J Korean Med Sci.
2023 Jul;38(27):e208. 10.3346/jkms.2023.38.e208.
Psychological Distress and Perceived Burden in Parents of Korean Children With IgE-Mediated Food Allergy
- Affiliations
-
- 1Department of Pediatrics, Kosin University Gospel Hospital, Kosin University School of Medicine, Busan, Korea
- 2Department of Pediatrics, Hallym University Dongtan Sacred Heart Hospital, Hallym University School of Medicine, Hwaseong, Korea
- 3Department of Pediatrics, Pusan National University Hospital, Busan, Korea
- 4Department of Pediatrics, Chungnam National University Sejong Hospital, Chungnam National University College of Medicine, Sejong, Korea
- 5Department of Pediatrics, Chuncheon Sacred Heart Hospital, Hallym University School of Medicine, Chuncheon, Korea
- 6Department of Occupational and Environmental Medicine, Seoul Medical Center, Seoul, Korea
- 7Korea University Graduate School of Public Health, Seoul, Korea
- 8Seoul Medical Book and Publishing, Jeju, Korea
- 9Biomedical Statistics Center, Research Institute for Future Medicine, Samsung Medical Center, Seoul, Korea
- 10Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 11Department of Health Sciences and Technology, Samsung Advanced Institute for Health Sciences & Technology, Seoul, Korea
- KMID: 2544412
- DOI: http://doi.org/10.3346/jkms.2023.38.e208
Abstract
- Background
Food allergy (FA) can have a profound effect on quality of life (QoL), stress, and anxiety in the family. We aimed to validate the Korean version of the Food Allergy Quality of Life-Parental Burden (FAQL-PB) and identify factors related to the parental psychosocial burden of caring for children with FAs.
Methods
Parents of children aged between 6 months and 17 years with immunoglobulin E (IgE)-mediated FAs from the Pediatric Allergy Department of five university hospitals in Korea were enrolled in the study. Parents were asked to complete the FAQL-PB, Food Allergy Independent Measure-Parent Form (FAIM-PF), Child Health Questionnaire-Parents Form 28 (CHQ-PF28), Beck’s Anxiety Inventory, Connor-Davidson Resilience Scale, and Patient Health Questionnaire-9 for depression. Statistical analyses included internal consistency, test-retest reliability, concurrent validity, discriminative validity, and logistic regression analyses.
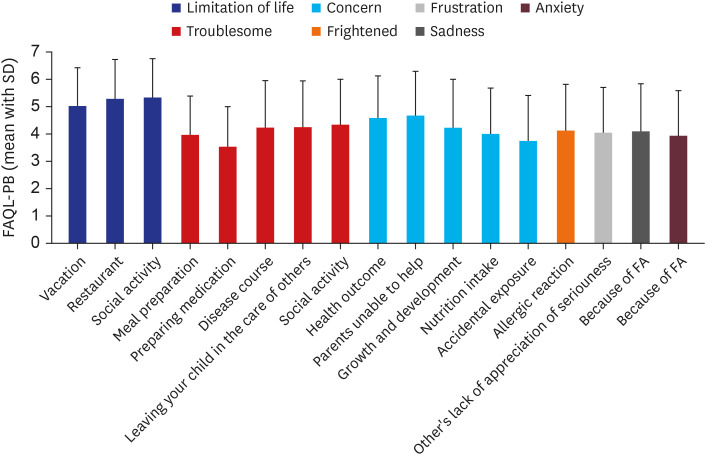
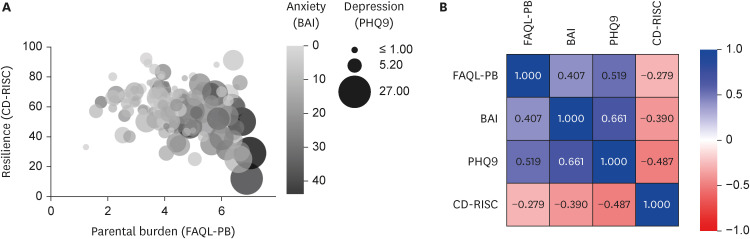
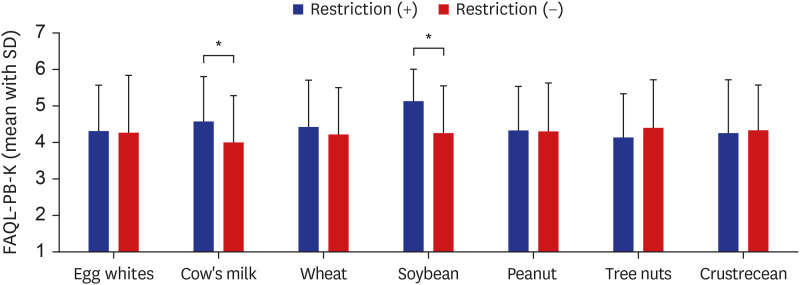
Results
A total of 190 parents were enrolled. Social activity limitation was the item with the highest FAQL-PB scores. The Cronbach’s α for each item was higher than 0.8. The test-retest reliability was good (intra-class correlation coefficient, 0.716; 95% confidence interval [CI], 0.100–0.935). An increase in the FAQL-PB was significantly associated with an increase in the FAIM-PF (β = 0.765, P < 0.001) (concurrent validity). There was a positive correlation between parental burden, anxiety, and depression, while resilience was inversely correlated with parental burden (all P < 0.001). The total FAQL-PB score in parents of children who had experienced anaphylaxis was significantly higher than that in parents of children who did not experience it (P = 0.008). When adjusting for age, sex, and underlying diseases, anaphylaxis β = 9.32; 95% CI, 2.97 to 15.68), cow’s milk (CM) allergy (β = 8.24; 95% CI, 2.04 to 14.44), soybean allergy (β = 13.91; 95% CI, 1.62 to 26.20), higher anxiety (β = 1.05; 95% CI, 0.07 to 1.41), higher depression (β = 2.15; 95% CI, 1.61 to 2.69), and lower resilience (β = −0.42; 95% CI, −0.61 to −0.2) were significantly associated with greater parental burden in children with IgE-mediated FAs.
Conclusion
FAQL-PB is a reliable and valid tool for use in Korea. Anaphylaxis, CM or soybean allergies, more anxiety and depression symptoms, and lower resilience are associated with poorer QoL in parents of children with FAs.
Keyword
Figure
Reference
-
1. Pettersson ME, Koppelman GH, Flokstra-de Blok BMJ, Kollen BJ, Dubois AEJ. Prediction of the severity of allergic reactions to foods. Allergy. 2018; 73(7):1532–1540. PMID: 29380392.2. Li J, Ogorodova LM, Mahesh PA, Wang MH, Fedorova OS, Leung TF, et al. Comparative study of food allergies in children from China, India, and Russia: the EuroPrevall-INCO surveys. J Allergy Clin Immunol Pract. 2020; 8(4):1349–1358.e16. PMID: 31857266.3. Sampath V, Abrams EM, Adlou B, Akdis C, Akdis M, Brough HA, et al. Food allergy across the globe. J Allergy Clin Immunol. 2021; 148(6):1347–1364. PMID: 34872649.4. Jeon YH, Lee S, Ahn K, Lee SY, Kim KW, Kim HH, et al. Infantile anaphylaxis in Korea: a multicenter retrospective case study. J Korean Med Sci. 2019; 34(13):e106. PMID: 30950251.5. Turner PJ, Jerschow E, Umasunthar T, Lin R, Campbell DE, Boyle RJ. Fatal anaphylaxis: mortality rate and risk factors. J Allergy Clin Immunol Pract. 2017; 5(5):1169–1178. PMID: 28888247.6. Roberts G, Allen K, Ballmer-Weber B, Clark A, Crevel R, Dunn Galvin A, et al. Identifying and managing patients at risk of severe allergic reactions to food: report from two iFAAM workshops. Clin Exp Allergy. 2019; 49(12):1558–1566. PMID: 31631439.7. Mehta H, Groetch M, Wang J. Growth and nutritional concerns in children with food allergy. Curr Opin Allergy Clin Immunol. 2013; 13(3):275–279. PMID: 23510952.8. Golding MA, Gunnarsson NV, Middelveld R, Ahlstedt S, Protudjer JL. A scoping review of the caregiver burden of pediatric food allergy. Ann Allergy Asthma Immunol. 2021; 127(5):536–547.e3. PMID: 33971359.9. Warren CM, Jiang J, Gupta RS. Epidemiology and burden of food allergy. Curr Allergy Asthma Rep. 2020; 20(2):6. PMID: 32067114.10. Acaster S, Gallop K, de Vries J, Marciniak A, Ryan R, Vereda A, et al. Psychosocial and productivity impact of caring for a child with peanut allergy. Allergy Asthma Clin Immunol. 2020; 16(1):83. PMID: 32983241.11. Lee Y, Chang HY, Kim SH, Yang MS, Koh YI, Kang HR, et al. A prospective observation of psychological distress in patients with anaphylaxis. Allergy Asthma Immunol Res. 2020; 12(3):496–506. PMID: 32141262.12. Proctor KB, Tison K, H Estrem H, Park J, Scahill L, Vickery BP, et al. A systematic review of parent report measures assessing the psychosocial impact of food allergy on patients and families. Allergy. 2022; 77(5):1347–1359. PMID: 34647344.13. Cohen BL, Noone S, Muñoz-Furlong A, Sicherer SH. Development of a questionnaire to measure quality of life in families with a child with food allergy. J Allergy Clin Immunol. 2004; 114(5):1159–1163. PMID: 15536425.14. Arasi S, Otani IM, Klingbeil E, Bégin P, Kearney C, Dominguez TL, et al. Two year effects of food allergen immunotherapy on quality of life in caregivers of children with food allergies. Allergy Asthma Clin Immunol. 2014; 10(1):57. PMID: 25788951.15. Ward C, Greenhawt M. Differences in caregiver food allergy quality of life between tertiary care, specialty clinic, and caregiver-reported food allergic populations. J Allergy Clin Immunol Pract. 2016; 4(2):257–64.e3. PMID: 26433752.16. Lee E, Kim K. Parental burden of food-allergic children’s parents and influencing factors. J Nutr Health. 2018; 51(2):140.17. Knibb RC, Stalker C. Validation of the food allergy quality of life-parental burden questionnaire in the UK. Qual Life Res. 2013; 22(7):1841–1849. PMID: 23076799.18. DunnGalvin A, de BlokFlokstra BM, Burks AW, Dubois AE, Hourihane JO. Food allergy QoL questionnaire for children aged 0-12 years: content, construct, and cross-cultural validity. Clin Exp Allergy. 2008; 38(6):977–986. PMID: 18435800.19. Bae SC, Ruperto N, Lee JH, Uhm WS, Park YW, Kim SY, et al. The Korean version of the Childhood Health Assessment Questionnaire (CHAQ) and the Child Health Questionnaire (CHQ). Clin Exp Rheumatol. 2001; 19(4):Suppl 23. S96–100. PMID: 11510340.20. Raat H, Botterweck AM, Landgraf JM, Hoogeveen WC, Essink-Bot ML. Reliability and validity of the short form of the Child Health Questionnaire for Parents (CHQ-PF28) in large random school based and general population samples. J Epidemiol Community Health. 2005; 59(1):75–82. PMID: 15598731.21. Lim SY, Lee EJ, Jeong SW, Kim HC, Jeong CH, Jeon TY, et al. Validation study of Beck Depression Scale 2 in Korean version. Anxiety Mood. 2011; 7:48–53.22. Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988; 56(6):893–897. PMID: 3204199.23. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001; 16(9):606–613. PMID: 11556941.24. Baek HS, Lee KU, Joo EJ, Lee MY, Choi KS. Reliability and validity of the Korean version of the Connor-Davidson Resilience scale. Psychiatry Investig. 2010; 7(2):109–115.25. Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience scale (CD-RISC). Depress Anxiety. 2003; 18(2):76–82. PMID: 12964174.26. Kim HS, Oh CY, Ahn KH. A survey on public perceptions of low fertility: a social research panel study. J Korean Med Sci. 2022; 37(25):e203. PMID: 35762146.27. Scott NW, Fayers PM, Aaronson NK, Bottomley A, de Graeff A, Groenvold M, et al. The relationship between overall quality of life and its subdimensions was influenced by culture: analysis of an international database. J Clin Epidemiol. 2008; 61(8):788–795. PMID: 18359194.28. Pappalardo AA, Herbert L, Warren C, Lombard L, Ramos A, Asa’ad A, et al. Self-efficacy among caregivers of children with food allergy: a cohort study. J Pediatr Psychol. 2022; 47(6):674–684. PMID: 35079803.29. Howe L, Franxman T, Teich E, Greenhawt M. What affects quality of life among caregivers of food-allergic children? Ann Allergy Asthma Immunol. 2014; 113(1):69–74.e2. PMID: 24950845.30. Allen CW, Bidarkar MS, vanNunen SA, Campbell DE. Factors impacting parental burden in food-allergic children. J Paediatr Child Health. 2015; 51(7):696–698. PMID: 25594910.31. Pouessel G, Antoine M, Lejeune S, Dubos F, Pierache A, Deschildre A, et al. The time course of anaphylaxis manifestations in children is diverse and unpredictable. Clin Exp Allergy. 2020; 50(1):117–120. PMID: 31594029.32. Boaventura RM, Mendonça RB, Fonseca FA, Mallozi M, Souza FS, Sarni RO. Nutritional status and food intake of children with cow’s milk allergy. Allergol Immunopathol (Madr). 2019; 47(6):544–550. PMID: 31167726.33. Abrams EM, Kim H, Gerdts J, Protudjer JL. Milk allergy most burdensome in multi-food allergic children. Pediatr Allergy Immunol. 2020; 31(7):827–834. PMID: 32413203.34. Rizzo G, Baroni L. Soy, soy foods and their role in vegetarian diets. Nutrients. 2018; 10(1):43. PMID: 29304010.35. Baek Y, Shim JE, Song S. Dietary intake of fat and fatty acids by 1-5-year-old children in Korea: a cross-sectional study based on data from the sixth Korea National Health and Nutrition Examination Survey. Nutr Res Pract. 2018; 12(4):324–335. PMID: 30090170.36. Lee C, Kim S, Jeong S, Lim C, Kim J, Kim Y, et al. MIND dataset for diet planning and dietary healthcare with machine learning: Dataset creation using combinatorial optimization and controllable generation with domain experts. Vanschoren J, Yeung S, editors. Proceedings of the Neural Information Processing Systems Track on Datasets and Benchmarks 1 (NeurIPS Datasets and Benchmarks 2021). Red Hook, NY, USA: Curran Associates Inc;2021. p. 1–13.37. Lau GY, Patel N, Umasunthar T, Gore C, Warner JO, Hanna H, et al. Anxiety and stress in mothers of food-allergic children. Pediatr Allergy Immunol. 2014; 25(3):236–242. PMID: 24750570.38. Birdi G, Cooke R, Knibb R. Quality of Life, stress, and mental health in parents of children with parentally diagnosed food allergy compared to medically diagnosed and healthy controls. J Allergy (Cairo). 2016; 2016:1497375. PMID: 27429624.39. Oh H, Park K, Yoon S, Kim Y, Lee SH, Choi YY, et al. Clinical utility of Beck Anxiety Inventory in clinical and nonclinical Korean samples. Front Psychiatry. 2018; 9:666. PMID: 30564158.40. Rubeiz CJ, Ernst MM. Psychosocial aspects of food allergy: resiliency, challenges and opportunities. Immunol Allergy Clin North Am. 2021; 41(2):177–188. PMID: 33863478.41. Shin YC, Kim SM, Kim H, Min KJ, Yoo SK, Kim EJ, et al. Resilience as a protective factor for depressive mood and anxiety among Korean employees. J Korean Med Sci. 2019; 34(27):e188. PMID: 31293112.42. Knibb RC, Barnes C, Stalker C. Parental self-efficacy in managing food allergy and mental health predicts food allergy-related quality of life. Pediatr Allergy Immunol. 2016; 27(5):459–464. PMID: 27019307.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The status of food allergy and parental burden of preschoolers in Jeju area
- The Diagnosis of Food Allergy in a Pediatric Gastroenterology: Focusing on Non-IgE-mediated Allergic Diseases
- Clinical Perspectives of Food Allergy in Infants and Young Children
- Food Allergy in Children
- Parental burden of food-allergic children's parents and influencing factors