Clin Endosc.
2023 Jul;56(4):499-509. 10.5946/ce.2022.208.
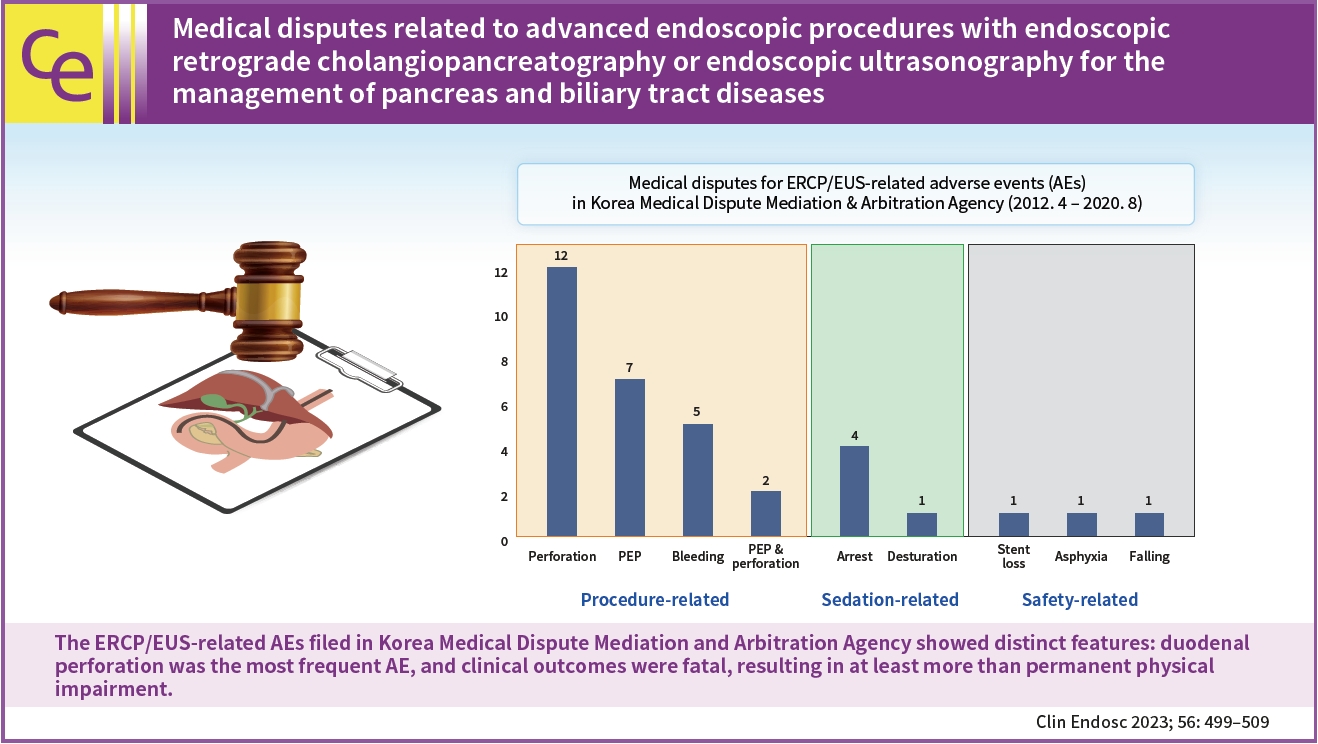
Medical disputes related to advanced endoscopic procedures with endoscopic retrograde cholangiopancreatography or endoscopic ultrasonography for the management of pancreas and biliary tract diseases
- Affiliations
-
- 1Department of Internal Medicine, Inje University Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea
- 2Department of Internal Medicine, Kyung Hee University Medical Center, Seoul, Korea
- 3Department of Internal Medicine, Seoul Medical Center, Seoul, Korea
- 4Department of Internal Medicine, Hanyang University Guri Hospital, Hanyang University College of Medicine, Guri, Korea
- 5Department of Internal Medicine, Ewha Womans University Seoul Hospital, Ewha Women’s University College of Medicine, Seoul, Korea
- 6Department of Internal Medicine, Kyungpook National University School of Medicine, Daegu, Korea
- 7Department of Internal Medicine, Dankook University Hospital, Dankook University College of Medicine, Cheonan, Korea
- 8Department of Internal Medicine, Dongguk University Ilsan Hospital, Dongguk University College of Medicine, Goyang, Korea
- 9Institute for Digestive Research and Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea
- 10Department of Internal Medicine, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea
- KMID: 2544573
- DOI: http://doi.org/10.5946/ce.2022.208
Abstract
- Background/Aims
This study aimed to evaluate the characteristics of endoscopic retrograde cholangiopancreatography (ERCP) or endoscopic ultrasonography (EUS)-related adverse events (AEs) that eventually lead to medical disputes or claims on medical professional liability.
Methods
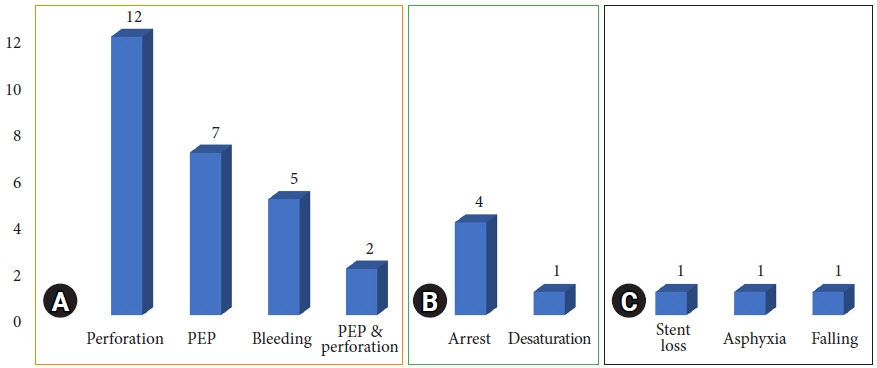
Medical disputes for ERCP/EUS-related AEs filed in the Korea Medical Dispute Mediation and Arbitration Agency between April 2012 and August 2020 were evaluated using corresponding medical records. AEs were categorized into three sections: procedure-related, sedation-related, and safety-related AEs.
Results
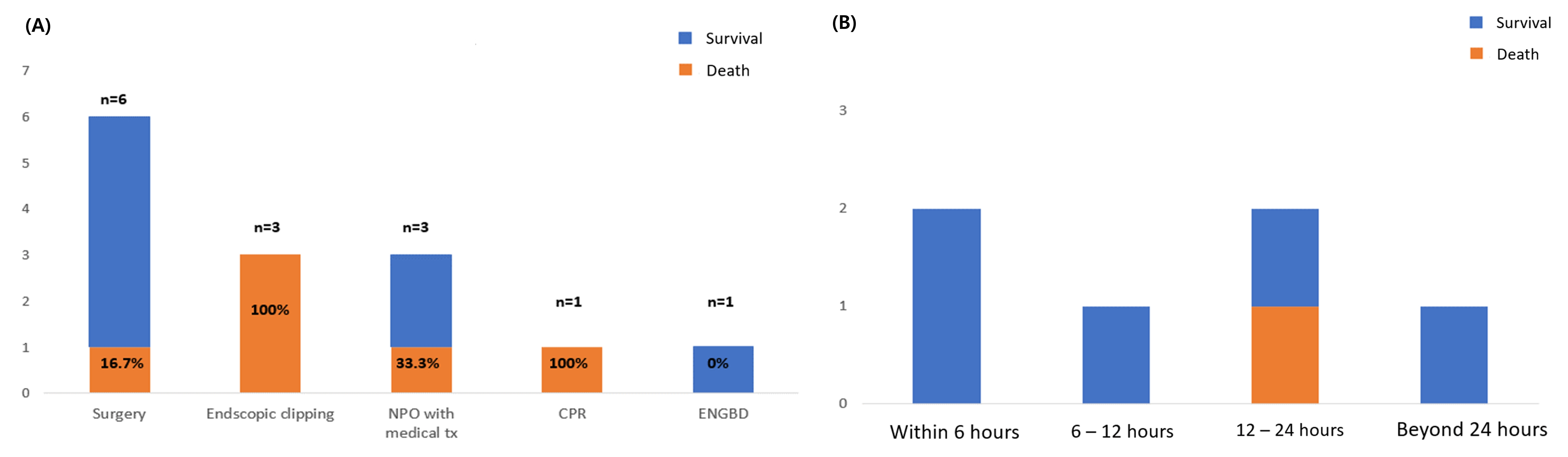
Among a total of 34 cases, procedure-related AEs were 26 (76.5%; 12 duodenal perforations, 7 post-ERCP pancreatitis, 5 bleedings, 2 perforations combined with post-ERCP pancreatitis); sedation-related AEs were 5 (14.7%; 4 cardiac arrests, 1 desaturation), and safety-related AEs were 5 (8.8%; 1 follow-up loss for stent removal, 1 asphyxia, 1 fall). Regarding clinical outcomes, 20 (58.8%) were fatal and eventually succumbed to AEs. For the types of medical institutions, 21 cases (61.8%) occurred at tertiary or academic hospitals, and 13 (38.2%) occurred at community hospitals.
Conclusions
The ERCP/EUS-related AEs filed in Korea Medical Dispute Mediation and Arbitration Agency showed distinct features: duodenal perforation was the most frequent AE, and clinical outcomes were fatal, resulting in at least more than permanent physical impairment.
Keyword
Figure
Reference
-
1. Park JM, Kang CD, Lee JC, et al. Recent 5-year trend of endoscopic retrograde cholangiography in Korea using National Health Insurance Review and Assessment Service open data. Gut Liver. 2020; 14:833–841.2. Ahn DW, Han JH, Kim HJ, et al. Practice of endoscopic retrograde cholangiopancreatography in Korea: results from a national survey. Korean J Pancreas Biliary Tract. 2019; 24:21–30.3. ASGE Standards of Practice Committee, Chandrasekhara V, Khashab MA, et al. Adverse events associated with ERCP. Gastrointest Endosc. 2017; 85:32–47.4. ASGE Standards of Practice Committee, Early DS, Acosta RD, et al. Adverse events associated with EUS and EUS with FNA. Gastrointest Endosc. 2013; 77:839–843.5. Kim YM, Park JJ, Youn YH. Iatrogenic pyriform sinus perforation during endoscopic ultrasonography. Int J Gastrointest Interv. 2019; 8:59–61.6. Verma D, Gostout CJ, Petersen BT, et al. Establishing a true assessment of endoscopic competence in ERCP during training and beyond: a single-operator learning curve for deep biliary cannulation in patients with native papillary anatomy. Gastrointest Endosc. 2007; 65:394–400.7. Paik CN, Ko SW, Cho KB. Certificated system for endoscopic retrograde cholangiopancreatography in foreign countries. Korean J Pancreas Biliary Tract. 2019; 24:51–54.8. Mulder CJ, Jacobs MA, Leicester RJ, et al. Guidelines for designing a digestive disease endoscopy unit: report of the World Endoscopy Organization. Dig Endosc. 2013; 25:365–375.9. Lee JM, Moon SH, Park SW, et al. A national survey on the environment and basic techniques of endoscopic retrograde cholangiopancreatography in Korea. Gut Liver. 2021; 15:904–911.10. Azizian J, Dalai C, Adams MA, et al. Medical professional liability in gastroenterology: definitions, trends, risk factors, provider behaviors, and implications. Expert Rev Gastroenterol Hepatol. 2021; 15:909–918.11. Korea Medical Dispute Mediation and Arbitration Agency. Medical dispute counseling service [Internet]. Seoul: Korea Medical Dispute Mediation and Arbitration Agency;2022. [updated 2022 May 21; cited 2022 May 21]. Available from: https://www.k-medi.or.kr/eng/index.do.12. Cotton PB, Eisen GM, Aabakken L, et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. 2010; 71:446–454.13. Statistics Korea. Population census [Internet]. Daejeon: Korean Statistical Information Service;2022. [cited 2022 Apr 5]. Available from: https://kosis.kr/eng/.14. Yoon SB, Kim J, Paik CN, et al. Trends and characteristics of endoscopic retrograde cholangiopancreatography: a nationwide database study in Korea. Korean J Pancreas Biliary Tract. 2021; 26:186–194.15. Lee HJ, Cho CM, Heo J, et al. Impact of hospital volume and the experience of endoscopist on adverse events related to endoscopic retrograde cholangiopancreatography: a prospective observational study. Gut Liver. 2020; 14:257–264.16. Stapfer M, Selby RR, Stain SC, et al. Management of duodenal perforation after endoscopic retrograde cholangiopancreatography and sphincterotomy. Ann Surg. 2000; 232:191–198.17. Paspatis GA, Dumonceau JM, Barthet M, et al. Diagnosis and management of iatrogenic endoscopic perforations: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy. 2014; 46:693–711.18. Enns R, Eloubeidi MA, Mergener K, et al. ERCP-related perforations: risk factors and management. Endoscopy. 2002; 34:293–298.19. Avgerinos DV, Llaguna OH, Lo AY, et al. Management of endoscopic retrograde cholangiopancreatography: related duodenal perforations. Surg Endosc. 2009; 23:833–838.20. Kochar B, Akshintala VS, Afghani E, et al. Incidence, severity, and mortality of post-ERCP pancreatitis: a systematic review by using randomized, controlled trials. Gastrointest Endosc. 2015; 81:143–149.21. El Zouhairi M, Swartz D, Shah T. Post-ERCP pancreatitis: mechanisms, risk factors, and prevention. Pancreat Disord Ther. 2013; 3:116.22. Choi JH, Kim HJ, Lee BU, et al. Vigorous periprocedural hydration with lactated Ringer’s solution reduces the risk of pancreatitis after retrograde cholangiopancreatography in hospitalized patients. Clin Gastroenterol Hepatol. 2017; 15:86–92.23. Oh HC, El Hajj II, Easler JJ, et al. Post-ERCP bleeding in the era of multiple antiplatelet agents. Gut Liver. 2018; 12:214–218.24. Ferreira LE, Baron TH. Post-sphincterotomy bleeding: who, what, when, and how. Am J Gastroenterol. 2007; 102:2850–2858.25. Burgess NG, Metz AJ, Williams SJ, et al. Risk factors for intraprocedural and clinically significant delayed bleeding after wide-field endoscopic mucosal resection of large colonic lesions. Clin Gastroenterol Hepatol. 2014; 12:651–661.26. Cho IB, Kim SY, Kim DO, et al. The effect of obesity on awareness in general anesthesia with propofol. Korean J Anesthesiol. 2006; 50:379–384.27. Kim J, Lee MJ, Song HC. A clinical study about comparison of inhalation anesthesia and intravenous anesthesia in oral and maxillofacial patients. J Korean Dent Soc Anesthesiol. 2002; 2:15–20.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Training in Endoscopy: Endoscopic Retrograde Cholangiopancreatography
- Monitored Anesthesia Care for Sedation during Endoscopic Retrograde Cholangiopancreatography
- Prevention of Post-endoscopic Retrograde Cholangiopancreatography Pancreatitis: An Endoscopic Perspective
- Introduction to the Rule Book of Pancreatobiliary Endoscopy Certification
- When the Going Gets Tough: Utilization of SpyGlass, or Drainage Followed by Stone Removal