Korean J Gastroenterol.
2023 Jul;82(1):18-24. 10.4166/kjg.2023.029.
Validity and Reliability of the Reflux Symptoms Index Translated into Indonesian: The Role of Upper Endoscopy in Assessing Extra-Esophageal Gastroesophageal Reflux Disease Symptoms
- Affiliations
-
- 1Doctoral Program of Medical Science, Faculty of Medicine, Universitas Airlangga, Surabaya, Indonesia
- 2Division of Gastroentero-Hepatology, Department of Internal Medicine, Faculty of Medicine, Universitas Airlangga, Surabaya, Indonesia
- 3Internal Medicine Department, Faculty of Medicine, Universitas Airlangga, Surabaya, Indonesia
- 4Department of Medical Microbiology, Faculty of Medicine, Universitas Airlangga, Surabaya, Indonesia
- 5Surabaya, Indonesia; Department of Gastroenterology, Dhaka Medical College and Hospital, Dhaka, Bangladesh
- 6Helicobacter pylori and Microbiota Study Group, Institute Tropical Disease, Universitas Airlangga, Surabaya, Indonesia
- KMID: 2544935
- DOI: http://doi.org/10.4166/kjg.2023.029
Abstract
- Background/Aims
The Reflux Symptom Index (RSI) is a questionnaire that evaluates the severity of extra-esophageal symptoms and is one of the most widely used measures to evaluate LPR. This study assessed the validity and reliability of the RSI questionnaire in Bahasa Indonesia and investigated the association between each extra-esophageal symptom reported in the questionnaire and the severity of erosive esophagitis as determined by endoscopic findings.
Methods
85 adult patients with GERD symptoms had an upper endoscopy examination and were asked to complete the translated RSI. The validity and reliability of the questionnaire were assessed.
Results
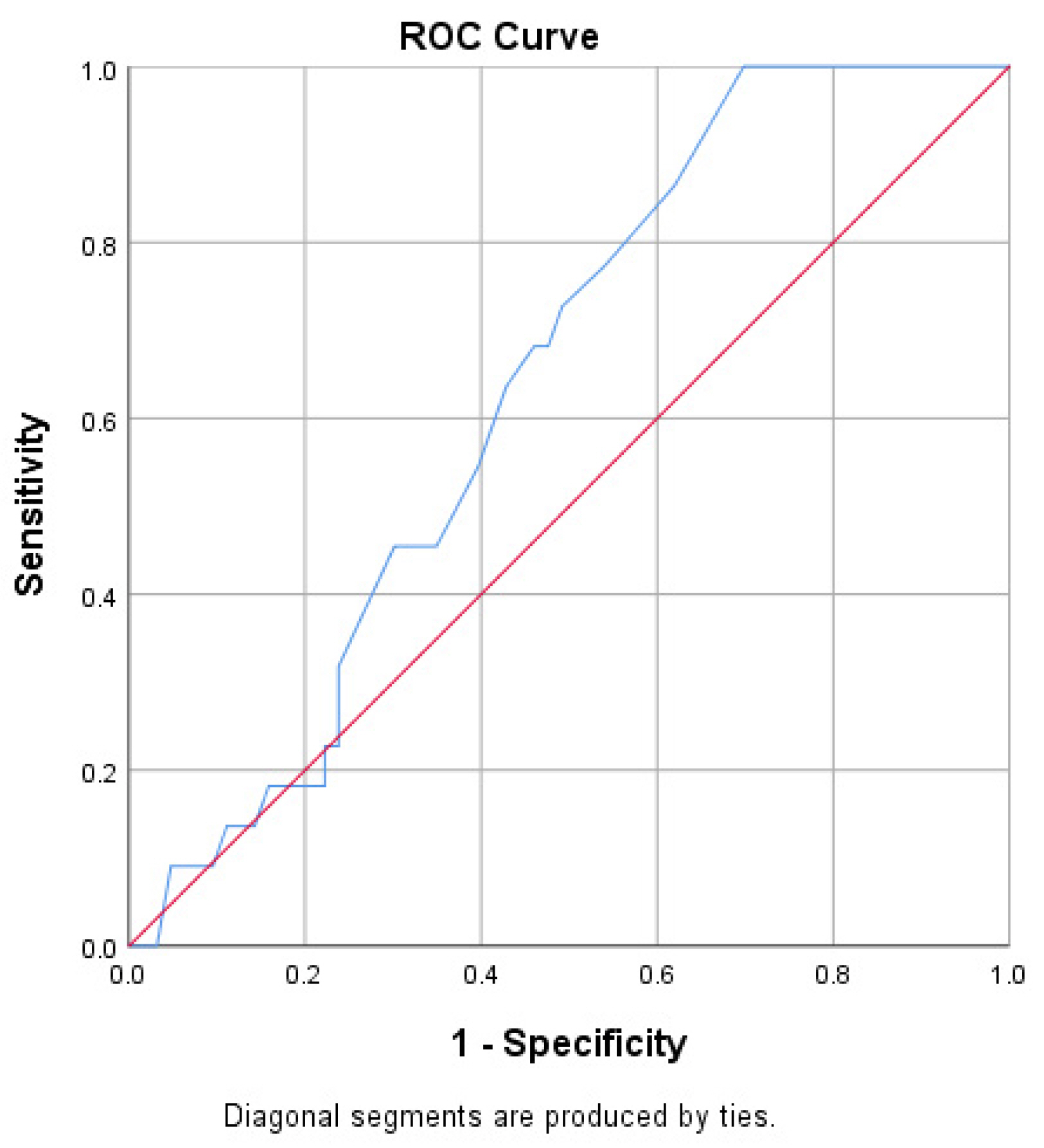
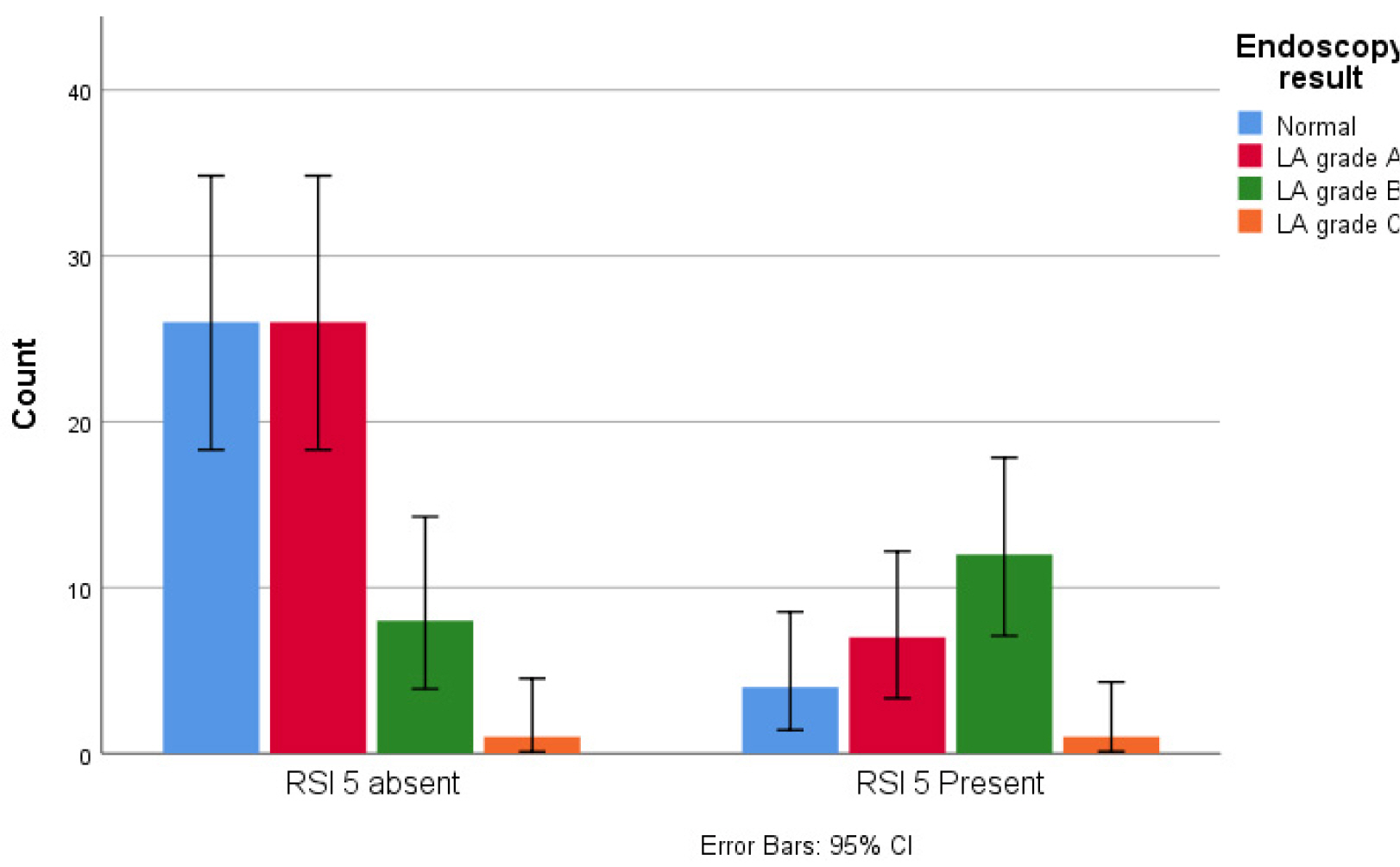
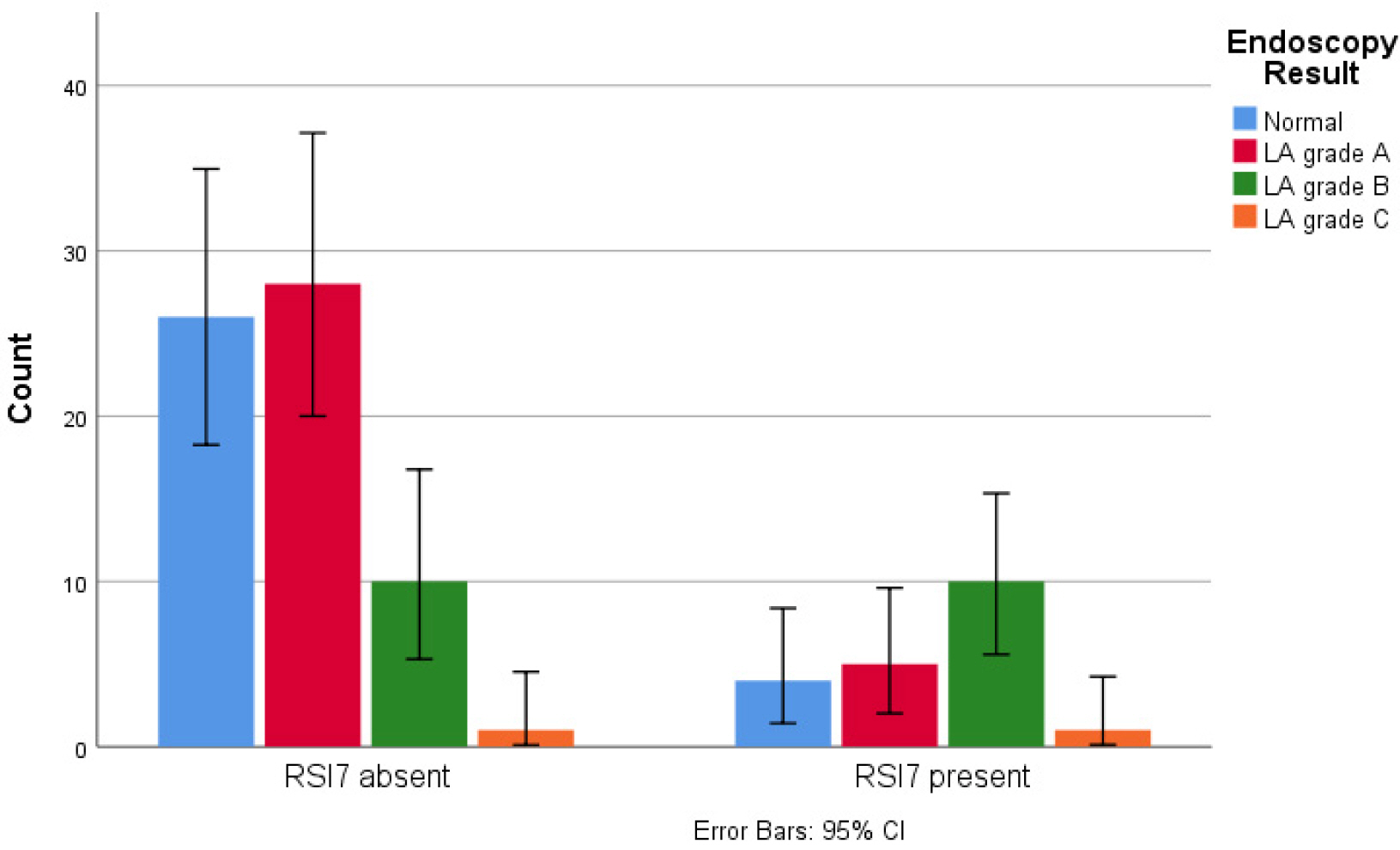
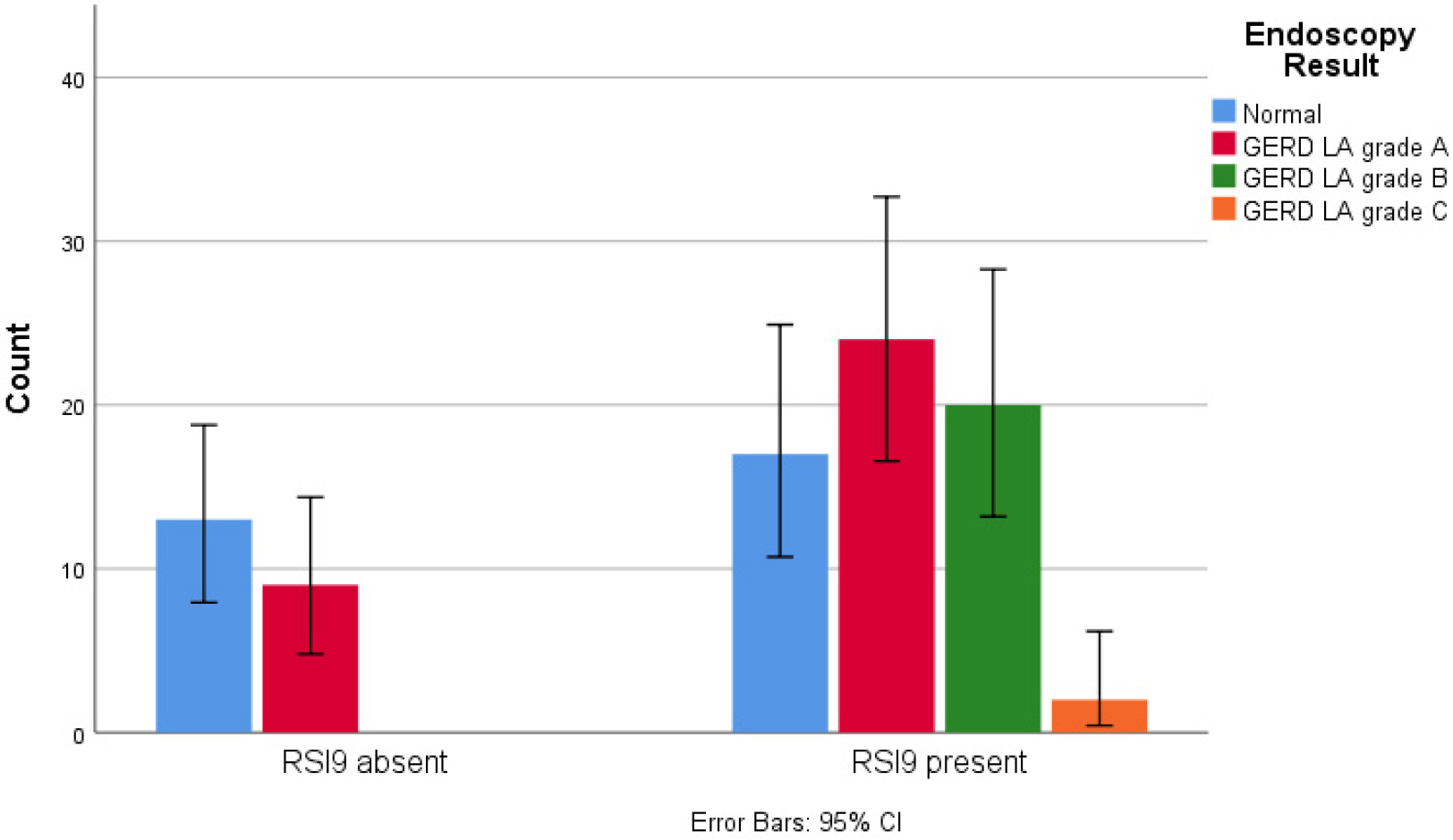
The construct validity of the RSI translated into Bahasa Indonesia was verified with the r value of each question being higher than the crucial table value (r>0.213, p<0.05). Our questionnaire had a Cronbach alpha value of 0.81, which indicates an acceptable level of internal consistency. At least one extra-esophageal symptom was seen in 91.7% of patients with Los Angeles (LA) grade B or higher-grade esophagitis. In addition, the presence of extra-esophageal symptoms was associated with significant mucosal erosion (p=0.20). The symptoms of cough after eating or lying down and chronic cough were associated with the severity of esophageal mucosal erosion (p<0.05).
Conclusions
The version of RSI translated into Bahasa Indonesia is a valid and reliable tool for assessing extra-esophageal GERD symptoms. The occurrence of extra-esophageal symptoms in patients with typical GERD symptoms is associated with endoscopic findings of LA grade B or erosive esophagitis of higher severity.
Keyword
Figure
Reference
-
1. Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R. Global Consensus Group. 2006; The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 101:1900–1920. quiz 1943DOI: 10.1111/j.1572-0241.2006.00630.x. PMID: 16928254.2. Nirwan JS, Hasan SS, Babar ZU, Conway BR, Ghori MU. 2020; Global prevalence and risk factors of gastro-oesophageal reflux disease (GORD): Systematic review with meta-analysis. Sci Rep. 10:5814. DOI: 10.1038/s41598-020-62795-1. PMID: 32242117. PMCID: PMC7118109.3. Syam AF, Sobur CS, Hapsari FCP, Abdullah M, Makmun D. 2017; Prevalence and risk factors of GERD in indonesian population- An internet-based study. Advanced Science Letters. 23:6734–6738. DOI: 10.1166/asl.2017.9384.4. Durazzo M, Lupi G, Cicerchia F, et al. 2020; Extra-esophageal presentation of gastroesophageal reflux disease: 2020 update. J Clin Med. 9:2559. DOI: 10.3390/jcm9082559. PMID: 32784573. PMCID: PMC7465150.5. Jaspersen D, Kulig M, Labenz J, et al. 2003; Prevalence of extra-oesophageal manifestations in gastro-oesophageal reflux disease: an analysis based on the ProGERD Study. Aliment Pharmacol Ther. 17:1515–1520. DOI: 10.1046/j.1365-2036.2003.01606.x. PMID: 12823154.6. Belafsky PC, Postma GN, Koufman JA. 2001; The validity and reliability of the reflux finding score (RFS). Laryngoscope. 111:1313–1317. DOI: 10.1097/00005537-200108000-00001.7. Katz PO, Dunbar KB, Schnoll-Sussman FH, Greer KB, Yadlapati R, Spechler SJ. 2022; ACG clinical guideline for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol. 117:27–56. DOI: 10.14309/ajg.0000000000001538. PMID: 34807007. PMCID: PMC8754510.8. Belafsky PC, Postma GN, Koufman JA. 2002; Validity and reliability of the reflux symptom index (RSI). J Voice. 16:274–277. DOI: 10.1016/S0892-1997(02)00097-8. PMID: 12150380.9. Eckley CA, Tangerina R. 2021; Sensitivity, Specificity, and reproducibility of the Brazilian Portuguese version of the reflux symptom index. J Voice. 35:161.e15–161.e19. DOI: 10.1016/j.jvoice.2019.08.012. PMID: 31586513.10. Calvo-Henríquez C, Ruano-Ravina A, Vaamonde P, et al. 2019; Translation and validation of the reflux symptom index to Spanish. J Voice. 33:807.e1–807.e5. DOI: 10.1016/j.jvoice.2018.04.019. PMID: 30076096.11. Akbulut S, Aydinli FE, Kuşçu O, et al. 2020; Reliability and validity of the Turkish reflux symptom index. J Voice. 34:965.e23–965.e28. DOI: 10.1016/j.jvoice.2019.05.015. PMID: 31248727.12. Włodarczyk E, Jetka T, Miaśkiewicz B, Skarzynski PH, Skarzynski H. 2022; Validation and reliability of Polish version of the reflux symptoms index and reflux finding score. Healthcare (Basel). 10:1411. DOI: 10.3390/healthcare10081411. PMID: 36011068. PMCID: PMC9408310.13. Acquadro C, Conway K, Christelle G, Mear I. 2012. Linguistic validation manual for health outcome assessments. Mapi Institute;Downey, CA:14. Lundell LR, Dent J, Bennett JR, et al. 1999; Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 45:172–180. DOI: 10.1136/gut.45.2.172. PMID: 10403727. PMCID: PMC1727604.15. Sigle D. 2022. Critical values of the Pearson product-moment correlation coefficient. Neag Center for Gifted Education and Talent Development University of Connecticut;Available from: https://researchbasics.education.uconn.edu/r_critical_value_table/. cited 2023 Jan 24.16. George D, Mallery P. 2003. SPSS for windows step by step: A simple guide and reference. 11.0 update. 4th ed. Allyn & Bacon;Boston:17. Cho E, Kim S. 2015; Cronbach's coefficient alpha: Well known but poorly understood. Organizational Research Methods. 18:207–230. DOI: 10.1177/1094428114555994.18. Na'im A SH. 2010. The 2010 Census of the Indonesian Population: Citizenship, Ethnicity, Religion, and Daily Language. Badan Pusat Statistik;Jakarta:19. Lai YC, Wang PC, Lin JC. 2008; Laryngopharyngeal reflux in patients with reflux esophagitis. World J Gastroenterol. 14:4523–4528. DOI: 10.3748/wjg.14.4523. PMID: 18680233. PMCID: PMC2731280.20. Smit CF, van Leeuwen JA, Mathus-Vliegen LM, et al. 2000; Gastropharyngeal and gastroesophageal reflux in globus and hoarseness. Arch Otolaryngol Head Neck Surg. 126:827–830. DOI: 10.1001/archotol.126.7.827. PMID: 10888993.21. Sadiku E, Hasani E, Këlliçi I, et al. 2021; Extra-esophageal symptoms in individuals with and without erosive esophagitis: a case-control study in Albania. BMC Gastroenterol. 21:76. DOI: 10.1186/s12876-021-01658-z. PMID: 33593300. PMCID: PMC7885502.22. Lei WY, Yu HC, Wen SH, et al. 2015; Predictive factors of silent reflux in subjects with erosive esophagitis. Dig Liver Dis. 47:24–29. DOI: 10.1016/j.dld.2014.09.017. PMID: 25308612.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Overlapping Reflux Symptoms in Functional Dyspepsia Are Mostly Unrelated to Gastroesophageal Reflux
- Incidence of Esophagitis in Gastroesophageal Reflux Disease (GERD)
- Is Gastroesophageal Reflux Disease and Achalasia Coincident or Not?
- Obesity and Upper Gastrointestinal Diseases
- Nonerosive Reflux Disease