Obstet Gynecol Sci.
2023 Jul;66(4):300-306. 10.5468/ogs.23089.
Diagnostic accuracy of hand-held colposcope (Gynocular) in comparison with standard colposcope in patients with abnormal cervical cytology or visual inspection with acetic acid positivity: a cross over randomized controlled study
- Affiliations
-
- 1Department of Obstetrics and Gynaecology, Jipmer Hospital, Pondicherry, India
- KMID: 2544385
- DOI: http://doi.org/10.5468/ogs.23089
Abstract
Objective
To compare the diagnostic accuracy of a handheld colposcope (Gynocular) versus a standard colposcope in women with abnormal cervical cytology or visual Inspection with acetic acid positivity.
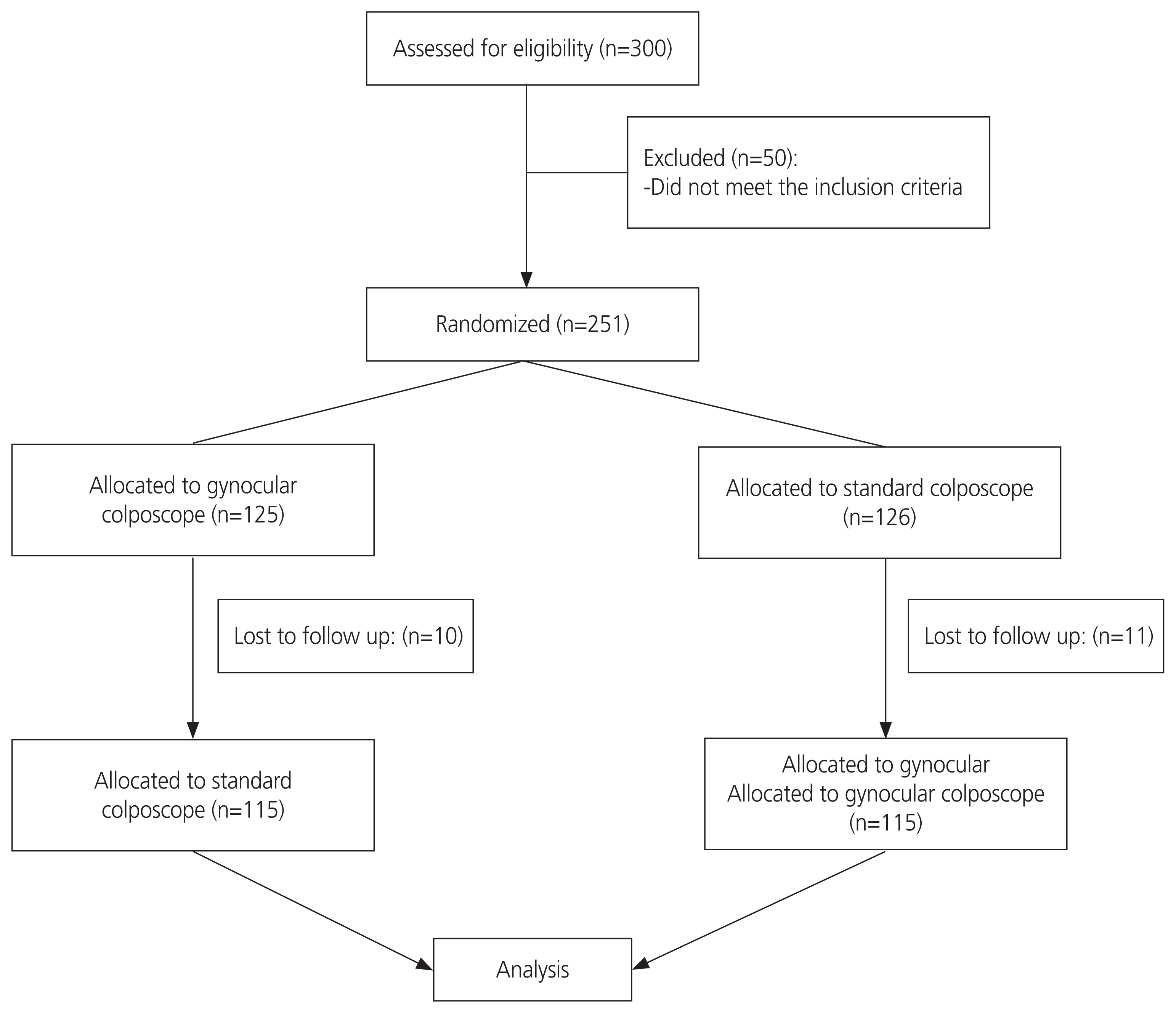
Methods
This crossover randomized clinical trial was conducted in Pondicherry, India, and included 230 women who were referred for colposcopy. Swede scores were calculated using both colposcopes, and a cervical biopsy was performed from the most visually abnormal areas. Swede scores were compared with the histopathological diagnosis, which was used as the reference standard. The level of agreement between the two colposcopes was calculated using Kappa (κ) statistics.
Results
The level of agreement of Swede scores between the standard and Gynocular colposcopes was 62.56%, and the κ statistic was 0.43 (P<0.001). Cervical intraepithelial neoplasia (CIN) 2+ (CIN 2, CIN 3, CIN 3+) was diagnosed in 40 (17.4%) women. There were no significant differences between the two colposcopes in terms of sensitivity, specificity, or predictive value for detecting CIN 2+ lesions.
Conclusion
The diagnostic accuracy of Gynocular colposcopy was similar to that of standard colposcopy for detecting CIN 2+ lesions. Gynocular colposcopes showed a good level of agreement with standard colposcopes when the Swede score was used.
Figure
Reference
-
References
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021; 71:209–49.
Article2. Ghalavandi S, Heidarnia A, Zarei F, Beiranvand R. Knowledge, attitude, practice, and self-efficacy of women regarding cervical cancer screening. Obstet Gynecol Sci. 2021; 64:216–25.
Article3. World Health Organization. Global strategy to accelerate the elimination of cervical cancer as a public health problem [Internet]. Geneva: World Health Organization;c2020. [cited 2020 Nov 17]. Available from: https://www.who.int/publications/i/item/9789240014107.4. Ngonzi J, Bajunirwe F, Wistrand C, Mayanja R, Altman D, Thorsell M, et al. Agreement of colposcope and gynocular in assessment of cervical lesions by swede score: a randomized, crossover pilot trial. J Low Genit Tract Dis. 2013; 17:372–7.5. Basu P, Banerjee D, Mittal S, Mandal R, Ghosh I, Das P, et al. Evaluation of a compact, rechargeable, magnifying device to triage VIA and HPV positive women in a cervical cancer screening program in rural India. Cancer Causes Control. 2016; 27:1253–9.
Article6. Newman H, Hu J, Li X, He J, Bradford L, Shan S, et al. Evaluation of portable colposcopy and human papillomavirus testing for screening of cervical cancer in rural China. Int J Gynecol Cancer. 2019; 29:23–7.
Article7. Nessa A, Wistrand C, Begum SA, Thuresson M, Shemer I, Thorsell M, et al. Evaluation of stationary colposcope and the gynocular, by the Swede score systematic colposcopic system in VIA positive women: a crossover randomized trial. Int J Gynecol Cancer. 2014; 24:339–45.
Article8. Kallner HK, Persson M, Thuresson M, Altman D, Shemer I, Thorsell M, et al. Diagnostic colposcopic accuracy by the gynocular and a stationary colposcope. Int J Technol Assess Health Care. 2015; 31:181–7.
Article9. Taghavi K, Rohner E, Basu P, Low N, Rutjes A, Bohlius J. Screening test accuracy of portable devices that can be used to perform colposcopy for detecting CIN2+ in low- and middle-income countries: a systematic review and meta-analysis. BMC Womens Health. 2020; 20:253.
Article10. Lam CT, Mueller J, Asma B, Asiedu M, Krieger MS, Chitalia R, et al. An integrated strategy for improving contrast, durability, and portability of a pocket colposcope for cervical cancer screening and diagnosis. PLoS One. 2018; 13:e0192530.
Article11. Sato M, Shintani D, Hanaoka M, Sato S, Miwa M, Ogasawara A, et al. A pilot study of mobile digital colposcopy in Japanese patients with cervical intraepithelial neoplasm. Mol Clin Oncol. 2021; 15:207.
Article12. Singh V, Parashari A, Gupta S, Sodhani P, Sehgal A. Performance of a low cost magnifying device, magnivisualizer, versus colposcope for detection of pre-cancer and cancerous lesions of uterine cervix. J Gynecol Oncol. 2014; 25:282–6.
Article13. Nessa A, Roy JS, Chowdhury MA, Khanam Q, Afroz R, Wistrand C, et al. Evaluation of the accuracy in detecting cervical lesions by nurses versus doctors using a stationary colposcope and gynocular in a low-resource setting. BMJ Open. 2014; 4:e005313.
Article14. Phoblap T, Temtanakitpaisan A, Aue-Angkul A, Kleebkaow P, Chumworathayi B, Luanratanakorn S, et al. Predictive value of ‘smartscopy’ for the detection of preinvasive cervical lesions during the COVID-19 pandemic: a diagnostic study. Obstet Gynecol Sci. 2022; 65:451–8.
Article15. Kanjak J, Likitdee N, Kietpeerakool C, Temtanakitpaisan A. Evaluation of mobile health applications for cervical cancer in the digital marketplace. Obstet Gynecol Sci. 2022; 65:244–55.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Performance of a low cost magnifying device, magnivisualizer, versus colposcope for detection of pre-cancer and cancerous lesions of uterine cervix
- Modified Cervicography and Visual Inspection With Acetic Acid as an Alternative Screening Method for Cervical Precancerous Lesions
- New Cervicography in the Diagnosis of Cervical Cancer
- Visual inspection with acetic acid for detection of high grade lesion in atypical squamous cells and low grade squamous intraepithelial lesions from cervical Pap smear
- Analysis of Factors Affecting Women of Childbearing Age to Screen Using Visual Inspection with Acetic Acid