. 94:1126–1134. 2012.6. Hacker FM, Babcock RM, Hacker RJ. Very late complications of cervical arthroplasty: results of 2 controlled randomized prospective studies from a single investigator site. Spine (Phila Pa 1976). 38:2223–2226. 2013.7. Hisey MS, Zigler JE, Jackson R, Nunley PD, Bae HW, Kim KD, et al. Prospective, randomized comparison of one-level mobi-C cervical total disc replacement vs. anterior cervical discectomy and fusion: results at 5-year follow-up. Int J Spine Surg. 10:10. 2016.8. Hsu JE, Bumgarner RE, Matsen FA 3rd. Propionibacterium in shoulder arthroplasty: what we think we know today. J Bone Joint Surg Am. 98:597–606. 2016.9. Joaquim AF, Lee NJ, Lehman RA Jr, Tumialán LM, Riew KD. Osteolysis after cervical disc arthroplasty. Eur Spine J. 29:2723–2733. 2020.10. Kieser DC, Cawley DT, Fujishiro T, Mazas S, Boissière L, Obeid I, et al. Risk factors for anterior bone loss in cervical disc arthroplasty. J Neurosurg Spine. 29:123–129. 2018.11. Kieser DC, Cawley DT, Fujishiro T, Tavolaro C, Mazas S, Boissiere L, et al. Anterior bone loss in cervical disc arthroplasty. Asian Spine J. 13:13–21. 2019.12. Kim SH, Chung YS, Ropper AE, Min KH, Ahn TK, Won KS, et al. Bone loss of the superior adjacent vertebral body immediately posterior to the anterior flange of Bryan cervical disc. Eur Spine J. 24:2872–2879. 2015.13. Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 40-A:607–624. 1958.14. Tumialán LM, Gluf WM. Progressive vertebral body osteolysis after cervical disc arthroplasty. Spine (Phila Pa 1976). 36:E973–E978. 2011.15. Wenger M, Markwalder TM. Heterotopic ossification associated with myelopathy following cervical disc prosthesis implantation. J Clin Neurosci. 26:154–156. 2016.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Atypical Heterotopic Bone Formation Rear to the Functioning Cervical Artificial Disc Prosthesis Causing Cervical Spondylotic Myelopathy
- Vertebral Body Sliding Osteotomy for Cervical Myelopathy With Rigid Kyphosis
- Anterior Decompression and Fusion for the Treatment of Cervical Myelopathy Caused by Ossification of the Posterior Longitudinal Ligament: A Narrative Review
- Guillain-Barre Syndrome Combined with Acute Cervical Myelopathy
- Cervical Myelopathy Following Intervertebral Disc Herniation at the Surgical Site Post-Cervical Artificial Disc Replacement Surgery