J Korean Med Sci.
2023 Aug;38(31):e238. 10.3346/jkms.2023.38.e238.
Substantial Lipid Increases During Menopausal Transition in Korean Middle-Aged Women
- Affiliations
-
- 1Division of Population Health Research, Department of Precision Medicine, Korea National Institute of Health, Korea Disease Control and Prevention Agency (KDCA), Cheongju, Korea
- 2Korea National Institute of Health, Korea Disease Control and Prevention Agency (KDCA), Cheongju, Korea
- KMID: 2544957
- DOI: http://doi.org/10.3346/jkms.2023.38.e238
Abstract
- Background
Adverse lipid profiles are observed in postmenopausal women. However, there is insufficient evidence of the association between lipids and reproductive aging in Korean women. We aimed to characterize lipid changes with respect to timing relative to menopause in Korean middle-aged women.
Methods
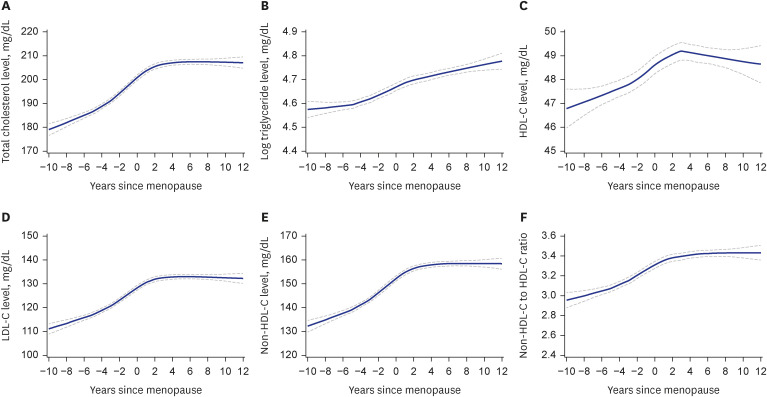
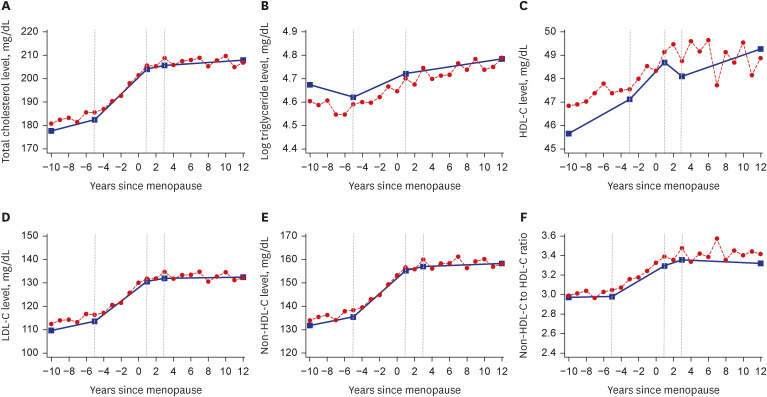
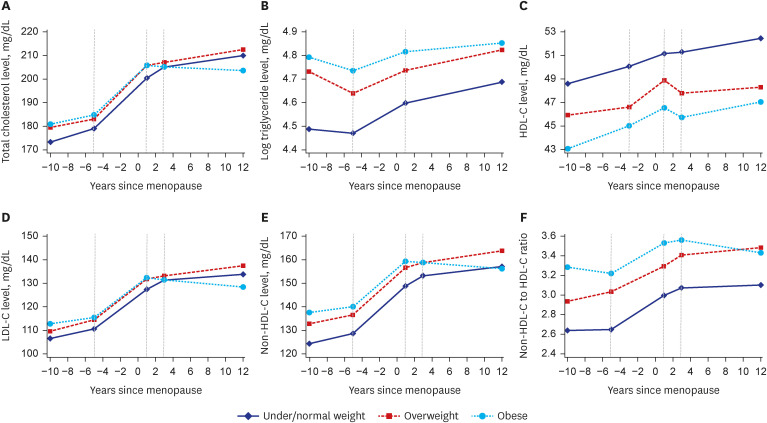
This study included 1,436 premenopausal women who had a natural menopause during the follow-up period (median = 15.76 years) from the Korean Genome and Epidemiology Study (KoGES) Ansan and Anseong cohort. Lipid levels were measured every 2 years, and the magnitudes of annual lipid changes and differences in the changes by premenopausal body mass index were estimated using piecewise linear mixed-effects models.
Results
All lipid levels increased greatly from 3 or 5 years before menopause to 1 year after menopause in all women, regardless of their premenopausal body mass index. During the period, high-density lipoprotein cholesterol (HDL-C) levels increased at 0.42 mg/dL per year (95% confidence interval [CI], 0.29 to 0.55 mg/dL). Nevertheless, non-HDL-C levels simultaneously increased at 3.42 mg/dL per year (95% CI, 3.11 to 3.72 mg/dL), and an annual change in the non-HDL-C to HDL-C ratio was 0.05 (95% CI, 0.04 to 0.06). One year after menopause, changes in all lipid parameters significantly slowed down, except for the nonHDL-C to HDL-C ratio (P < 0.001 for all). The ratio continued to increase until 3 years after menopause, but thereafter, the change leveled off.
Conclusion
Women experienced remarkable increases in lipid levels during menopausal transition, highlighting the need for early intervention strategies for cardiovascular disease prevention in women.
Keyword
Figure
Reference
-
1. Vogel B, Acevedo M, Appelman Y, Bairey Merz CN, Chieffo A, Figtree GA, et al. The Lancet women and cardiovascular disease Commission: reducing the global burden by 2030. Lancet. 2021; 397(10292):2385–2438. PMID: 34010613.2. O’Kelly AC, Michos ED, Shufelt CL, Vermunt JV, Minissian MB, Quesada O, et al. Pregnancy and reproductive risk factors for cardiovascular disease in women. Circ Res. 2022; 130(4):652–672. PMID: 35175837.3. Harlow SD, Gass M, Hall JE, Lobo R, Maki P, Rebar RW, et al. Executive summary of the Stages of Reproductive Aging Workshop + 10: addressing the unfinished agenda of staging reproductive aging. J Clin Endocrinol Metab. 2012; 97(4):1159–1168. PMID: 22344196.4. El Khoudary SR, Aggarwal B, Beckie TM, Hodis HN, Johnson AE, Langer RD, et al. Menopause transition and cardiovascular disease risk: implications for timing of early prevention: a scientific statement from the American Heart Association. Circulation. 2020; 142(25):e506–e532. PMID: 33251828.5. Cho SMJ, Lee H, Lee HH, Baek J, Heo JE, Joo HJ, et al. Dyslipidemia fact sheets in Korea 2020: an analysis of nationwide population-based data. J Lipid Atheroscler. 2021; 10(2):202–209. PMID: 34095012.6. An S, Ahn C, Jang J, Lee J, Kang D, Lee JK, et al. Comparison of the prevalence of cardiometabolic disorders and comorbidities in Korea and the United States: analysis of the National Health and Nutrition Examination Survey. J Korean Med Sci. 2022; 37(18):e149. PMID: 35535376.7. Park CY, Lim JY, Park HY. Age at natural menopause in Koreans: secular trends and influences thereon. Menopause. 2018; 25(4):423–429. PMID: 29112598.8. Matthews KA, Chen X, Barinas-Mitchell E, Brooks MM, Derby CA, Harlow S, et al. Age at menopause in relationship to lipid changes and subclinical carotid disease across 20 years: Study of Women’s Health Across the Nation. J Am Heart Assoc. 2021; 10(18):e021362. PMID: 34482713.9. Matthews KA, Crawford SL, Chae CU, Everson-Rose SA, Sowers MF, Sternfeld B, et al. Are changes in cardiovascular disease risk factors in midlife women due to chronological aging or to the menopausal transition? J Am Coll Cardiol. 2009; 54(25):2366–2373. PMID: 20082925.10. Matthews KA, El Khoudary SR, Brooks MM, Derby CA, Harlow SD, Barinas-Mitchell EJ, et al. Lipid changes around the final menstrual period predict carotid subclinical disease in postmenopausal women. Stroke. 2017; 48(1):70–76. PMID: 27909203.11. Ambikairajah A, Walsh E, Cherbuin N. Lipid profile differences during menopause: a review with meta-analysis. Menopause. 2019; 26(11):1327–1333. PMID: 31567869.12. Choi Y, Chang Y, Kim BK, Kang D, Kwon MJ, Kim CW, et al. Menopausal stages and serum lipid and lipoprotein abnormalities in middle-aged women. Maturitas. 2015; 80(4):399–405. PMID: 25631350.13. El Khoudary SR, Chen X, Nasr AN, Billheimer J, Brooks MM, McConnell D, et al. HDL (high-density lipoprotein) subclasses, lipid content, and function trajectories across the menopause transition: SWAN-HDL study. Arterioscler Thromb Vasc Biol. 2021; 41(2):951–961. PMID: 33267661.14. Iannuzzi A, Giallauria F, Gentile M, Rubba P, Covetti G, Bresciani A, et al. Association between non-HDL-C/HDL-C ratio and carotid intima-media thickness in post-menopausal women. J Clin Med. 2021; 11(1):78. PMID: 35011818.15. Masson W, Epstein T, Huerín M, Lobo M, Molinero G, Siniawski D. Association between non-HDL-C/HDL-C ratio and carotid atherosclerosis in postmenopausal middle-aged women. Climacteric. 2019; 22(5):518–522. PMID: 31287342.16. Kim Y, Han BG. KoGES Group. Cohort profile: the Korean Genome and Epidemiology Study (KoGES) Consortium. Int J Epidemiol. 2017; 46(4):1350. PMID: 28938752.17. Wu SI, Chou P, Tsai ST. The impact of years since menopause on the development of impaired glucose tolerance. J Clin Epidemiol. 2001; 54(2):117–120. PMID: 11166525.18. World Health Organization; International Association for the Study of Obesity. International Obesity Taskforce. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment. Sydney, Australia: Health Communications Australia;2000. p. 15–21.19. Duncan MS, Vasan RS, Xanthakis V. Trajectories of blood lipid concentrations over the adult life course and risk of cardiovascular disease and all-cause mortality: observations from the Framingham Study over 35 years. J Am Heart Assoc. 2019; 8(11):e011433. PMID: 31137992.20. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972; 18(6):499–502. PMID: 4337382.21. Derby CA, Crawford SL, Pasternak RC, Sowers M, Sternfeld B, Matthews KA. Lipid changes during the menopause transition in relation to age and weight: the Study of Women’s Health Across the Nation. Am J Epidemiol. 2009; 169(11):1352–1361. PMID: 19357323.22. Seong SC, Kim YY, Park SK, Khang YH, Kim HC, Park JH, et al. Cohort profile: the National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) in Korea. BMJ Open. 2017; 7(9):e016640.23. Shin DW, Cho J, Park JH, Cho B. National general health screening program in Korea: history, current status, and future direction: a scoping review. Precis Future Med. 2022; 6(1):9–31.24. Park BH, Lee BK, Ahn J, Kim NS, Park J, Kim Y. Association of participation in health check-ups with risk factors for cardiovascular diseases. J Korean Med Sci. 2021; 36(3):e19. PMID: 33463093.25. Freeman EW, Sammel MD, Lin H, Gracia CR. Obesity and reproductive hormone levels in the transition to menopause. Menopause. 2010; 17(4):718–726. PMID: 20216473.26. Tepper PG, Randolph JF Jr, McConnell DS, Crawford SL, El Khoudary SR, Joffe H, et al. Trajectory clustering of estradiol and follicle-stimulating hormone during the menopausal transition among women in the Study of Women’s Health across the Nation (SWAN). J Clin Endocrinol Metab. 2012; 97(8):2872–2880. PMID: 22659249.27. Anderson KM, Castelli WP, Levy D. Cholesterol and mortality. 30 years of follow-up from the Framingham Study. JAMA. 1987; 257(16):2176–2180. PMID: 3560398.28. Orkaby AR. The highs and lows of cholesterol: a paradox of healthy aging? J Am Geriatr Soc. 2020; 68(2):236–237. PMID: 31930729.29. Li H, Sun R, Chen Q, Guo Q, Wang J, Lu L, et al. Association between HDL-C levels and menopause: a meta-analysis. Hormones (Athens). 2021; 20(1):49–59. PMID: 32557344.30. Ding M, Manson JE. HDL-c and arterial calcification in midlife women: does an HDL paradox exist? Menopause. 2021; 28(3):231–233. PMID: 33399324.31. Fan AZ, Dwyer JH. Sex differences in the relation of HDL cholesterol to progression of carotid intima-media thickness: the Los Angeles Atherosclerosis Study. Atherosclerosis. 2007; 195(1):e191–e196. PMID: 17482196.32. Borén J, Taskinen MR, Björnson E, Packard CJ. Metabolism of triglyceride-rich lipoproteins in health and dyslipidaemia. Nat Rev Cardiol. 2022; 19(9):577–592. PMID: 35318466.33. Clayton GL, Soares AG, Kilpi F, Fraser A, Welsh P, Sattar N, et al. Cardiovascular health in the menopause transition: a longitudinal study of up to 3892 women with up to four repeated measures of risk factors. BMC Med. 2022; 20(1):299. PMID: 35974322.34. Park JH, Lee MH, Shim JS, Choi DP, Song BM, Lee SW, et al. Effects of age, sex, and menopausal status on blood cholesterol profile in the Korean population. Korean Circ J. 2015; 45(2):141–148. PMID: 25810736.35. Frank AT, Zhao B, Jose PO, Azar KM, Fortmann SP, Palaniappan LP. Racial/ethnic differences in dyslipidemia patterns. Circulation. 2014; 129(5):570–579. PMID: 24192801.36. Paramsothy P, Harlow SD, Nan B, Greendale GA, Santoro N, Crawford SL, et al. Duration of the menopausal transition is longer in women with young age at onset: the multiethnic Study of Women’s Health Across the Nation. Menopause. 2017; 24(2):142–149. PMID: 27676632.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Structural Equation Modeling on Healthy Menopausal Transition
- Effects of Koryo Hand Therapy on Menopausal Symptoms and Blood Lipid Levels in Middle-aged Women
- Middle-aged women’s experiences of physical activity for managing menopausal symptoms: a phenomenological study
- Menopause Knowledge, Attitude, Symptom and Management among Midlife Employed Women
- A menopausal transition model based on transition theory