Obstet Gynecol Sci.
2023 Jul;66(4):327-335. 10.5468/ogs.23057.
Relationship between female sexual function, vaginal volume, vaginal resting tone, and pelvic floor muscle strength in women with stress urinary incontinence
- Affiliations
-
- 1Department of Physical Therapy, College of Health Science, Laboratory of Kinetic Ergocise Based on Movement Analysis, Yonsei University, Wonju, Korea
- 2Sophie-Marceau Women’s Clinic, Daegu, Korea
- KMID: 2544388
- DOI: http://doi.org/10.5468/ogs.23057
Abstract
Objective
Vaginal morphology and pelvic floor muscle (PFM) strength may influence sexual stimulation, sensation, and orgasmic response. This study aimed to determine the relationship between female sexual function and PFM strength and vaginal morphology (represented by vaginal resting tone and vaginal volume) in women with stress urinary incontinence (SUI).
Methods
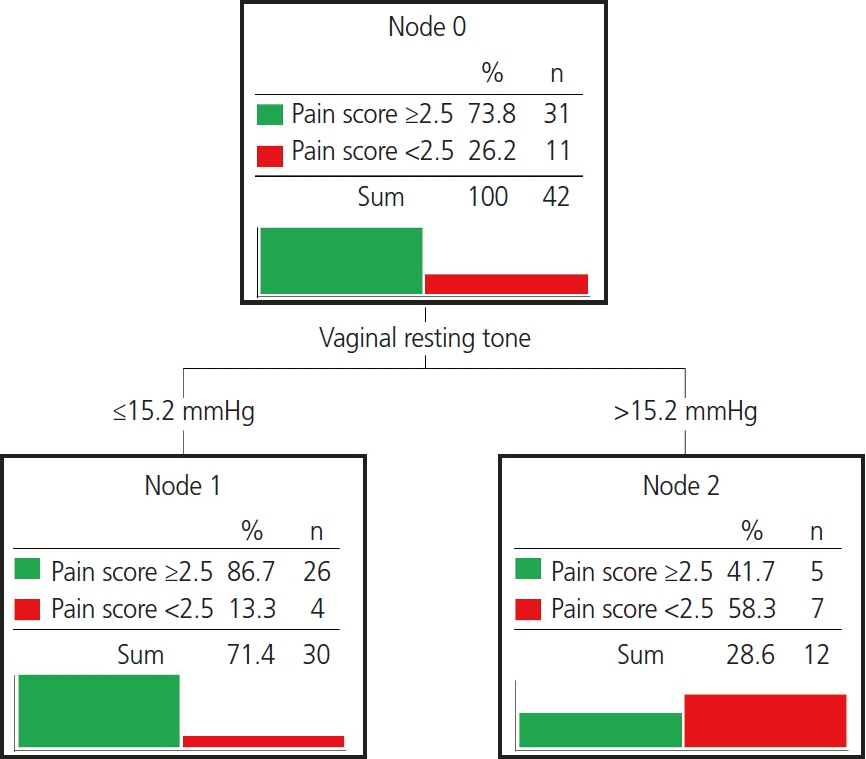
Forty-two subjects with SUI were recruited for the study. Female sexual function was measured using the female sexual function index (FSFI) questionnaire. PFM strength was measured by digital palpation. Vaginal resting tone (mmHg) and vaginal volume (mL) were measured using a perineometer. The significance of the correlations between female sexual function and PFM function and hip muscle strength was assessed using Pearson’s correlation coefficients. If a significant correlation between vaginal morphology and FSFI score was confirmed using Pearson’s correlation, the cutoff value was confirmed through a decision tree.
Results
PFM strength was significantly correlated with desire (r=0.397), arousal (r=0.388), satisfaction (r=0.326), and total (r=0.315) FSFI scores. Vaginal resting tone (r=-0.432) and vaginal volume (r=0.332) were significantly correlated with the FSFI pain score. The cutoff point of vaginal resting tone for the presence of pain-related sexual dysfunction was >15.2 mmHg.
Conclusion
PFM strength training should be the first strategy to improve female sexual function. Additionally, because of the relationship between vaginal morphology and pain-related sexual dysfunction, surgical procedures to achieve vaginal rejuvenation should be carefully considered.
Figure
Cited by 1 articles
-
Combined effects of high-intensity focused electromagnetic therapy and pelvic floor exercises on pelvic floor muscles and sexual function in postmenopausal women
Saher Lotfy Elgayar
Obstet Gynecol Sci. 2024;67(6):574-585. doi: 10.5468/ogs.24103.
Reference
-
References
1. Moore RD, Miklos JR. Vaginal reconstruction and rejuvenation surgery: is there data to support improved sexual function? AJCS. 2012; 29:97–113.
Article2. Griffiths A, Watermeyer S, Sidhu K, Amso NN, Nix B. Female genital tract morbidity and sexual function following vaginal delivery or lower segment caesarean section. J Obstet Gynaecol. 2006; 26:645–9.
Article3. Pauls RN, Occhino JA, Dryfhout VL. Effects of pregnancy on female sexual function and body image: a prospective study. J Sex Me. 2008; 5:1915–22.
Article4. Safarinejad MR, Kolahi AA, Hosseini L. RETRACTED: the effect of the mode of delivery on the quality of life, sexual function, and sexual satisfaction in primiparous women and their husbands. J Sex Med. 2009; 6:165–67.
Article5. Hwang UJ, Kwon OY, Lee MS. Effects of surface electrical stimulation during sitting on pelvic floor muscle function and sexual function in women with stress urinary incontinence. Obstet Gynecol Sci. 2020; 63:370–8.
Article6. Abramov Y, Gandhi S, Botros SM, Goldberg RP, Sherman W, Rurak M, et al. Do alterations in vaginal dimensions after reconstructive pelvic surgeries affect the risk for dyspareunia? Am J Obstet Gynecol. 2005; 192:1573–7.
Article7. Weber AM, Walters MD, Piedmonte MR. Sexual function and vaginal anatomy in women before and after surgery for pelvic organ prolapse and urinary incontinence. Am J Obstet Gynecol. 2000; 182:1610–5.
Article8. Zahariou AG, Karamouti MV, Papaioannou PD. Pelvic floor muscle training improves sexual function of women with stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2008; 19:401–6.
Article9. Bø K, Talseth T, Vinsnes A. Randomized controlled trial on the effect of pelvic floor muscle training on quality of life and sexual problems in genuine stress incontinent women. Acta Obstet Gynecol Scand. 2000; 79:598–603.
Article10. Messelink B, Benson T, Berghmans B, Bø K, Corcos J, Fowler C, et al. Standardization of terminology of pelvic floor muscle function and dysfunction: report from the pelvic floor clinical assessment group of the International Continence Society. Neurourol Urodyn. 2005; 24:374–80.
Article11. Haylen BT, De Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010; 29:4–20.
Article12. Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009; 41:1149–60.
Article13. Hwang UJ, Lee MS, Jung SH, Ahn SH, Kwon OY. Relationship between sexual function and pelvic floor and hip muscle strength in women with stress urinary incontinence. Sex Med. 2021; 9:100325.
Article14. Hwang UJ. Is there an association between the quality of life of incontinence symptoms and the hip joint muscles strength in women with stress urinary incontinence? J Musculoskelet Sci Technol. 2022; 6:15–21.
Article15. Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The female sexual function index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000; 26:191–208.
Article16. Kim HY, So HS, Park KS, Jeong SJ, Lee JY, Ryu SB. Development of the Korean-version of female sexual function index (FSFI). Korean J Androl. 2002; 50–6.17. Bø K, Sherburn M. Evaluation of female pelvic-floor muscle function and strength. Phys Ther. 2005; 85:269–82.
Article18. Devreese A, Staes F, De Weerdt W, Feys H, Van Assche A, Penninckx F, et al. Clinical evaluation of pelvic floor muscle function in continent and incontinent women. Neurourol Urodyn. 2004; 23:190–7.
Article19. Albrich S, Steetskamp J, Knoechel SL, Porta S, Hoffmann G, Skala C. Assessment of pelvic floor muscle contractility: digital palpation versus 2D and 3D perineal ultrasound. Arch Gynecol Obstet. 2016; 293:839–43.
Article20. Portney LG, Watkins MP. Foundations of clinical research: applications to practice. 3rd ed. Upper Saddle River: Pearson/Prentice Hall;2009.21. Hwang UJ, Kwon OY, Yi CH, Jeon HS, Weon JH, Ha SM. Predictors of upper trapezius pain with myofascial trigger points in food service workers: the STROBE study. Medicine (Baltimore). 2017; 96:e7252.22. Jiann BP, Su CC, Yu CC, Wu TT, Huang JK. Risk factors for individual domains of female sexual function. J Sex Med. 2009; 6:3364–75.
Article23. Addis IB, Van Den Eeden SK, Wassel-Fyr CL, Vittinghoff E, Brown JS, Thom DH, et al. Sexual activity and function in middle-aged and older women. Obstet Gynecol. 2006; 107:755–64.
Article24. Chedraui P, Perez-Lopez FR, San Miguel G, Avila C. Assessment of sexuality among middle-aged women using the female sexual function index. Climacteric. 2009; 12:213–21.
Article25. Barbara G, Facchin F, Buggio L, Alberico D, Frattaruolo MP, Kustermann A. Vaginal rejuvenation: current perspectives. Int J Womens Health. 2017; 9:513–9.
Article26. Ferreira CH, Dwyer PL, Davidson M, De Souza A, Ugarte JA, Frawley HC. Does pelvic floor muscle training improve female sexual function? A systematic review. Int Urogynecol J. 2015; 26:1735–50.
Article27. Shafik A. The role of the levator ani muscle in evacuation, sexual performance and pelvic floor disorders. Int Urogynecol J Pelvic Floor Dysfunct. 2000; 11:361–76.
Article28. Giuseppe PG, Pace G, Vicentini C. Sexual function in women with urinary incontinence treated by pelvic floor transvaginal electrical stimulation. J Sex Med. 2007; 4:702–7.
Article29. Mercier J, Tang A, Morin M, Khalifé S, Lemieux MC, Reichetzer B, et al. Test-retest reliability of clitoral blood flow measurements using color Doppler ultrasonography at rest and after a pelvic floor contraction task in healthy adult women. Neurourol Urodyn. 2018; 37:2249–56.
Article30. Ma Y, Qin H. Pelvic floor muscle exercises may improve female sexual function. Med Hypotheses. 2009; 72:223.
Article31. Swift S, Woodman P, O’Boyle A, Kahn M, Valley M, Bland D, et al. Pelvic organ support study (POSST): the distribution, clinical definition, and epidemiologic condition of pelvic organ support defects. Am J Obstet Gynecol. 2005; 192:795–806.
Article32. Schimpf MO, Harvie HS, Omotosho TB, Epstein LB, Jean-Michel M, Olivera CK, et al. Does vaginal size impact sexual activity and function? Int Urogynecol J. 2010; 21:447–52.
Article33. Kim-Fine S, Antosh DD, Balk EM, Meriwether KV, Kanter G, Dieter AA, et al. Relationship of postoperative vaginal anatomy and sexual function: a systematic review with meta-analysis. Int Urogynecol J. 2021; 32:2125–34.
Article34. Goldfinger C, Pukall CF, Gentilcore-Saulnier E, McLean L, Chamberlain S. A prospective study of pelvic floor physical therapy: pain and psychosexual outcomes in provoked vestibulodynia. J Sex Med. 2009; 6:1955–68.35. Piassarolli VP, Hardy E, Andrade NF, Ferreira Nde O, Osis MJ. Pelvic floor muscle training in female sexual dysfunctions. Rev Bras Ginecol Obstet. 2010; 32:234–40.36. Kim SR, Suh DH, Kim W, Jeon MJ. Current techniques used to perform surgery for anterior and posterior vaginal wall prolapse in South Korea. Obstet Gynecol Sci. 2022; 65:273–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Assessment of Pelvic Floor Muscle Exercise using Vaginal Cone in Stress Urinary Incontinence of Korea Women
- The Effect of Pelvic Muscle Exercise Program on Women with Stress Urinary Incontinence in the Degree and Amount of Urinary Incontinence and Maximum Vaginal Contraction Pressure
- Effects of Electric Stimulation and Biofeedback for Pelvic Floor Muscle Exercise in Women with Vaginal Rejuvenation Women
- The Effect of Pelvic Floor Muscle Exercise Using Biofeedback for Stress Urinary Incontinence
- The Efficacy of Pelvic Floor Muscle Exercise in Patients with Genuine Stress Incontinence