J Korean Med Sci.
2023 Jul;38(30):e235. 10.3346/jkms.2023.38.e235.
Complication Analysis in Korean Patients With Hemophilia A From 2007 to 2019: A Nationwide Study by the Health Insurance Review and Assessment Service Database
- Affiliations
-
- 1Department of Pediatrics, Ajou University Hospital, Ajou University School of Medicine, Suwon, Korea
- 2Department of Pediatrics, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, Daegu, Korea
- 3Education Support Center, Keimyung University School of Medicine, Daegu, Korea
- 4Medical Research Collaboration Center in Kyungpook National University Hospital, Department of Medical Informatics, School of Medicine, Kyungpook National University, Daegu, Korea
- KMID: 2544953
- DOI: http://doi.org/10.3346/jkms.2023.38.e235
Abstract
- Background
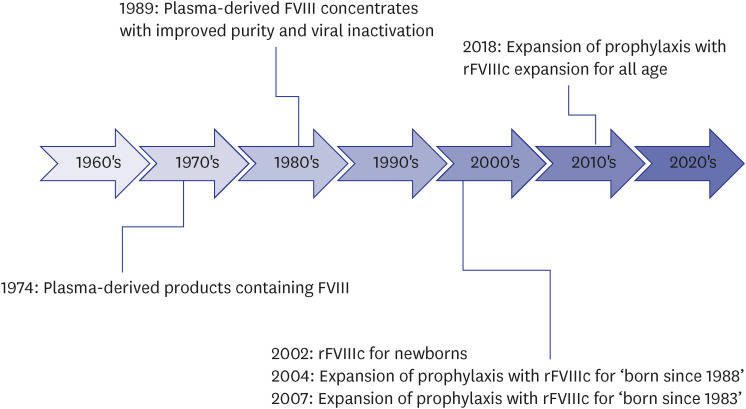
There has been remarkable progress in hemophilia A (HA) treatment in Korea. Viral inactivation products were developed in 1989, use of recombinant factor VIII (FVIII) concentrates started in 2002, and prophylaxis expanded thereafter. This study was conducted to identify the changes in complications in HA before and after 1989 or 2002.
Methods
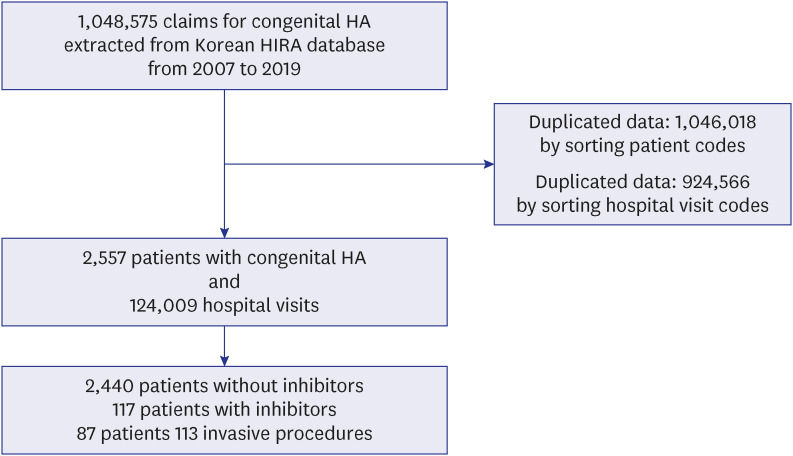
The study was performed using the 2007–2019 Healthcare Big Data Hub of the Health Insurance Review and Assessment Service.
Results
Among 2,557 patients, 1,084 had ≥ 1 complication; 829 had joint problems, 328 had viral infections, 146 had neurologic sequelae, and 87 underwent 113 surgeries or procedures due to complications. Patients born after 1989 had a significantly lower risk of viral infections than those born before 1989; 27.1% vs. 1.4% (P < 0.001, odds ratio [OR], 0.037). Patients born after 2002 had a significantly lower risk of joint problems than those born before 2002; 36.8% vs. 24.7% (P < 0.001, OR, 0.538). Patients born after 2002 had a higher incidence of neurologic sequelae than those born before 2002; 3.7% vs. 11.1% (P < 0.001, OR, 3.210). Medical expenses for complication-associated surgeries or procedures were ₩2,957,557,005.
Conclusion
Viral infections have significantly decreased in Korean patients with HA. The degree of reduction of joint problems was lower than we expected, because it took > 10 years to expand prophylaxis widely. Neurologic sequelae have not decreased; thus, additional efforts to decrease intracranial hemorrhage are needed. We suggest personalized dosing of FVIII and more meticulous care during childbirth to further reduce the complications.
Figure
Reference
-
1. Franchini M, Mannucci PM. Past, present and future of hemophilia: a narrative review. Orphanet J Rare Dis. 2012; 7(1):24. PMID: 22551339.2. Mannucci PM, Tuddenham EG. The hemophilias--from royal genes to gene therapy. N Engl J Med. 2001; 344(23):1773–1779. PMID: 11396445.3. Franchini M, Mannucci PM. Hemophilia A in the third millennium. Blood Rev. 2013; 27(4):179–184. PMID: 23815950.4. Valentino LA. Blood-induced joint disease: the pathophysiology of hemophilic arthropathy. J Thromb Haemost. 2010; 8(9):1895–1902. PMID: 20586922.5. Ljung RC. Intracranial haemorrhage in haemophilia A and B. Br J Haematol. 2008; 140(4):378–384. PMID: 18081890.6. Mannucci PM. Hemophilia: treatment options in the twenty-first century. J Thromb Haemost. 2003; 1(7):1349–1355. PMID: 12871268.7. Hay CRM, Nissen F, Pipe SW. Mortality in congenital hemophilia A - a systematic literature review. J Thromb Haemost. 2021; 19:Suppl 1. (Suppl 1):6–20. PMID: 33331043.8. Raso S, Hermans C. Recombinant factor VIII: past, present and future of treatment of hemophilia A. Drugs Today (Barc). 2018; 54(4):269–281. PMID: 29869648.9. Manco-Johnson MJ, Soucie JM, Gill JC. Joint Outcomes Committee of the Universal Data Collection, US Hemophilia Treatment Center Network. Prophylaxis usage, bleeding rates, and joint outcomes of hemophilia, 1999 to 2010: a surveillance project. Blood. 2017; 129(17):2368–2374. PMID: 28183693.10. Warren BB, Thornhill D, Stein J, Fadell M, Ingram JD, Funk S, et al. Young adult outcomes of childhood prophylaxis for severe hemophilia A: results of the Joint Outcome Continuation Study. Blood Adv. 2020; 4(11):2451–2459. PMID: 32492157.11. Kim DH, Kim SK. Progress of hemophilia A therapeutics in Korea. Clin Pediatr Hematol Oncol. 2018; 25(1):17–22.12. Yoo KY, Kim SK, Kwon SS, Park SK, Yoon HJ, Lee KS, et al. Life expectancy of Korean haemophiliacs, 1991-2012. Haemophilia. 2014; 20(4):e356–e358. PMID: 24948408.13. Kim EJ, Lee H. Current status and comprehensive care of Korean hemophiliacs. Korean J Hematol. 2000; 35(3-4):222–232.14. Yoon HJ, Lee SY, Hwang TJ, Sohn YT. A prospective study on the pharmacokinetics of monoclonal-antibody-purified factor VIII concentrate (GreenMono (R)) in previously treated subjects with hemophilia A. Korean J Hematol. 2001; 36(2):148–153.15. Callaghan MU, Negrier CG, Paz-Priel I, Chang TY, Chebon S, Lehle M, et al. Long-term outcomes with emicizumab prophylaxis for hemophilia A with/without FVIII inhibitors from the HAVEN 1-4 studies. Blood. 2021; 137(16):2231–2242. PMID: 33512413.16. Ahn JH, Jung N, Shim YJ, Kim HS. Emicizumab prophylaxis in a Korean child with severe hemophilia A and high titer inhibitor: a case report. Blood Res. 2021; 56(1):44–46. PMID: 33504687.17. Hill HA, Stein SF. Viral infections among patients with hemophilia in the state of Georgia. Am J Hematol. 1998; 59(1):36–41. PMID: 9723574.18. Gualtierotti R, Solimeno LP, Peyvandi F. Hemophilic arthropathy: current knowledge and future perspectives. J Thromb Haemost. 2021; 19(9):2112–2121. PMID: 34197690.19. van Dijk K, Fischer K, van der Bom JG, Grobbee DE, van den Berg HM. Variability in clinical phenotype of severe haemophilia: the role of the first joint bleed. Haemophilia. 2005; 11(5):438–443. PMID: 16128885.20. van Vulpen LF, Holstein K, Martinoli C. Joint disease in haemophilia: pathophysiology, pain and imaging. Haemophilia. 2018; 24(Suppl 6):44–49. PMID: 29878659.21. Posthouwer D, Plug I, van der Bom JG, Fischer K, Rosendaal FR, Mauser-Bunschoten EP. Hepatitis C and health-related quality of life among patients with hemophilia. Haematologica. 2005; 90(6):846–850. PMID: 15951299.22. Stieltjes N, Calvez T, Demiguel V, Torchet MF, Briquel ME, Fressinaud E, et al. Intracranial haemorrhages in French haemophilia patients (1991-2001): clinical presentation, management and prognosis factors for death. Haemophilia. 2005; 11(5):452–458. PMID: 16128887.23. Klinge J, Auberger K, Auerswald G, Brackmann HH, Mauz-Körholz C, Kreuz W. Prevalence and outcome of intracranial haemorrhage in haemophiliacs--a survey of the paediatric group of the German Society of Thrombosis and Haemostasis (GTH). Eur J Pediatr. 1999; 158(Suppl 3):S162–S165. PMID: 10650860.24. Ljung R, Chambost H, Stain AM, DiMichele D. Haemophilia in the first years of life. Haemophilia. 2008; 14(Suppl 3):188–195. PMID: 18510541.25. Andersson NG, Auerswald G, Barnes C, Carcao M, Dunn AL, Fijnvandraat K, et al. Intracranial haemorrhage in children and adolescents with severe haemophilia A or B - the impact of prophylactic treatment. Br J Haematol. 2017; 179(2):298–307. PMID: 28699675.26. Collins PW, Björkman S, Fischer K, Blanchette V, Oh M, Schroth P, et al. Factor VIII requirement to maintain a target plasma level in the prophylactic treatment of severe hemophilia A: influences of variance in pharmacokinetics and treatment regimens. J Thromb Haemost. 2010; 8(2):269–275. PMID: 19943875.27. Economou M, Banov L, Ljung R. Perinatal aspects of haemophilia. Eur J Haematol Suppl. 2014; 76:21–25. PMID: 24957104.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Epidemiology of Congenital Bleeding Disorders: a Nationwide Populationbased Korean Study
- The Effect of the National Health Insurance Coverage of Chuna Therapy on the Costs and Service Uses of Chuna Therapy in Automobile Insurance Oriental Medical Institutions
- Incidence and Treatment Pattern of Extremity Soft Tissue Sarcoma in Korea, 2009-2011: A Nationwide Study Based on the Health Insurance Review and Assessment Service Database
- Data Configuration and Publication Trends for the Korean National Health Insurance and Health Insurance Review & Assessment Database
- Validation of operational definitions of mortality in a nationwide hemodialysis population using the Health Insurance Review and Assessment Service databases of Korea