Korean Circ J.
2023 Jul;53(7):452-471. 10.4070/kcj.2023.0115.
Korean Society of Heart Failure Guidelines for the Management of Heart Failure: Advanced and Acute Heart Failure
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Cardiovascular Medicine, Chonnam National University Medical School, Gwangju, Korea
- 3Division of Cardiology, Department of Internal Medicine, Seoul St. Mary's Hospital, Catholic Research Institute for Intractable Cardiovascular Disease, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 4Division of Cardiology, Department of Medicine, Heart Vascular Stroke Institute, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 5Division of Cardiology, Department of Internal Medicine, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea
- 6Department of Cardiology, Nowon Eulji Medical Center, Eulji University, Seoul, Korea
- 7Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea
- 8Division of Cardiology, Department of Internal Medicine, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea
- 9Division of Cardiology, Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea
- 10Division of Cardiology, Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2545131
- DOI: http://doi.org/10.4070/kcj.2023.0115
Abstract
- The Korean Society of Heart Failure (KSHF) Guidelines provide evidence-based recommendations based on Korean and international data to guide adequate diagnosis and management of heart failure (HF). Since introduction of 2017 edition of the guidelines, management of advanced HF has considerably improved, especially with advances in mechanical circulatory support and devices. The current guidelines addressed these improvements. In addition, we have included recently updated evidence-based recommendations regarding acute HF in these guidelines. In summary, Part IV of the KSHF Guidelines covers the appropriate diagnosis and optimized management of advanced and acute HF.
Figure
Cited by 1 articles
-
Frailty, Sarcopenia, Cachexia, and Malnutrition in Heart Failure
Daichi Maeda, Yudai Fujimoto, Taisuke Nakade, Takuro Abe, Shiro Ishihara, Kentaro Jujo, Yuya Matsue
Korean Circ J. 2024;54(7):363-381. doi: 10.4070/kcj.2024.0089.
Reference
-
1. Park JJ, Lee CJ, Park SJ, et al. Heart failure statistics in Korea, 2020: a report from the Korean Society of Heart Failure. Int J Heart Fail. 2021; 3:224–236. PMID: 36262554.
Article2. Groenewegen A, Rutten FH, Mosterd A, Hoes AW. Epidemiology of heart failure. Eur J Heart Fail. 2020; 22:1342–1356. PMID: 32483830.
Article3. Kim MS, Lee JH, Kim EJ, et al. Korean guidelines for diagnosis and management of chronic heart failure. Korean Circ J. 2017; 47:555–643. PMID: 28955381.
Article4. Kim MS, Lee JH, Cho HJ, et al. KSHF guidelines for the management of acute heart failure: Part III. Specific management of acute heart failure according to the etiology and co-morbidity. Korean Circ J. 2019; 49:46–68. PMID: 30637995.
Article5. Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022; 145:e895–1032. PMID: 35363499.6. McDonagh TA, Metra M, Adamo M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021; 42:3599–3726. PMID: 34447992.
Article7. Crespo-Leiro MG, Metra M, Lund LH, et al. Advanced heart failure: a position statement of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2018; 20:1505–1535. PMID: 29806100.
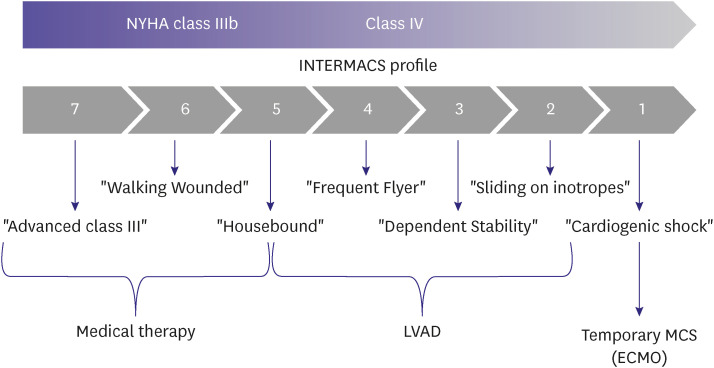
Article8. Stevenson LW, Pagani FD, Young JB, et al. INTERMACS profiles of advanced heart failure: the current picture. J Heart Lung Transplant. 2009; 28:535–541. PMID: 19481012.
Article9. Baran DA, Grines CL, Bailey S, et al. SCAI clinical expert consensus statement on the classification of cardiogenic shock: This document was endorsed by the American College of Cardiology (ACC), the American Heart Association (AHA), the Society of Critical Care Medicine (SCCM), and the Society of Thoracic Surgeons (STS) in April 2019. Catheter Cardiovasc Interv. 2019; 94:29–37. PMID: 31104355.
Article10. Jentzer JC, van Diepen S, Barsness GW, et al. Cardiogenic shock classification to predict mortality in the cardiac intensive care unit. J Am Coll Cardiol. 2019; 74:2117–2128. PMID: 31548097.
Article11. Keebler ME, Haddad EV, Choi CW, et al. Venoarterial extracorporeal membrane oxygenation in cardiogenic shock. JACC Heart Fail. 2018; 6:503–516. PMID: 29655828.
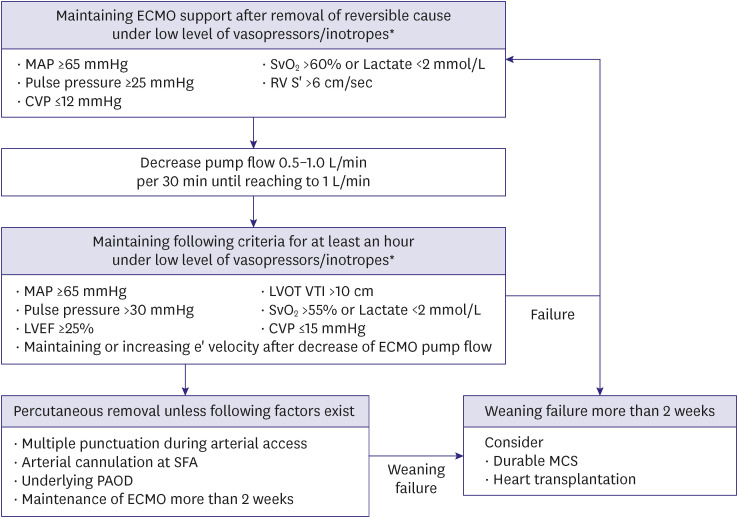
Article12. Kim D, Jang WJ, Park TK, et al. Echocardiographic predictors of successful extracorporeal membrane oxygenation weaning after refractory cardiogenic shock. J Am Soc Echocardiogr. 2021; 34:414–422.e4. PMID: 33321165.
Article13. Kim D, Park Y, Choi KH, et al. Prognostic implication of RV coupling to pulmonary circulation for successful weaning from extracorporeal membrane oxygenation. JACC Cardiovasc Imaging. 2021; 14:1523–1531. PMID: 33865793.
Article14. Mehra MR, Goldstein DJ, Uriel N, et al. Two-year outcomes with a magnetically levitated cardiac pump in heart failure. N Engl J Med. 2018; 378:1386–1395. PMID: 29526139.
Article15. Park Y, Kim D, Yang JH, Cho YH, Choi JO, Jeon ES. Clinical outcome in patients with end-stage heart failure who underwent continuous-flow left ventricular assist devices in a single center. Korean J Intern Med. 2022; 37:340–349. PMID: 34871480.
Article16. Mehra MR, Canter CE, Hannan MM, et al. The 2016 International Society for Heart Lung Transplantation listing criteria for heart transplantation: a 10-year update. J Heart Lung Transplant. 2016; 35:1–23. PMID: 26776864.
Article17. Kim IC, Youn JC, Kobashigawa JA. The past, present and future of heart transplantation. Korean Circ J. 2018; 48:565–590. PMID: 29968430.
Article19. Kim D, Choi JO, Oh J, et al. The Korean Organ Transplant Registry (KOTRY): second official adult heart transplant report. Korean Circ J. 2019; 49:724–737. PMID: 31074219.
Article20. Khush KK, Cherikh WS, Chambers DC, et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: thirty-sixth adult heart transplantation report - 2019; focus theme: donor and recipient size match. J Heart Lung Transplant. 2019; 38:1056–1066. PMID: 31548031.
Article21. Kim KJ, Cho HJ, Kim MS, et al. Focused update of 2016 Korean Society of Heart Failure guidelines for the management of chronic heart failure. Int J Heart Fail. 2019; 1:4–24. PMID: 36262736.
Article22. Sahlollbey N, Lee CK, Shirin A, Joseph P. The impact of palliative care on clinical and patient-centred outcomes in patients with advanced heart failure: a systematic review of randomized controlled trials. Eur J Heart Fail. 2020; 22:2340–2346. PMID: 32176831.
Article23. Hill L, Prager Geller T, Baruah R, et al. Integration of a palliative approach into heart failure care: a European Society of Cardiology Heart Failure Association position paper. Eur J Heart Fail. 2020; 22:2327–2339. PMID: 32892431.
Article24. Johnson MJ, McDonagh TA, Harkness A, McKay SE, Dargie HJ. Morphine for the relief of breathlessness in patients with chronic heart failure--a pilot study. Eur J Heart Fail. 2002; 4:753–756. PMID: 12453546.
Article25. Oxberry SG, Bland JM, Clark AL, Cleland JG, Johnson MJ. Repeat dose opioids may be effective for breathlessness in chronic heart failure if given for long enough. J Palliat Med. 2013; 16:250–255. PMID: 23368980.
Article26. Lee SE, Lee HY, Cho HJ, et al. Clinical characteristics and outcome of acute heart failure in Korea: results from the Korean Acute Heart Failure Registry (KorAHF). Korean Circ J. 2017; 47:341–353. PMID: 28567084.
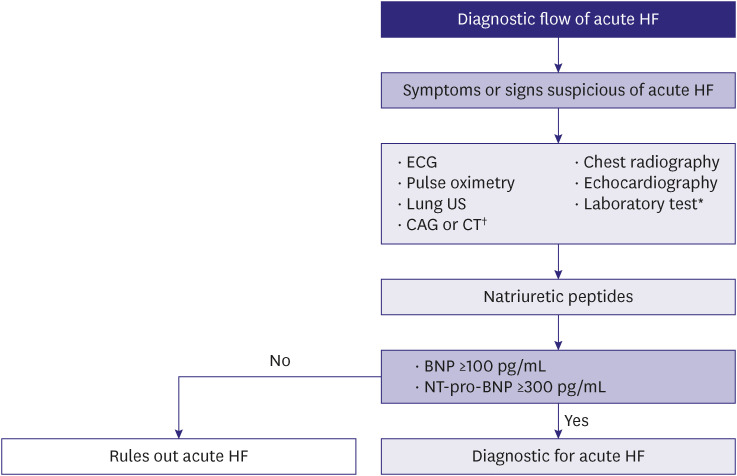
Article27. Januzzi JL Jr, Chen-Tournoux AA, Christenson RH, et al. N-terminal pro-B-type natriuretic peptide in the emergency department: the ICON-RELOADED study. J Am Coll Cardiol. 2018; 71:1191–1200. PMID: 29544601.28. Mueller C, McDonald K, de Boer RA, et al. Heart Failure Association of the European Society of Cardiology practical guidance on the use of natriuretic peptide concentrations. Eur J Heart Fail. 2019; 21:715–731. PMID: 31222929.
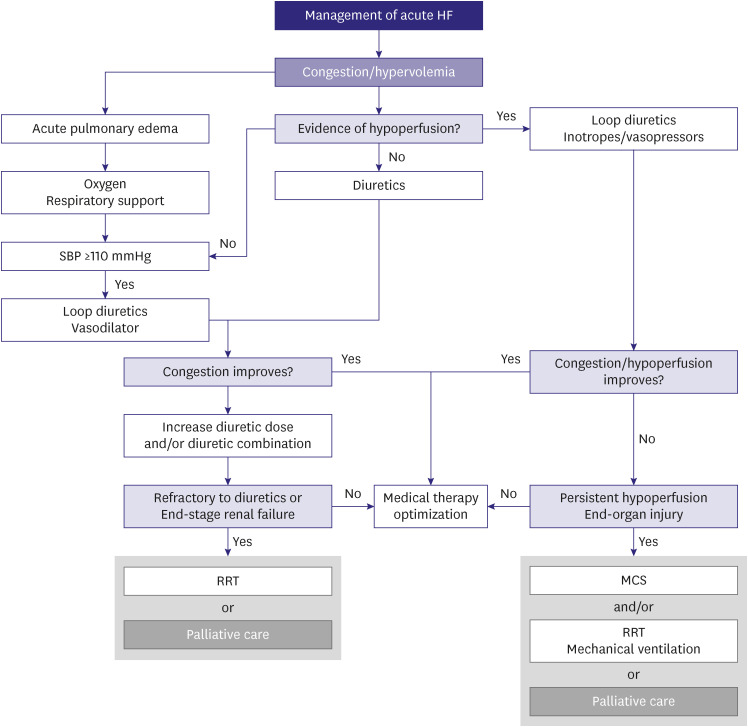
Article29. Takagi K, Kimmoun A, Sato N, Mebazaa A. Management of acute heart failure during an early phase. Int J Heart Fail. 2020; 2:91–110. PMID: 36263292.
Article30. Nikolaou M, Parissis J, Yilmaz MB, et al. Liver function abnormalities, clinical profile, and outcome in acute decompensated heart failure. Eur Heart J. 2013; 34:742–749. PMID: 23091203.
Article31. Wettersten N. Biomarkers in acute heart failure: diagnosis, prognosis, and treatment. Int J Heart Fail. 2021; 3:81–105. PMID: 36262882.
Article32. Drazner MH, Hellkamp AS, Leier CV, et al. Value of clinician assessment of hemodynamics in advanced heart failure: the ESCAPE trial. Circ Heart Fail. 2008; 1:170–177. PMID: 19675681.
Article33. Stevenson LW, Perloff JK. The limited reliability of physical signs for estimating hemodynamics in chronic heart failure. JAMA. 1989; 261:884–888. PMID: 2913385.
Article34. Chakko S, Woska D, Martinez H, et al. Clinical, radiographic, and hemodynamic correlations in chronic congestive heart failure: conflicting results may lead to inappropriate care. Am J Med. 1991; 90:353–359. PMID: 1825901.
Article35. Butman SM, Ewy GA, Standen JR, Kern KB, Hahn E. Bedside cardiovascular examination in patients with severe chronic heart failure: importance of rest or inducible jugular venous distension. J Am Coll Cardiol. 1993; 22:968–974. PMID: 8409071.
Article36. Binanay C, Califf RM, Hasselblad V, et al. Evaluation study of congestive heart failure and pulmonary artery catheterization effectiveness: the ESCAPE trial. JAMA. 2005; 294:1625–1633. PMID: 16204662.
Article37. Shah MR, Hasselblad V, Stevenson LW, et al. Impact of the pulmonary artery catheter in critically ill patients: meta-analysis of randomized clinical trials. JAMA. 2005; 294:1664–1670. PMID: 16204666.
Article38. Costanzo MR, Stevenson LW, Adamson PB, et al. Interventions linked to decreased heart failure hospitalizations during ambulatory pulmonary artery pressure monitoring. JACC Heart Fail. 2016; 4:333–344. PMID: 26874388.
Article39. Abraham WT, Adamson PB, Bourge RC, et al. Wireless pulmonary artery haemodynamic monitoring in chronic heart failure: a randomised controlled trial. Lancet. 2011; 377:658–666. PMID: 21315441.
Article40. Lindenfeld J, Zile MR, Desai AS, et al. Haemodynamic-guided management of heart failure (GUIDE-HF): a randomised controlled trial. Lancet. 2021; 398:991–1001. PMID: 34461042.
Article41. Rohde LE, Rover MM, Figueiredo Neto JA, et al. Short-term diuretic withdrawal in stable outpatients with mild heart failure and no fluid retention receiving optimal therapy: a double-blind, multicentre, randomized trial. Eur Heart J. 2019; 40:3605–3612. PMID: 31424503.
Article42. Mebazaa A, Yilmaz MB, Levy P, et al. Recommendations on pre-hospital & early hospital management of acute heart failure: a consensus paper from the Heart Failure Association of the European Society of Cardiology, the European Society of Emergency Medicine and the Society of Academic Emergency Medicine. Eur J Heart Fail. 2015; 17:544–558. PMID: 25999021.
Article43. Damman K, Ter Maaten JM, Coster JE, et al. Clinical importance of urinary sodium excretion in acute heart failure. Eur J Heart Fail. 2020; 22:1438–1447. PMID: 32086996.
Article44. Mullens W, Verbrugge FH, Nijst P, et al. Rationale and design of the ADVOR (Acetazolamide in Decompensated Heart Failure with Volume Overload) trial. Eur J Heart Fail. 2018; 20:1591–1600. PMID: 30238574.
Article45. Cox ZL, Hung R, Lenihan DJ, Testani JM. Diuretic strategies for loop diuretic resistance in acute heart failure: the 3T trial. JACC Heart Fail. 2020; 8:157–168. PMID: 31838029.46. Mullens W, Dauw J, Martens P, et al. Acetazolamide in acute decompensated heart failure with volume overload. N Engl J Med. 2022; 387:1185–1195. PMID: 36027559.
Article47. Vardeny O, Claggett B, Kachadourian J, et al. Reduced loop diuretic use in patients taking sacubitril/valsartan compared with enalapril: the PARADIGM-HF trial. Eur J Heart Fail. 2019; 21:337–341. PMID: 30741494.
Article48. Mullens W, Damman K, Harjola VP, et al. The use of diuretics in heart failure with congestion - a position statement from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2019; 21:137–155. PMID: 30600580.49. Cotter G, Metzkor E, Kaluski E, et al. Randomised trial of high-dose isosorbide dinitrate plus low-dose furosemide versus high-dose furosemide plus low-dose isosorbide dinitrate in severe pulmonary oedema. Lancet. 1998; 351:389–393. PMID: 9482291.
Article50. Levy P, Compton S, Welch R, et al. Treatment of severe decompensated heart failure with high-dose intravenous nitroglycerin: a feasibility and outcome analysis. Ann Emerg Med. 2007; 50:144–152. PMID: 17509731.
Article51. Peacock WF, Hollander JE, Diercks DB, Lopatin M, Fonarow G, Emerman CL. Morphine and outcomes in acute decompensated heart failure: an ADHERE analysis. Emerg Med J. 2008; 25:205–209. PMID: 18356349.
Article52. Gil V, Domínguez-Rodríguez A, Masip J, Peacock WF, Miró Ò. Morphine use in the treatment of acute cardiogenic pulmonary edema and its effects on patient outcome: a systematic review. Curr Heart Fail Rep. 2019; 16:81–88. PMID: 31183779.
Article53. van Diepen S, Katz JN, Albert NM, et al. Contemporary management of cardiogenic shock: a scientific statement from the American Heart Association. Circulation. 2017; 136:e232–e268. PMID: 28923988.
Article54. Kang J, Cho HJ, Lee HY, et al. Effects of widespread inotrope use in acute heart failure patients. J Clin Med. 2018; 7:368. PMID: 30340408.
Article55. Chioncel O, Parissis J, Mebazaa A, et al. Epidemiology, pathophysiology and contemporary management of cardiogenic shock - a position statement from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2020; 22:1315–1341. PMID: 32469155.
Article56. Maack C, Eschenhagen T, Hamdani N, et al. Treatments targeting inotropy. Eur Heart J. 2019; 40:3626–3644. PMID: 30295807.
Article57. Ahmad T, Miller PE, McCullough M, et al. Why has positive inotropy failed in chronic heart failure? Lessons from prior inotrope trials. Eur J Heart Fail. 2019; 21:1064–1078. PMID: 31407860.
Article58. De Backer D, Biston P, Devriendt J, et al. Comparison of dopamine and norepinephrine in the treatment of shock. N Engl J Med. 2010; 362:779–789. PMID: 20200382.
Article59. Levy B, Clere-Jehl R, Legras A, et al. Epinephrine versus norepinephrine for cardiogenic shock after acute myocardial infarction. J Am Coll Cardiol. 2018; 72:173–182. PMID: 29976291.
Article60. Greene SJ, Fonarow GC, Vaduganathan M, Khan SS, Butler J, Gheorghiade M. The vulnerable phase after hospitalization for heart failure. Nat Rev Cardiol. 2015; 12:220–229. PMID: 25666406.
Article61. Chioncel O, Mebazaa A, Maggioni AP, et al. Acute heart failure congestion and perfusion status - impact of the clinical classification on in-hospital and long-term outcomes; insights from the ESC-EORP-HFA Heart Failure Long-Term Registry. Eur J Heart Fail. 2019; 21:1338–1352. PMID: 31127678.
Article62. Naylor M, Brooten D, Jones R, Lavizzo-Mourey R, Mezey M, Pauly M. Comprehensive discharge planning for the hospitalized elderly. A randomized clinical trial. Ann Intern Med. 1994; 120:999–1006. PMID: 8185149.
Article63. Gayat E, Arrigo M, Littnerova S, et al. Heart failure oral therapies at discharge are associated with better outcome in acute heart failure: a propensity-score matched study. Eur J Heart Fail. 2018; 20:345–354. PMID: 28849606.
Article64. Prins KW, Neill JM, Tyler JO, Eckman PM, Duval S. Effects of beta-blocker withdrawal in acute decompensated heart failure: a systematic review and meta-analysis. JACC Heart Fail. 2015; 3:647–653. PMID: 26251094.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute Heart Failure and Its Management
- Key Role of the Korean Society of Heart Failure: Moving Towards a Global and Individualized Approach
- The Korean Society of Heart Failure: Breaking Barriers, Bridging Solutions Together!
- Role of cardiac imaging in management of heart failure
- Korean Society of Heart Failure Guidelines for the Management of Heart Failure: Advanced and Acute Heart Failure