Ann Surg Treat Res.
2023 Aug;105(2):76-81. 10.4174/astr.2023.105.2.76.
Atypical parathyroid tumor: clinical and parathyroid hormone response to surgical treatment
- Affiliations
-
- 1Thoracic Surgery Unit, Department of Surgical Sciences, Santa Maria della Misericordia University Hospital, University of Perugia Medical School, Perugia, Italy
- 2Endocrine Surgery Unit, Department of Surgical Sciences, Santa Maria University Hospital, University of Perugia Medical School, Terni, Italy
- 3Department of Surgery, Policlinico Umberto I, Sapienza University of Rome, Roma, Italy
- KMID: 2545158
- DOI: http://doi.org/10.4174/astr.2023.105.2.76
Abstract
- Purpose
Primary hyperparathyroidism (PHPT) is caused by typical adenoma (TA), multiglandular disease (MD), or parathyroid carcinoma (PC), and in a smaller percentage of cases by atypical parathyroid tumor (APT). The objective of this study is the retrospective analysis of clinical features and parathyroid hormone (PTH)/calcium response to surgery in patients who underwent parathyroidectomy for symptomatic PHPT with histological evidence of APT.
Methods
We retrospectively reviewed our institutional experience in the management of PHPT from January 2016 to December 2021 focusing on those patients presenting APTs. We analyzed the clinical features of this disease and PTH/ calcium response to surgical treatment in APTs compared to the other pathological conditions causing PHPT.
Results
In a cohort of 125 patients with PHPT we found 112 TAs (89.6%), 6 APTs (4.8%), 6 PCs (4.8%), and only 1 MD (0.8%). APTs in comparison to other parathyroid diseases showed peculiar features such as adhesion to the surrounding structures and a frequent intrathyroidal location, which may justify thyroid loboistmectomy adopted in most of the observed cases. APTs showed significantly higher preoperative PTH values compared to TA + MD and were relevant to PC.
Conclusion
Due to its rarity, there is a lack of specific indications in the management of APTs. Biochemical features observed in APT and PC can be related to similar biological behavior. However, some specific features observed preoperatively in some cases of PHPT might suggest presence of an APT, which could be helpful mostly in surgical and postoperative management. Further studies are required to confirm the results of the present preliminary report.
Keyword
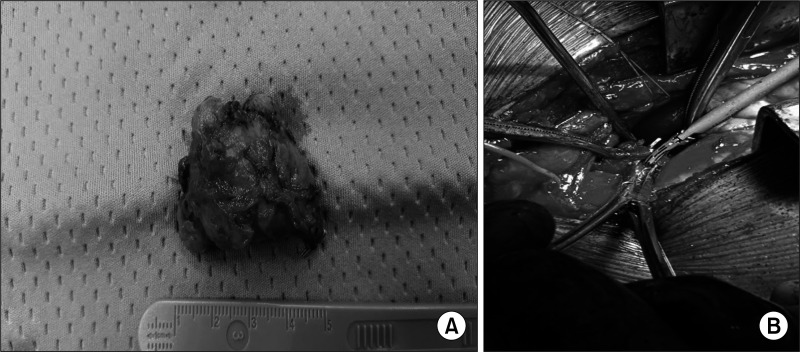
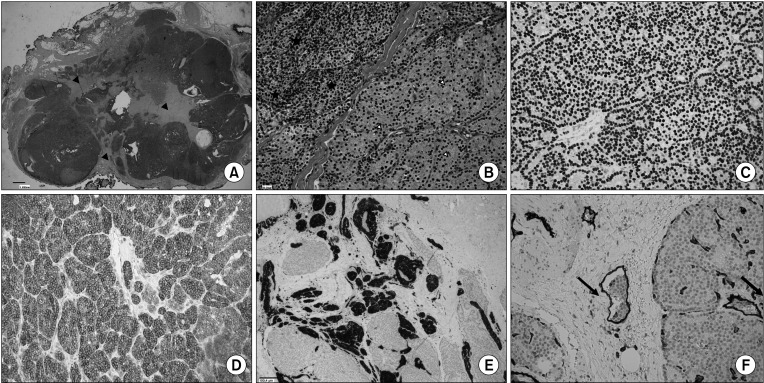
Figure
Reference
-
1. Vaira V, Verdelli C, Forno I, Corbetta S. MicroRNAs in parathyroid physiopathology. Mol Cell Endocrinol. 2017; 456:9–15. PMID: 27816765.
Article2. Saponaro F, Cetani F, Repaci A, Pagotto U, Cipriani C, Pepe J, et al. Clinical presentation and management of patients with primary hyperparathyroidism in Italy. J Endocrinol Invest. 2018; 41:1339–1348. PMID: 29616419.
Article3. Aldinger KA, Hickey RC, Ibanez ML, Samaan NA. Parathyroid carcinoma: a clinical study of seven cases of functioning and two cases of nonfunct ioning parathyroid cancer. Cancer. 1982; 49:388–397. PMID: 7053835.
Article4. Bilezikian JP, Bandeira L, Khan A, Cusano NE. Hyperparathyroidism. Lancet. 2018; 391:168–178. PMID: 28923463.
Article5. Gasser RW. Clinical aspects of primary hyperparathyroidism: clinical manifestations, diagnosis, and therapy. Wien Med Wochenschr. 2013; 163:397–402. PMID: 23990260.
Article6. Erickson LA, Mete O, Juhlin CC, Perren A, Gill AJ. Overview of the 2022 WHO classification of parathyroid tumors. Endocr Pathol. 2022; 33:64–89. PMID: 35175514.
Article7. Galani A, Morandi R, Dimko M, Molfino S, Baronchelli C, Lai S, et al. Atypical parathyroid adenoma: clinical and anatomical pathologic features. World J Surg Oncol. 2021; 19:19. PMID: 33472651.
Article8. DeLellis RA. Parathyroid tumors and related disorders. Mod Pathol. 2011; 24 Suppl 2:S78–S93. PMID: 21455204.
Article9. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014; 12:1495–1499. PMID: 25046131.
Article10. Rosato L, Raffaelli M, Bellantone R, Pontecorvi A, Avenia N, Boniardi M, et al. Diagnostic, therapeutic and healthcare management protocols in parathyroid surgery: II Consensus Conference of the Italian Association of Endocrine Surgery Units (U.E.C. CLUB). J Endocrinol Invest. 2014; 37:149–165. PMID: 24497214.
Article11. Polistena A, Lucchini R, Monacelli M, Triola R, Avenia S, Barillaro I, et al. Current indications for surgical treatment of primary hyperparathyroidism in the elderly. Am Surg. 2017; 83:296–302. PMID: 28316315.
Article12. Polistena A, Sanguinetti A, Lucchini R, Galasse S, Avenia S, Monacelli M, et al. Surgical treatment of secondary hyperparathyroidism in elderly patients: an institutional experience. Aging Clin Exp Res. 2017; 29(Suppl 1):23–28. PMID: 27830521.
Article13. Wilhelm SM, Wang TS, Ruan DT, Lee JA, Asa SL, Duh QY, et al. The American Association of Endocrine Surgeons guidelines for definitive management of primary hyperparathyroidism. JAMA Surg. 2016; 151:959–968. PMID: 27532368.
Article14. Cetani F, Marcocci C, Torregrossa L, Pardi E. Atypical parathyroid adenomas: challenging lesions in the differential diagnosis of endocrine tumors. Endocr Relat Cancer. 2019; 26:R441–R464. PMID: 31085770.
Article15. Martínez-Rodríguez I, Martínez-Amador N, de Arcocha-Torres M, Quirce R, Ortega-Nava F, Ibáñez-Bravo S, et al. Comparison of 99mTc-sestamibi and 11C-methionine PET/CT in the localization of parathyroid adenomas in primary hyperparathyroidism. Rev Esp Med Nucl Imagen Mol. 2014; 33:93–98. PMID: 24125595.
Article16. Kong SH, Kim JH, Kim SW, Shin CS. Radioactive parathyroid adenomas on sestamibi scans: low parathyroid hormone secretory potential and large volume. Endocrinol Metab (Seoul). 2021; 36:351–358. PMID: 33820395.
Article17. Weber T, Dotzenrath C, Dralle H, Niederle B, Riss P, Holzer K, et al. Management of primary and renal hyperparathyroidism: guidelines from the German Association of Endocrine Surgeons (CAEK). Langenbecks Arch Surg. 2021; 406:571–585. PMID: 33880642.
Article18. Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK, et al. The eighth edition AJCC cancer staging manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin. 2017; 67:93–99. PMID: 28094848.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Parathyroid Adenoma without Hyperparathyroidism Presenting as a Large Neck Mass
- Supernumerary Ectopic Mediastinal Parathyroid Adenoma Combined With Parathyroid Hyperplasia
- Giant Parathyroid Adenomas: Differential Aspects Compared to Atypical Parathyroid Adenomas
- Aging and Hormone: Estrogen, Parathyroid hormone and Bone Metabolism
- The effects of long-term lithium treatment on the parathyroid hormone and calcium level