Diabetes Metab J.
2023 Jul;47(4):470-483. 10.4093/dmj.2023.0036.
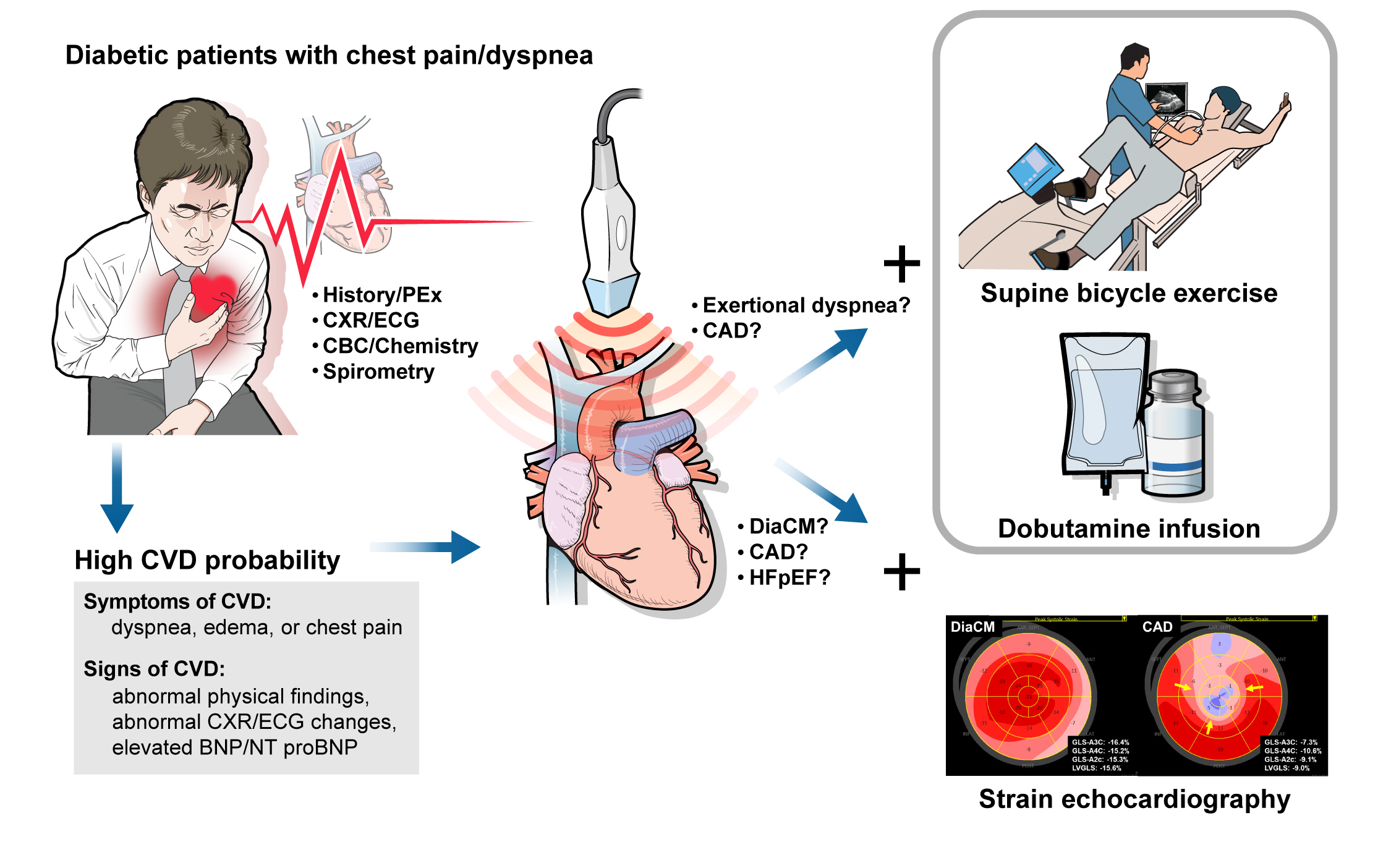
The Role of Echocardiography in Evaluating Cardiovascular Diseases in Patients with Diabetes Mellitus
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Jeonbuk National University Medical School and Research Institute of Clinical Medicine of Jeonbuk National University-Biomedical Research Institute of Jeonbuk National University Hospital, Jeonju, Korea
- 2Division of Cardiology, Department of Internal Medicine, Regional Cardiocerebrovascular Center, Chungnam National University Hospital, Chungnam National University College of Medicine, Daejeon, Korea
- KMID: 2544726
- DOI: http://doi.org/10.4093/dmj.2023.0036
Abstract
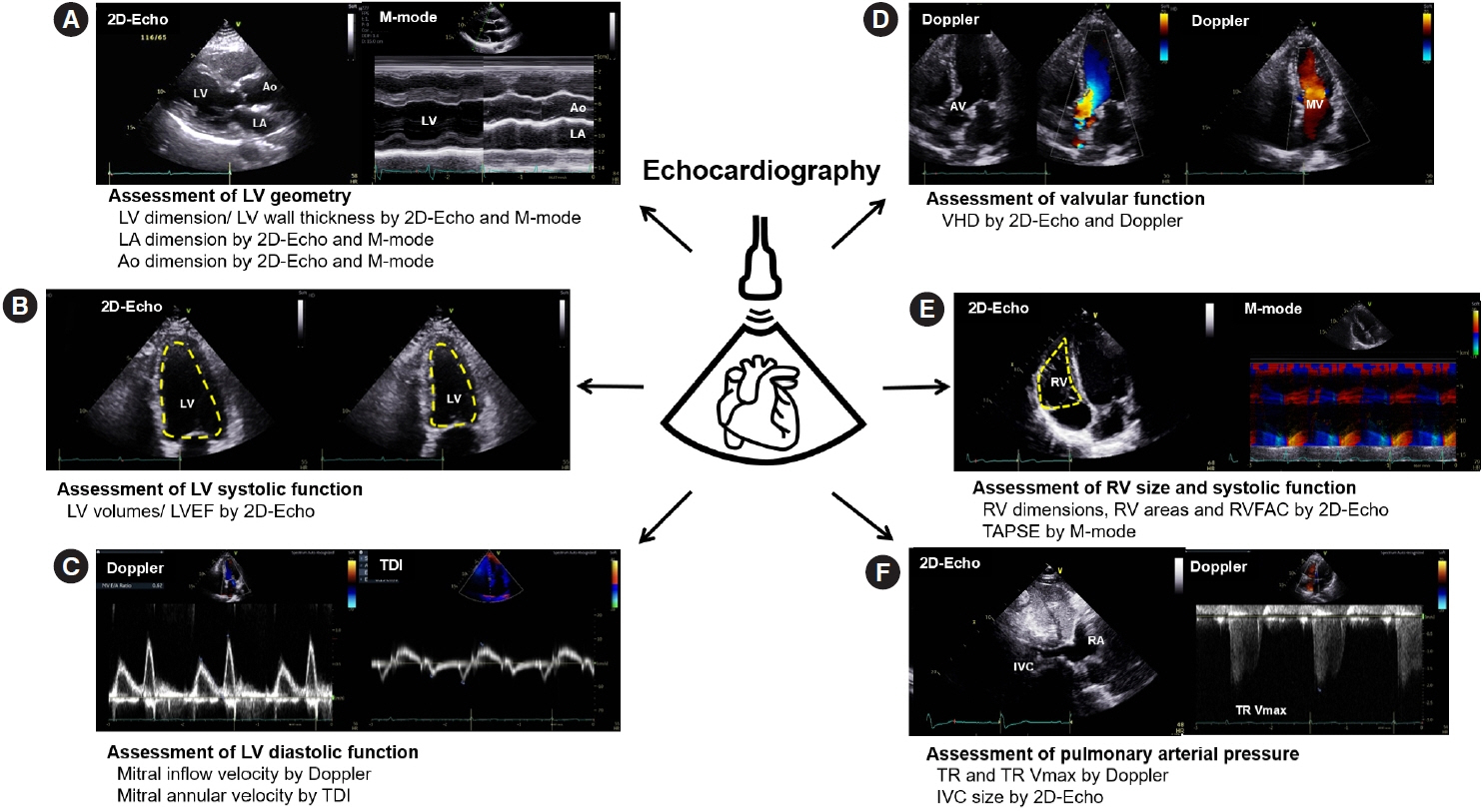
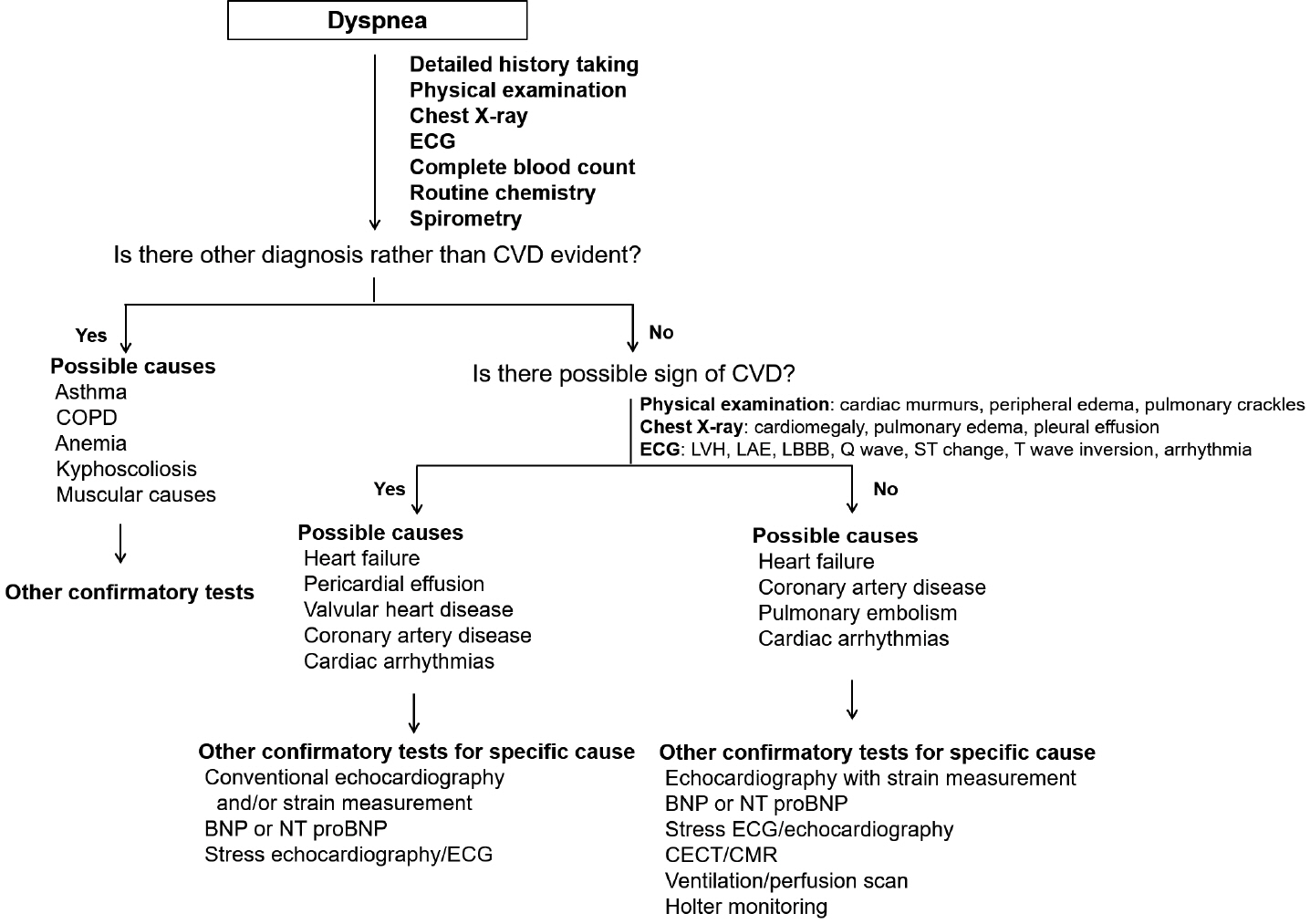
- Patients with diabetes mellitus are highly susceptible to cardiovascular complications, which are directly correlated with cardiovascular morbidity and mortality. In addition to coronary artery disease, there is growing awareness of the risk and prevalence of heart failure (HF) in patients with diabetes. Echocardiography is an essential diagnostic modality commonly performed in patients with symptoms suggestive of cardiovascular diseases (CVD), such as dyspnea or chest pain, to establish or rule out the cause of symptoms. Conventional echocardiographic parameters, such as left ventricular ejection fraction, are helpful not only for diagnosing CVD but also for determining severity, treatment strategy, prognosis, and response to treatment. Echocardiographic myocardial strain, a novel echocardiographic technique, enables the detection of early changes in ventricular dysfunction before HF symptoms develop. This article aims to review the role of echocardiography in evaluating CVD in patients with diabetes mellitus and how to use it in patients with suspected cardiac diseases.
Figure
Reference
-
1. Park JH, Ha KH, Kim BY, Lee JH, Kim DJ. Trends in cardiovascular complications and mortality among patients with diabetes in South Korea. Diabetes Metab J. 2021; 45:120–4.
Article2. Pop-Busui R, Januzzi JL, Bruemmer D, Butalia S, Green JB, Horton WB, et al. Heart failure: an underappreciated complication of diabetes. A consensus report of the American Diabetes Association. Diabetes Care. 2022; 45:1670–90.
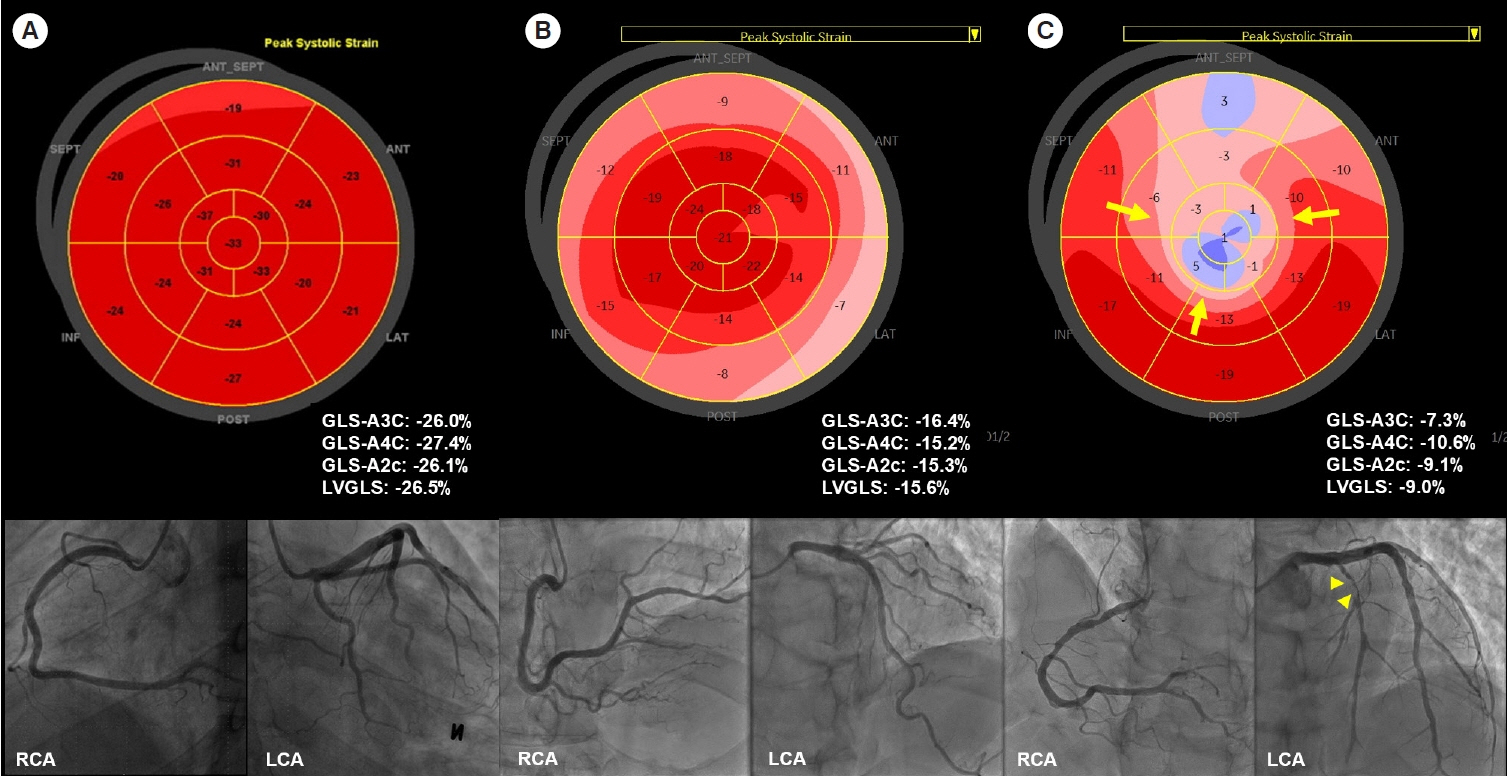
Article3. Park JH. Two-dimensional echocardiographic assessment of myocardial strain: important echocardiographic parameter readily useful in clinical field. Korean Circ J. 2019; 49:908–31.
Article4. Choi W, Kim CH, Hwang IC, Yoon CH, Choi HM, Yoon YE, et al. Three-dimensional myocardial strain for the prediction of clinical events in patients with ST-segment elevation myocardial infarction. J Cardiovasc Imaging. 2022; 30:185–96.
Article5. Malagoli A, Fanti D, Albini A, Rossi A, Ribichini FL, Benfari G. Echocardiographic strain imaging in coronary artery disease: the added value of a quantitative approach. Cardiol Clin. 2020; 38:517–26.6. Marwick TH. Ejection fraction pros and cons: JACC state-of-the-art review. J Am Coll Cardiol. 2018; 72:2360–79.7. Guerreiro RA, Fazendas P, Pereira AR, Marques A, Pais J, Alegria S, et al. Clinical and echocardiographic characterization of false-positive results from stress echocardiography. J Cardiovasc Imaging. 2020; 28:123–33.
Article8. Kim HC, Lee H, Lee HH, Seo E, Kim E, Han J, et al. Korea hypertension fact sheet 2021: analysis of nationwide population-based data with special focus on hypertension in women. Clin Hypertens. 2022; 28:1.
Article9. Al Backr HB, Albacker TB, Elshaer F, Asfina N, AlSubaie FA, Ullah A, et al. Ischemic cardiomyopathy versus non-ischemic cardiomyopathy in diabetic patients: clinical characteristics, management, and long-term outcomes. Am J Cardiovasc Dis. 2022; 12:56–66.10. Standl E, Khunti K, Hansen TB, Schnell O. The global epidemics of diabetes in the 21st century: current situation and perspectives. Eur J Prev Cardiol. 2019; 26(2 Suppl):7–14.
Article11. Leon BM, Maddox TM. Diabetes and cardiovascular disease: epidemiology, biological mechanisms, treatment recommendations and future research. World J Diabetes. 2015; 6:1246–58.12. Rawshani A, Rawshani A, Gudbjornsdottir S. Mortality and cardiovascular disease in type 1 and type 2 diabetes. N Engl J Med. 2017; 377:300–1.
Article13. Gyldenkerne C, Knudsen JS, Olesen KK, Sorensen HT, Botker HE, Thomsen RW, et al. Nationwide trends in cardiac risk and mortality in patients with incident type 2 diabetes: a Danish cohort study. Diabetes Care. 2021; dc210383.
Article14. Shimabukuro M, Saito T, Higa T, Nakamura K, Masuzaki H, Sata M, et al. Risk stratification of coronary artery disease in asymptomatic diabetic subjects using multidetector computed tomography. Circ J. 2015; 79:2422–9.
Article15. Marchant B, Umachandran V, Stevenson R, Kopelman PG, Timmis AD. Silent myocardial ischemia: role of subclinical neuropathy in patients with and without diabetes. J Am Coll Cardiol. 1993; 22:1433–7.
Article16. Duque A, Mediano MF, De Lorenzo A, Rodrigues LF Jr. Cardiovascular autonomic neuropathy in diabetes: pathophysiology, clinical assessment and implications. World J Diabetes. 2021; 12:855–67.
Article17. Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022; 79:e263–421.18. McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Bohm M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021; 42:3599–726.
Article19. Lee HY. Heart failure and diabetes mellitus: dangerous liaisons. Int J Heart Fail. 2022; 4:163–74.
Article20. Kenny HC, Abel ED. Heart failure in type 2 diabetes mellitus. Circ Res. 2019; 124:121–41.
Article21. Dunlay SM, Givertz MM, Aguilar D, Allen LA, Chan M, Desai AS, et al. Type 2 diabetes mellitus and heart failure: a scientific statement from the American Heart Association and the Heart Failure Society of America. This statement does not represent an update of the 2017 ACC/AHA/HFSA heart failure guideline update. Circulation. 2019; 140:e294–324.
Article22. Park JJ, Lee CJ, Park SJ, Choi JO, Choi S, Park SM, et al. Heart failure statistics in Korea, 2020: a report from the Korean Society of Heart Failure. Int J Heart Fail. 2021; 3:224–36.
Article23. Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jodar E, Leiter LA, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016; 375:1834–44.
Article24. McMurray JJ, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014; 371:993–1004.
Article25. Paolillo S, Marsico F, Prastaro M, Renga F, Esposito L, De Martino F, et al. Diabetic cardiomyopathy: definition, diagnosis, and therapeutic implications. Heart Fail Clin. 2019; 15:341–7.26. Jia G, Hill MA, Sowers JR. Diabetic cardiomyopathy: an update of mechanisms contributing to this clinical entity. Circ Res. 2018; 122:624–38.27. Dawson A, Morris AD, Struthers AD. The epidemiology of left ventricular hypertrophy in type 2 diabetes mellitus. Diabetologia. 2005; 48:1971–9.
Article28. Urlic H, Kumric M, Vrdoljak J, Martinovic D, Dujic G, Vilovic M, et al. Role of echocardiography in diabetic cardiomyopathy: from mechanisms to clinical practice. J Cardiovasc Dev Dis. 2023; 10:46.
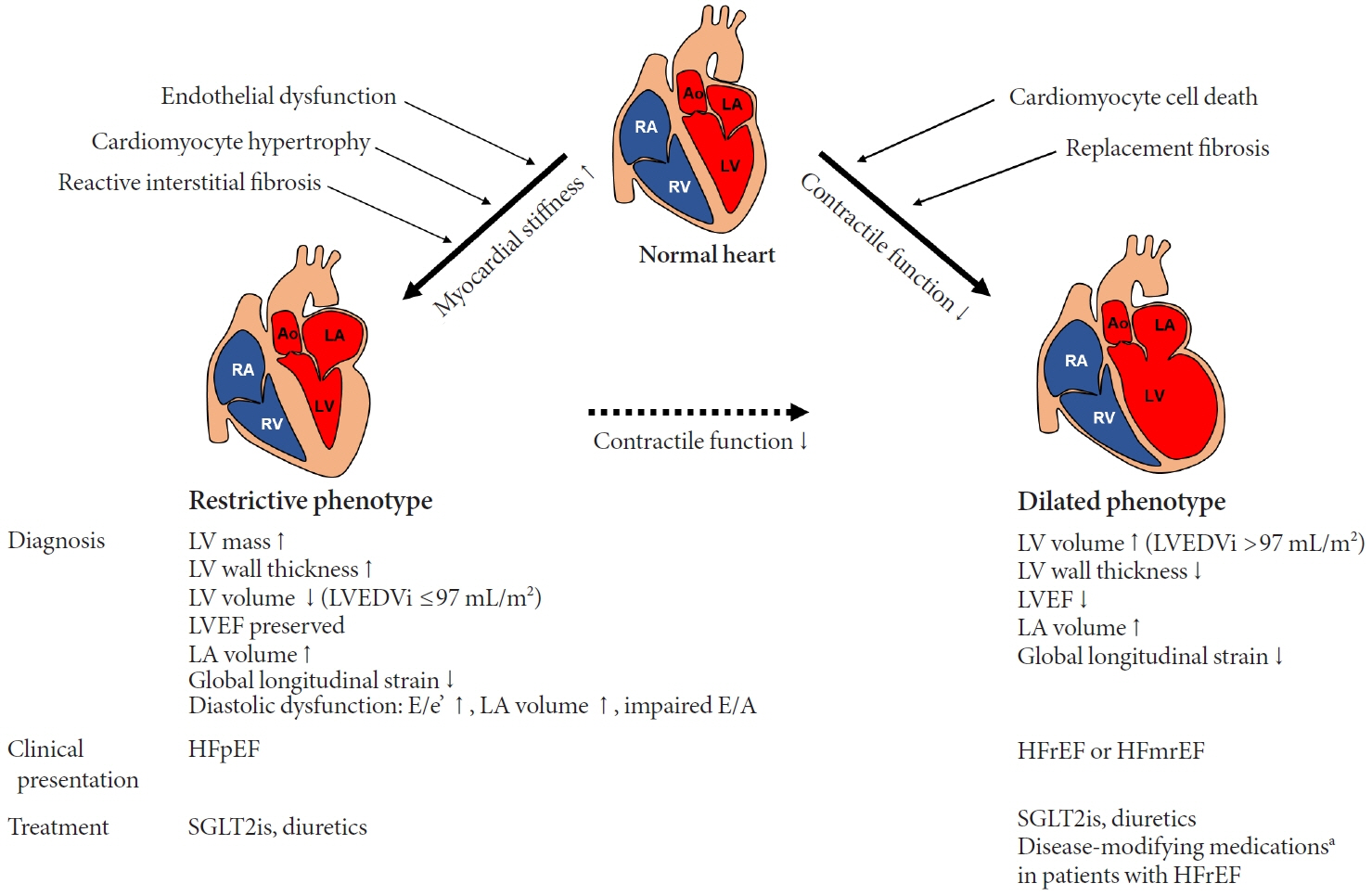
Article29. Kishi S, Gidding SS, Reis JP, Colangelo LA, Venkatesh BA, Armstrong AC, et al. Association of insulin resistance and glycemic metabolic abnormalities with LV structure and function in middle age: the CARDIA study. JACC Cardiovasc Imaging. 2017; 10:105–14.30. Marwick TH, Ritchie R, Shaw JE, Kaye D. Implications of underlying mechanisms for the recognition and management of diabetic cardiomyopathy. J Am Coll Cardiol. 2018; 71:339–51.31. From AM, Scott CG, Chen HH. The development of heart failure in patients with diabetes mellitus and pre-clinical diastolic dysfunction a population-based study. J Am Coll Cardiol. 2010; 55:300–5.32. Murtaza G, Virk HU, Khalid M, Lavie CJ, Ventura H, Mukherjee D, et al. Diabetic cardiomyopathy: a comprehensive updated review. Prog Cardiovasc Dis. 2019; 62:315–26.33. Seferovic PM, Paulus WJ. Clinical diabetic cardiomyopathy: a two-faced disease with restrictive and dilated phenotypes. Eur Heart J. 2015; 36:1718–27.
Article34. Berti M, Pernigo M, Dinatolo E, Cozza F, Cuccia C. Differentiating typical Tako-tsubo syndrome from extensive anterior STEMI: look behind the anterior wall. Echocardiography. 2022; 39:1299–306.
Article35. Farsalinos KE, Daraban AM, Unlu S, Thomas JD, Badano LP, Voigt JU. Head-to-head comparison of global longitudinal strain measurements among nine different vendors: the EACVI/ASE inter-vendor comparison study. J Am Soc Echocardiogr. 2015; 28:1171–81.36. Ferry OR, Huang YC, Masel PJ, Hamilton M, Fong KM, Bowman RV, et al. Diagnostic approach to chronic dyspnoea in adults. J Thorac Dis. 2019; 11(Suppl 17):S2117–28.
Article37. Gulati M, Levy PD, Mukherjee D, Amsterdam E, Bhatt DL, Birtcher KK, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021; 144:e368–454.
Article38. Oh JK, Park JH. Role of echocardiography in acute pulmonary embolism. Korean J Intern Med. 2023; 38:456–70.
Article39. Biswas K, Mukherjee A, Nandi S, Khanra D, Sharma RK, Maji S. Utility of global longitudinal strain to detect significant coronary artery disease, its extent and severity in patients with stable ischemic heart disease. Echocardiography. 2020; 37:2000–9.
Article40. Gupta DK, Wang TJ. Natriuretic peptides and cardiometabolic health. Circ J. 2015; 79:1647–55.
Article41. Zois NE, Bartels ED, Hunter I, Kousholt BS, Olsen LH, Goetze JP. Natriuretic peptides in cardiometabolic regulation and disease. Nat Rev Cardiol. 2014; 11:403–12.
Article42. Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015; 28:1–39.
Article43. Choi HJ. Multi-modality echocardiography for cardiac assessment in fetuses of pregnant women with diabetes mellitus. J Cardiovasc Imaging. 2022; 30:135–7.
Article44. Hamdy RM, Habib SA, Mohamed LA, Abd Elaziz OH. The usefulness of 4D echocardiographic modality for assessing RV affection in uncontrolled hypertensive patients. J Cardiovasc Imaging. 2022; 30:279–89.
Article45. Reddy YN, Carter RE, Obokata M, Redfield MM, Borlaug BA. A simple, evidence-based approach to help guide diagnosis of heart failure with preserved ejection fraction. Circulation. 2018; 138:861–70.
Article46. Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016; 29:277–314.
Article47. Sueta D, Yamamoto E, Nishihara T, Tokitsu T, Fujisue K, Oike F, et al. H2FPEF score as a prognostic value in HFpEF patients. Am J Hypertens. 2019; 32:1082–90.
Article48. Tada A, Nagai T, Omote K, Iwano H, Tsujinaga S, Kamiya K, et al. Performance of the H2FPEF and the HFA-PEFF scores for the diagnosis of heart failure with preserved ejection fraction in Japanese patients: a report from the Japanese multicenter registry. Int J Cardiol. 2021; 342:43–8.
Article49. Park JJ, Park JB, Park JH, Cho GY. Global longitudinal strain to predict mortality in patients with acute heart failure. J Am Coll Cardiol. 2018; 71:1947–57.50. Chaudhury A, Wanek A, Ponnalagu D, Singh H, Kohut A. Use of speckle tracking echocardiography to detect induced regional strain changes in the murine myocardium by acoustic radiation force. J Cardiovasc Imaging. 2021; 29:147–57.
Article51. Wang T, Li L, Huang J, Fan L. Assessment of subclinical left ventricle myocardial dysfunction using global myocardial work in type 2 diabetes mellitus patients with preserved left ventricle ejection fraction. Diabetol Metab Syndr. 2022; 14:17.52. Sun BJ, Park JH. Echocardiographic measurement of left atrial strain: a key requirement in clinical practice. Circ J. 2021; 86:6–13.53. Yoon SJ, Park S, Choi EY, Seo HS, Shim CY, Ahn CM, et al. Left atrial velocity vector imaging can assess early diastolic dysfunction in left ventricular hypertrophy and hypertrophic cardiomyopathy. J Cardiovasc Imaging. 2023; 31:41–8.54. Lorenzo-Almoros A, Tunon J, Orejas M, Cortes M, Egido J, Lorenzo O. Diagnostic approaches for diabetic cardiomyopathy. Cardiovasc Diabetol. 2017; 16:28.55. Yang QM, Fang JX, Chen XY, Lv H, Kang CS. The systolic and diastolic cardiac function of patients with type 2 diabetes mellitus: an evaluation of left ventricular strain and torsion using conventional and speckle tracking echocardiography. Front Physiol. 2022; 12:726719.56. Ghoreyshi-Hefzabad SM, Jeyaprakash P, Gupta A, Vo HQ, Pathan F, Negishi K. Three-dimensional global left ventricular myocardial strain reduced in all directions in subclinical diabetic cardiomyopathy: a systematic review and meta-analysis. J Am Heart Assoc. 2021; 10:e020811.57. Lee LE, Chandrasekar B, Yu P, Ma L. Quantification of myocardial fibrosis using noninvasive T2-mapping magnetic resonance imaging: preclinical models of aging and pressure overload. NMR Biomed. 2022; 35:e4641.
Article58. Kersten J, Hackenbroch C, Bouly M, Tyl B, Bernhardt P. What is normal for an aging heart?: a prospective CMR cohort study. J Cardiovasc Imaging. 2022; 30:202–11.
Article59. Hamdy RM, Osama H, Fereig HM. Evaluation of cardiac mechanical dyssynchrony in heart failure patients using current echo-doppler modalities. J Cardiovasc Imaging. 2022; 30:307–19.
Article60. Lancellotti P, Pellikka PA, Budts W, Chaudhry FA, Donal E, Dulgheru R, et al. The clinical use of stress echocardiography in non-ischaemic heart disease: recommendations from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. Eur Heart J Cardiovasc Imaging. 2016; 17:1191–229.
Article61. Erdei T, Smiseth OA, Marino P, Fraser AG. A systematic review of diastolic stress tests in heart failure with preserved ejection fraction, with proposals from the EU-FP7 MEDIA study group. Eur J Heart Fail. 2014; 16:1345–61.
Article62. Ferrini M, Johansson I, Aboyans V. Heart failure and its complications in patients with diabetes: mounting evidence for a growing burden. Eur J Prev Cardiol. 2019; 26(2 Suppl):106–13.
Article63. Zelniker TA, Wiviott SD, Raz I, Im K, Goodrich EL, Furtado RH, et al. Comparison of the effects of glucagon-like peptide receptor agonists and sodium-glucose cotransporter 2 inhibitors for prevention of major adverse cardiovascular and renal outcomes in type 2 diabetes mellitus. Circulation. 2019; 139:2022–31.
Article64. Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015; 373:2117–28.
Article65. Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017; 377:644–57.
Article66. Giugliano D, Ceriello A, De Nicola L, Perrone-Filardi P, Cosentino F, Esposito K. Primary versus secondary cardiorenal prevention in type 2 diabetes: which newer anti-hyperglycaemic drug matters? Diabetes Obes Metab. 2020; 22:149–57.
Article67. Vaduganathan M, Docherty KF, Claggett BL, Jhund PS, de Boer RA, Hernandez AF, et al. SGLT-2 inhibitors in patients with heart failure: a comprehensive meta-analysis of five randomised controlled trials. Lancet. 2022; 400:757–67.
Article68. Wee CF, Teo YH, Teo YN, Syn NL, See RM, Leong S, et al. Effects of sodium/glucose cotransporter 2 (SGLT2) inhibitors on cardiac imaging parameters: a systematic review and metaanalysis of randomized controlled trials. J Cardiovasc Imaging. 2022; 30:153–68.
Article69. Seferovic PM, Coats AJ, Ponikowski P, Filippatos G, Huelsmann M, Jhund PS, et al. European Society of Cardiology/Heart Failure Association position paper on the role and safety of new glucose-lowering drugs in patients with heart failure. Eur J Heart Fail. 2020; 22:196–213.
Article70. Ikonomidis I, Pavlidis G, Thymis J, Birba D, Kalogeris A, Kousathana F, et al. Effects of glucagon-like peptide-1 receptor agonists, sodium-glucose cotransporter-2 inhibitors, and their combination on endothelial glycocalyx, arterial function, and myocardial work index in patients with type 2 diabetes mellitus after 12-month treatment. J Am Heart Assoc. 2020; 9:e015716.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment Strategy for Diabetes with Cardiovascular Disease
- Stress Echocardiography and Carotid Intima-Media Thickness in Diabetic Patients
- Smoking and Type 2 Diabetes Mellitus
- Non-invasive Methods for Cardiovascular Risk Assessment in Asymptomatic Type 2 Diabetes Mellitus
- The Findings of 2D and M-mode Echocardiography in Young Insulin-Dependent Diabetes Mellitus