J Korean Med Sci.
2023 Aug;38(32):e246. 10.3346/jkms.2023.38.e246.
Development of Items for Transitional Care Service and Outcome Indicators of Discharged Patients for Improvement in Quality of Care
- Affiliations
-
- 1Department of Health Policy and Management, School of Medicine, Kangwon National University, Chuncheon, Korea
- 2Department of Preventive Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea
- 3Department of Preventive Medicine, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2545198
- DOI: http://doi.org/10.3346/jkms.2023.38.e246
Abstract
- Background
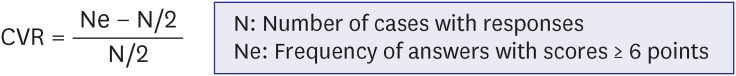
In this study, with the aim of improving the quality of transitional care service for discharged patients, the Health Care Quality and Outcomes Indicators of the Organization for Economic Co-operation and Development and National Health Service Outcomes Framework of the UK were applied to derive service items for provision and develop evaluation indicators under categories of effectiveness, safety, and patient-centeredness. Method: A scoping review was conducted to derive core concepts and evidence materials/data for transitional care service. For the derived items of transitional care service and evaluation indicators, a three-round Delphi study was conducted with experts in the fields of healthcare/ medicine/nursing/social welfare.
Results
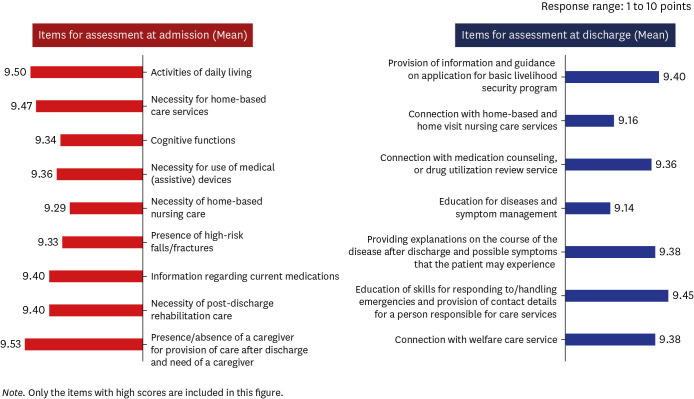
First, as a result of the scoping review, components of transitional care service (assessment of need by period of transitional care service, multi-professional team, connection to community resources, etc.) and themes for outcome indicators (effectiveness, patient safety, patient-centeredness) were derived. Second, by classifying the items for assessment according to the hospitalization and transition period and conducting a Delphi study to derive service items for transitional care service, during the hospitalization period, presence/absence of a caregiver and need for a caregiver, activities of daily living, and necessity for home-based care services were identified as items of high priority. Regarding patient safety, risk of falls and fractures during hospitalization, and necessity for medication reconciliation were identified as the items of high importance. For the transition period, provision of education regarding adequate responses and handling of emergencies, provision of information and guidance on application of services for basic livelihood security program beneficiaries, and education for patient skills in self-management of health were derived as items of high priority. Third, for the derivation of outcome indicators for transitional care service, in the “effectiveness” category, the experts rated a reduction in the 30-day readmission rate as an item of high importance along with a decrease in emergency department visits, reduction in preventable admissions as indicators of high relevance. In terms of “patient safety,” a decrease in drug adverse reactions, and reduction in the incidence of falls and pressure ulcers were identified as indicators of high priority. Finally, for the category of “patient-centeredness,” patient experience assessment, level of service satisfaction reported by patients and their caregivers, and reducing burden on caregivers were identified as indicators of high priority.
Conclusion
This study suggest practical implications for the service with high relevance and necessity for transitional period. It also presented outcome indicators of transitional care service to contribute toward an improvement in the quality of care.
Figure
Reference
-
1. Weeks LE, Barber B, MacDougall ES, Macdonald M, Martin-Misener R, Warner G. An exploration of Canadian transitional care programs for older adults. Healthc Manage Forum. 2020; 34(3):163–168. PMID: 33272058.2. Boyd CM, Ricks M, Fried LP, Guralnik JM, Xue QL, Xia J, et al. Functional decline and recovery of activities of daily living in hospitalized, disabled older women: the Women’s Health and Aging Study I. J Am Geriatr Soc. 2009; 57(10):1757–1766. PMID: 19694869.3. Greenwald J, Denham C, Jack B. The hospital discharge: a review of a high risk care transition with highlights of a reengineered discharge process. J Patient Saf. 2007; 3(2):97–106.4. Wu HY, Sahadevan S, Ding YY. Factors associated with functional decline of hospitalised older persons following discharge from an acute geriatric unit. Ann Acad Med Singapore. 2006; 35(1):17–23. PMID: 16470269.5. Covinsky KE, Palmer RM, Fortinsky RH, Counsell SR, Stewart AL, Kresevic D, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc. 2003; 51(4):451–458. PMID: 12657063.6. Boo EH, Oh IO, Kim SA, Son JE, Yoon MS, Park HH, et al. A study on the future nursing management of discharged patients in comprehensive nursing service. Goyang, Korea: NHIS Ilsan Hospital;2016. p. 1–121.7. Heim N, Rolden H, van Fenema EM, Weverling-Rijnsburger AW, Tuijl JP, Jue P, et al. The development, implementation and evaluation of a transitional care programme to improve outcomes of frail older patients after hospitalisation. Age Ageing. 2016; 45(5):643–651. PMID: 27298381.8. Ministry of Health and Welfare of South Korea. Updated 2019. Accessed May 20, 2022. http://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&page=2&CONT_SEQ=351474&SEARCHKEY=DEPT_NM&SEARCHVALUE=%EA%B3%B5%EA%B3%B5%EC%9D%98%EB%A3%8C%EA%B3%BC .9. Ministry of Health and Welfare of South Korea. Updated 2020. Accessed October 4, 2022. https://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&page=1&CONT_SEQ=362387 .10. Health Insurance Review and Assessment Service. Updated 2021. Accessed October 4, 2022. https://www.hira.or.kr/bbsDummy.do?brdScnBltNo=4&brdBltNo=10262&pgmid=HIRAA020041000100#none .11. Qiu L, Kumar S, Sen A, Sinha AP. Impact of the Hospital Readmission Reduction Program on hospital readmission and mortality: an economic analysis. Prod Oper Manag. 2022; 31(5):2341–2360.12. Khera R, Wang Y, Bernheim SM, Lin Z, Krumholz HM. Post-discharge acute care and outcomes following readmission reduction initiatives: national retrospective cohort study of Medicare beneficiaries in the United States. BMJ. 2020; 368:l6831. PMID: 31941686.13. Naylor MD, Aiken LH, Kurtzman ET, Olds DM, Hirschman KB. The care span: the importance of transitional care in achieving health reform. Health Aff (Millwood). 2011; 30(4):746–754. PMID: 21471497.14. Baldonado A, Hawk O, Ormiston T, Nelson D. Transitional care management in the outpatient setting. BMJ Qual Improv Rep. 2017; 6(1):u212974.w5206.15. Yoshimura M, Sumi N. Measurement tools that assess the quality of transitional care from patients’ perspective: a literature review. Jpn J Nurs Sci. 2022; 19(3):e12472. PMID: 35132783.16. Naylor M, Keating SA. Transitional care. Am J Nurs. 2008; 108(9):Suppl. 58–63.17. Organization for Economic Co-operation and Development. Healthcare quality and outcomes indicators. Updated 2021. Accessed October 4, 2022. https://www.oecd.org/health/health-care-quality-outcomes-indicators.htm .18. UK National Health Service. Guidance: NHS outcomes framework 2011 to 2012. Updated 2010. Accessed October 4, 2022. https://www.gov.uk/government/publications/nhs-outcomes-framework-2011-to-2012 .19. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005; 8(1):19–32.20. Yoon MS. A three-round Delphi study on current & future competencies of secretary. J Secr Stud. 2003; 12(2):109–141.21. Wheeler FD. The theory and practice of feminist-informed family therapy: a Delphi study (women, gender) [dissertation]. West Lafayette, IN, USA: Purdue University;1985.22. Lawshe CH. A quantitative approach to content validity. Person Psychol. 1975; 28(4):563–575.23. Konkuk University Medical Center. Development of Senior Specific Citizen Oriented Health Care Service System Based on Korean 48/6 Model. Sejong, Korea: Ministry of Health and Welfare;2018. p. 1–895.24. Health Insurance Review and Assessment Service. Guidelines for Pilot Projects for Community-Linked Activities and Support for Discharge of Acute Patients. Sejong, Korea: Ministry of Health and Welfare;2020. p. 1–49.25. Chiquet C, Maurin M, Thuret G, Benito Y, Cornut PL, Creuzot-Garcher C, et al. Analysis of diluted vitreous samples from vitrectomy is useful in eyes with severe acute postoperative endophthalmitis. Ophthalmology. 2009; 116(12):2437–2441.e1. PMID: 19815283.26. Khalandi F, Yoldashkhan M, Bana Derakhshan H, Nasiri M. Disability in activities of daily living after discharge from the cardiac care unit: a cross-sectional study. Evid Based Care. 2020; 9(4):48–52.27. Kwon IS, Eun Y. Cancer patients require home care after. J Korean Acad Nurs. 1999; 29(4):743–754.28. Dronina Y, Kim SK, Jo HS. Predictors of the need for post-discharge transitional care services in older adults: a cross-sectional analysis. J Korean Gerontol Soc. 2022; 42(4):787–803.29. Kim EJ. Nursing needs analysis of elderly female patients with liver cancer. Asia Pac J Multimed Serv Converg Art Humanit Sociol. 2018; 8(6):667–674.30. Hong JS, Lee GE. Scale development of job stress for home care nurses. J Korean Acad Nurs. 2004; 34(6):1097–1107.31. Hwang MS, Park HY, Jang SJ. Difficulties and coping experienced by advanced practice nurses in home health nursing field. J Korean Acad Community Health Nurs. 2020; 31(2):143–155.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Development of the Quality Indicators in Long Term Care Service
- Development and Application of Nursing Service Quality Indicators in Nursing Homes
- Development of an Evaluation Tool for the Nursing Care Quality by 4GL
- Present Status of Papers on the Primary Care Quality Assessment in Korea
- Implementation of a care coordination system for chronic diseases