Obstet Gynecol Sci.
2023 Jul;66(4):270-289. 10.5468/ogs.22323.
The coronavirus disease 2019 infection in pregnancy and adverse pregnancy outcomes: a systematic review and meta-analysis
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2544383
- DOI: http://doi.org/10.5468/ogs.22323
Abstract
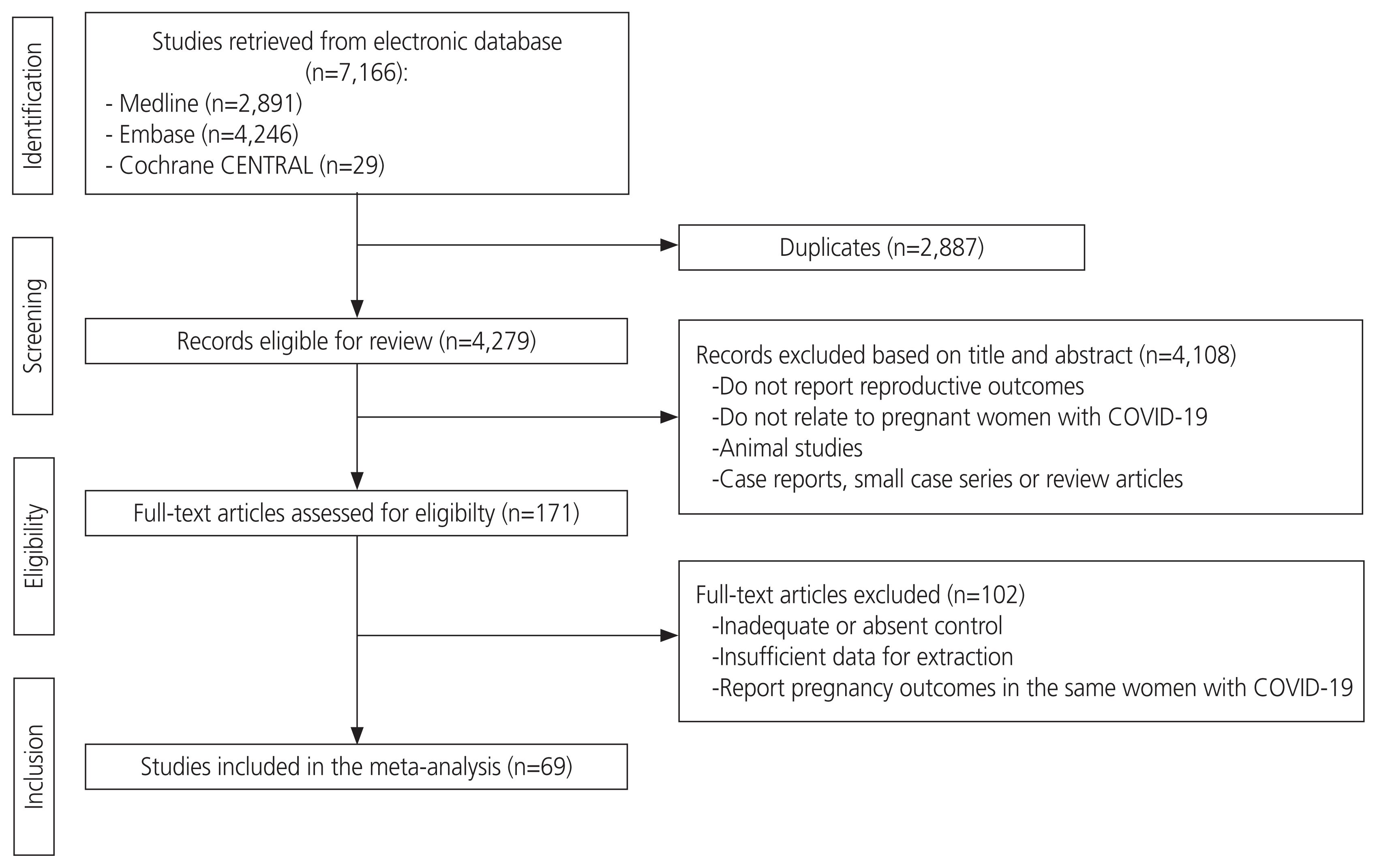
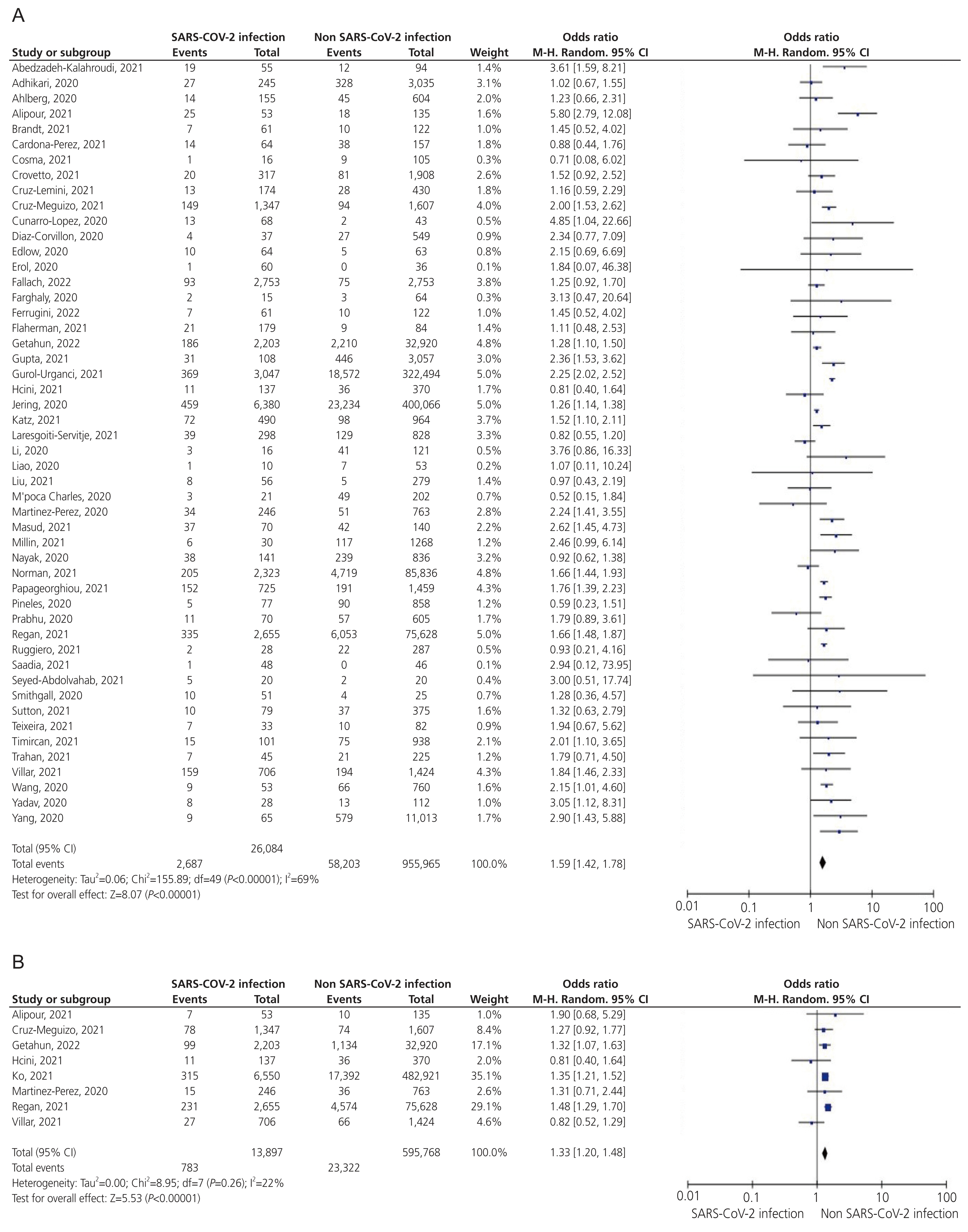
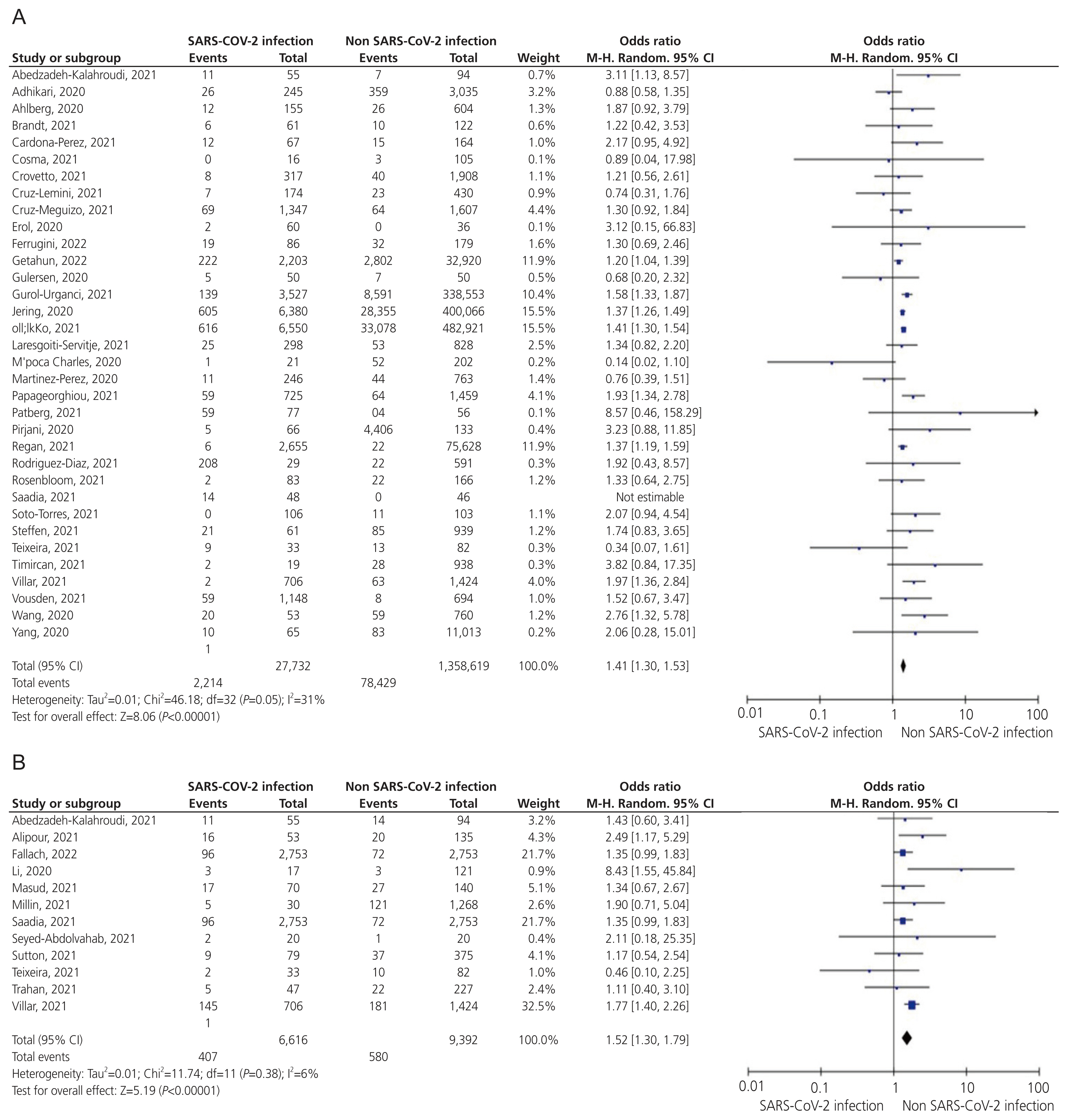
- The coronavirus disease 2019 (COVID-19) outbreak which started in December 2019 rapidly developed into a global health concern. Pregnant women are susceptible to respiratory infections and can experience adverse outcomes. This systematic review and meta-analysis compared pregnancy outcomes according to COVID-19 disease status. The MEDLINE, EMBASE, and Cochrane Library databases were searched for relevant articles published between December 1, 2019, and October 19, 2022. Main inclusion criterion was any population-based, cross-sectional, cohort, or case-control study that assessed pregnancy outcomes in women with or without laboratory-confirmed COVID-19. Sixty-nine studies including 1,606,543 pregnant women (39,716 [2.4%] diagnosed with COVID-19) were retrieved. COVID-19-infected pregnant women had a higher risk of preterm birth (odds ratio [OR], 1.59; 95% confidence interval [CI], 1.42-1.78), preeclampsia (OR, 1.41; 95% CI, 1.30-1.53), low birth weight (OR, 1.52; 95% CI, 1.30-1.79), cesarean delivery (OR, 1.20; 95% CI, 1.10-1.30), stillbirth (OR, 1.71; 95% CI, 1.39-2.10), fetal distress (OR, 2.49; 95% CI, 1.54-4.03), neonatal intensive care unit admission (OR, 2.33; 95% CI, 1.72-3.16), perinatal mortality (OR, 1.96; 95% CI, 1.15-3.34), and maternal mortality (OR, 6.15; 95% CI, 3.74-10.10). There were no significant differences in total miscarriage, preterm premature rupture of membranes, postpartum hemorrhage, cholestasis, or chorioamnionitis according to infection. This review demonstrates that COVID-19 infection during pregnancy can lead to adverse pregnancy outcomes. This information could aid researchers and clinicians in preparing for another pandemic caused by newly discovered respiratory viruses. The findings of this study may assist with evidence-based counseling and help clinicians manage pregnant women with COVID-19.
Keyword
Figure
Reference
-
References
1. Khoury R, Bernstein PS, Debolt C, Stone J, Sutton DM, Simpson LL, et al. Characteristics and outcomes of 241 births to women with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection at five New York City medical centers. Obstet Gynecol. 2020; 136:273–82.
Article2. Allotey J, Stallings E, Bonet M, Yap M, Chatterjee S, Kew T, et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ. 2020; 370:m3320.
Article3. Adhikari EH, Moreno W, Zofkie AC, MacDonald L, McIntire DD, Collins RRJ, et al. Pregnancy outcomes among women with and without severe acute respiratory syndrome coronavirus 2 infection. JAMA Netw Open. 2020; 3:e2029256.
Article4. Melo GC, Araújo KCGM. COVID-19 infection in pregnant women, preterm delivery, birth weight, and vertical transmission: a systematic review and meta-analysis. Cad Saude Publica. 2020; 36:e00087320.
Article5. Shephard HM, Manning SE, Nestoridi E, Brown C, Yazdy MM. Characteristics of people with and without laboratory-confirmed SARS-CoV-2 infection during pregnancy, massachusetts, March 2020–March 2021. Public Health Rep. 2022; 137:782–9.
Article6. Vera von Bargen H, Espinosa Serrano M, Martin Navarrete D, Ahumada Droguett P, Méndez Benavente C, Flores Castillo M, et al. Analysis of prevalence and sociodemographic conditions among women in labor with and without COVID-19 in public hospitals in Chile. J Perinat Med. 2021; 50:132–8.
Article7. Griffin I, Benarba F, Peters C, Oyelese Y, Murphy T, Contreras D, et al. The impact of COVID-19 infection on labor and delivery, newborn nursery, and neonatal intensive care unit: prospective observational data from a single hospital system. Am J Perinatol. 2020; 37:1022–30.
Article8. Wei L, Gao X, Chen S, Zeng W, Wu J, Lin X, et al. Clinical characteristics and outcomes of childbearing-age women with COVID-19 in Wuhan: retrospective, single-center study. J Med Internet Res. 2020; 22:e19642.
Article9. Martinez-Perez O, Prats Rodriguez P, Muner Hernandez M, Encinas Pardilla MB, Perez Perez N, Vila Hernandez MR, et al. The association between SARS-CoV-2 infection and preterm delivery: a prospective study with a multivariable analysis. BMC Pregnancy Childbirth. 2021; 21:273.
Article10. Dhuyvetter A, Cejtin HE, Adam M, Patel A. Coronavirus disease 2019 in pregnancy: the experience at an urban safety net hospital. J Community Health. 2021; 46:267–9.
Article11. Yang H, Wang C, Poon LC. Novel coronavirus infection and pregnancy. Ultrasound Obstet Gynecol. 2020; 55:435–7.
Article12. Charles CM, Osman NB, Arijama D, Matingane B, Sitoé T, Kenga D, et al. Clinical and epidemiological aspects of SARS-CoV-2 infection among pregnant and postpartum women in Mozambique: a prospective cohort study. Reprod Health. 2022; 19:164.
Article13. Nayak AH, Kapote DS, Fonseca M, Chavan N, Mayekar R, Sarmalkar M, et al. Impact of the coronavirus infection in pregnancy: a preliminary study of 141 patients. J Obstet Gynaecol India. 2020; 70:256–61.
Article14. Taghavi SA, Heidari S, Jahanfar S, Amirjani S, Aji-ramkani A, Azizi-Kutenaee M, et al. Obstetric, maternal, and neonatal outcomes in COVID-19 compared to healthy pregnant women in Iran: a retrospective, case-control study. Middle East Fertil Soc J. 2021; 26:17.
Article15. Milln J, Heard S, Gunganah K, Velauthar L, Saeed F. Clinical characteristics and pregnancy outcomes of women diagnosed with SARS-CoV-2 in London’s most ethnically diverse borough: a cross-sectional study. Obstet Med. 2021; 14:164–9.
Article16. Pasternak B, Neovius M, Söderling J, Ahlberg M, Norman M, Ludvigsson JF, et al. Preterm birth and stillbirth during the COVID-19 pandemic in Sweden: a nationwide cohort study. Ann Intern Med. 2021; 174:873–5.
Article17. Prabhu M, Cagino K, Matthews KC, Friedlander RL, Glynn SM, Kubiak JM, et al. Pregnancy and postpartum outcomes in a universally tested population for SARS-CoV-2 in New York City: a prospective cohort study. BJOG. 2020; 127:1548–56.
Article18. Li N, Han L, Peng M, Lv Y, Ouyang Y, Liu K, et al. Maternal and neonatal outcomes of pregnant women with coronavirus disease 2019 (COVID-19) pneumonia: a case-control study. Clin Infect Dis. 2020; 71:2035–41.
Article19. Flaherman VJ, Afshar Y, Boscardin WJ, Keller RL, Mardy AH, Prahl MK, et al. Infant outcomes following maternal infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): first report from the pregnancy coronavirus outcomes registry (PRIORITY) study. Clin Infect Dis. 2021; 73:e2810–3.
Article20. Crovetto F, Crispi F, Llurba E, Pascal R, Larroya M, Trilla C, et al. Impact of severe acute respiratory syndrome coronavirus 2 infection on pregnancy outcomes: a population-based study. Clin Infect Dis. 2021; 73:1768–75.
Article21. Edlow AG, Li JZ, Collier AY, Atyeo C, James KE, Boatin AA, et al. Assessment of maternal and neonatal SARS-CoV-2 viral load, transplacental antibody transfer, and placental pathology in pregnancies during the COVID-19 pandemic. JAMA Netw Open. 2020; 3:e2030455.
Article22. Rodríguez-Díaz M, Alonso-Molero J, Cabero-Perez MJ, Llorca J, Dierssen-Sotos T, Gómez-Acebo I, et al. Pregnancy and birth outcomes during the early months of the COVID-19 pandemic: the MOACC-19 cohort. Int J Environ Res Public Health. 2021; 18:10931.
Article23. Jering KS, Claggett BL, Cunningham JW, Rosenthal N, Vardeny O, Greene MF, et al. Clinical characteristics and outcomes of hospitalized women giving birth with and without COVID-19. JAMA Intern Med. 2021; 181:714–7.
Article24. Regan AK, Arah OA, Fell DB, Sullivan SG. SARS-CoV-2 infection during pregnancy and associated perinatal health outcomes: a national US cohort study. J Infect Dis. 2022; 225:759–67.
Article25. Sahin D, Tanacan A, Erol SA, Anuk AT, Eyi EGY, Ozgu-Erdinc AS, et al. A pandemic center’s experience of managing pregnant women with COVID-19 infection in Turkey: a prospective cohort study. Int J Gynaecol Obstet. 2020; 151:74–82.
Article26. Ferrugini CLP, Boldrini NAT, Costa FLS, Salgueiro MAOB, Coelho PDP, Miranda AE. SARS-CoV-2 infection in pregnant women assisted in a high-risk maternity hospital in Brazil: clinical aspects and obstetric outcomes. PLoS One. 2022; 17:e0264901.
Article27. Binte Masud S, Zebeen F, Alam DW, Hossian M, Zaman S, Begum RA, et al. Adverse birth outcomes among pregnant women with and without COVID-19: a comparative study from bangladesh. J Prev Med Public Health. 2021; 54:422–30.
Article28. Brandt JS, Fell DB. SARS-CoV-2 infection in pregnancy: lessons learned from the first pandemic wave. Paediatr Perinat Epidemiol. 2021; 35:34–6.
Article29. Hcini N, Maamri F, Picone O, Carod JF, Lambert V, Mathieu M, et al. Maternal, fetal and neonatal outcomes of large series of SARS-CoV-2 positive pregnancies in peripartum period: a single-center prospective comparative study. Eur J Obstet Gynecol Reprod Biol. 2021; 257:11–8.
Article30. Patberg ET, Adams T, Rekawek P, Vahanian SA, Akerman M, Hernandez A, et al. Coronavirus disease 2019 infection and placental histopathology in women delivering at term. Am J Obstet Gynecol. 2021; 224:382.e1–382.e18.
Article31. Sakowicz A, Ayala AE, Ukeje CC, Witting CS, Grobman WA, Miller ES. Risk factors for severe acute respiratory syndrome coronavirus 2 infection in pregnant women. Am J Obstet Gynecol MFM. 2020; 2:100198.
Article32. Pineles BL, Goodman KE, Pineles L, O’Hara LM, Nadimpalli G, Magder LS, et al. In-hospital mortality in a cohort of hospitalized pregnant and nonpregnant patients with COVID-19. Ann Intern Med. 2021; 174:1186–8.
Article33. Saadia Z, Farrukh R, Kanwal S, Shahzad Q. Clinical profiles, demographic features, and maternal outcomes among coronavirus disease positive pregnant women: a cross-sectional study. Open Access Maced J Med Sci. 2021; 9:486–91.
Article34. Díaz-Corvillón P, Mönckeberg M, Barros A, Illanes SE, Soldati A, Nien JK, et al. Routine screening for SARS CoV-2 in unselected pregnant women at delivery. PLoS One. 2020; 15:e0239887.
Article35. Fallach N, Segal Y, Agassy J, Perez G, Peretz A, Chodick G, et al. Pregnancy outcomes after SARS-CoV-2 infection by trimester: a large, population-based cohort study. PLoS One. 2022; 17:e0270893.
Article36. Sutton D, Wen T, Staniczenko AP, Huang Y, Andrikopoulou M, D’Alton M, et al. Clinical and demographic risk factors for COVID-19 during delivery hospitalizations in New York City. Am J Perinatol. 2021; 38:857–68.
Article37. Getahun D, Peltier MR, Lurvey LD, Shi JM, Braun D, Sacks DA, et al. Association between SARS-CoV-2 infection and adverse perinatal outcomes in a large health maintenance organization. Am J Perinatol. 2022; Jun. 23. [Epub]. https://doi.org/10.1055/s-0042-1749666.
Article38. Cruz-Lemini M, Ferriols Perez E, de la Cruz Conty ML, Caño Aguilar A, Encinas Pardilla MB, Prats Rodríguez P, et al. Obstetric outcomes of SARS-CoV-2 infection in asymptomatic pregnant women. Viruses. 2021; 13:112.
Article39. Cruz Melguizo S, de la Cruz Conty ML, Carmona Payán P, Abascal-Saiz A, Pintando Recarte P, González Rodríguez L, et al. Pregnancy outcomes and SARS-CoV-2 infection: the Spanish Obstetric Emergency Group study. Viruses. 2021; 13:853.
Article40. Teixeira MLB, Costa Ferreira Júnior OD, João E, Fuller T, Silva Esteves J, Mendes-Silva W, et al. Maternal and neonatal outcomes of SARS-CoV-2 infection in a cohort of pregnant women with comorbid disorders. Viruses. 2021; 13:1277.
Article41. Wang MJ, Schapero M, Iverson R, Yarrington CD. Obstetric hemorrhage risk associated with novel COVID-19 diagnosis from a single-institution cohort in the United States. Am J Perinatol. 2020; 37:1411–6.
Article42. Abedzadeh-Kalahroudi M, Karimian Z, Nasiri S, Khorshidifard MS. Anxiety and perceived stress of pregnant women towards covid-19 disease and its related factors in Kashan (2020). Iran J Obstet Gynecol Infertil. 2021; 24:8–18.43. Alipour Z, Samadi P, Eskandari N, Ghaedrahmati M, Vahedian M, Khalajinia Z, et al. Relationship between coronavirus disease 2019 in pregnancy and maternal and fetal outcomes: retrospective analytical cohort study. Midwifery. 2021; 102:103128.
Article44. Li WK, Chen XJC, Altshuler D, Islam S, Spiegler P, Emerson L, et al. The incidence of propofol infusion syndrome in critically-ill patients. J Crit Care. 2022; 71:154098.
Article45. Cardona-Pérez JA, Villegas-Mota I, Helguera-Repetto AC, Acevedo-Gallegos S, Rodríguez-Bosch M, Aguinaga-Ríos M, et al. Prevalence, clinical features, and outcomes of SARS-CoV-2 infection in pregnant women with or without mild/moderate symptoms: results from universal screening in a tertiary care center in Mexico City, Mexico. PLoS One. 2021; 16:e0249584.
Article46. Chornock R, Iqbal SN, Wang T, Kodama S, Kawakita T, Fries M. Incidence of hypertensive disorders of pregnancy in women with COVID-19. Am J Perinatol. 2021; 38:766–72.
Article47. Cosma S, Carosso AR, Borella F, Cusato J, Bovetti M, Bevilacqua F, et al. Prenatal biochemical and ultrasound markers in covid-19 pregnant patients: a prospective case-control study. Diagnostics (Basel). 2021; 11:398.
Article48. Cuñarro-López Y, Cano-Valderrama Ó, Pintado-Recarte P, Cueto-Hernández I, González-Garzón B, García-Tizón S, et al. Maternal and perinatal outcomes in patients with suspected COVID-19 and their relationship with a negative RT-PCR result. J Clin Med. 2020; 9:3552.
Article49. Farghaly MAA, Kupferman F, Castillo F, Kim RM. Characteristics of newborns born to SARS-CoV-2-positive mothers: a retrospective cohort study. Am J Perinatol. 2020; 37:1310–6.
Article50. Gulersen M, Blitz MJ, Rochelson B, Nimaroff M, Shan W, Bornstein E. Clinical implications of SARS-CoV-2 infection in the viable preterm period. Am J Perinatol. 2020; 37:1077–83.
Article51. Gupta P, Khatana VP, Prabha R, Jha I, Singh M, Pandey AK, et al. An observational study for appraisal of clinical outcome and risk of mother-to-child SARS-CoV-2 transmission in neonates provided the benefits of mothers’ own milk. Eur J Pediatr. 2022; 181:513–27.
Article52. Gurol-Urganci I, Waite L, Webster K, Jardine J, Carroll F, Dunn G, et al. Obstetric interventions and pregnancy outcomes during the COVID-19 pandemic in England: a nationwide cohort study. PLoS Med. 2022; 19:e1003884.
Article53. Smithgall MC, Liu-Jarin X, Hamele-Bena D, Cimic A, Mourad M, Debelenko L, et al. Third-trimester placentas of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)-positive women: histomorphology, including viral immunohistochemistry and in-situ hybridization. Histopathology. 2020; 77:994–9.
Article54. Katz D, Bateman BT, Kjaer K, Turner DP, Spence NZ, Habib AS, et al. The society for obstetric anesthesia and perinatology coronavirus disease 2019 registry: an analysis of outcomes among pregnant women delivering during the initial severe acute respiratory syndrome coronavirus-2 outbreak in the United States. Anesth Analg. 2021; 133:462–73.
Article55. Ko JY, DeSisto CL, Simeone RM, Ellington S, Galang RR, Oduyebo T, et al. Adverse pregnancy outcomes, maternal complications, and severe illness among US delivery hospitalizations with and without a coronavirus disease 2019 (COVID-19) diagnosis. Clin Infect Dis. 2021; 73:S24–31.
Article56. Laresgoiti-Servitje E, Cardona-Pérez JA, Hernández-Cruz RG, Helguera-Repetto AC, Valdespino-Vázquez MY, Moreno-Verduzco ER, et al. COVID-19 infection in pregnancy: PCR cycle thresholds, placental pathology, and perinatal outcomes. Viruses. 2021; 13:1884.
Article57. Liao X, Yang H, Kong J, Yang H. Chest CT findings in a pregnant patient with 2019 novel coronavirus disease. Balkan Med J. 2020; 37:226–8.
Article58. Liu S, Dzakpasu S, Nelson C, Wei SQ, Little J, Scott H, et al. Pregnancy outcomes during the COVID-19 pandemic in Canada, March to August 2020. J Obstet Gynaecol Can. 2021; 43:1406–15.
Article59. Papageorghiou AT, Gunier RB, Villar J. The link between COVID-19 and preeclampsia. Am J Obstet Gynecol. 2022; 226:153–4.
Article60. Pirjani R, Rabiei M, Abiri A, Moini A. An overview on guidelines on COVID-19 virus and natural and assisted reproductive techniques pregnancies. Int J Fertil Steril. 2020; 14:264–71.61. Ríos-Silva M, Murillo-Zamora E, Mendoza-Cano O, Trujillo X, Huerta M. COVID-19 mortality among pregnant women in Mexico: a retrospective cohort study. J Glob Health. 2020; 10:020512.
Article62. Rosenbloom JI, Raghuraman N, Carter EB, Kelly JC. Coronavirus disease 2019 infection and hypertensive disorders of pregnancy. Am J Obstet Gynecol. 2021; 224:623–4.
Article63. Ruggiero M, Somigliana E, Tassis B, Li Piani L, Uceda Renteria S, Barbara G, et al. Clinical relevance of SARS-CoV-2 infection in late pregnancy. BMC Pregnancy Childbirth. 2021; 21:505.
Article64. Savirón-Cornudella R, Villalba A, Esteban LM, Tajada M, Rodríguez-Solanilla B, Andeyro-Garcia M, et al. Screening of severe acute respiratory syndrome coronavirus-2 infection during labor and delivery using polymerase chain reaction and immunoglobulin testing. Life Sci. 2021; 271:119200.
Article65. Soto-Torres E, Hernandez-Andrade E, Huntley E, Mendez-Figueroa H, Blackwell SC. Ultrasound and Doppler findings in pregnant women with SARS-CoV-2 infection. Ultrasound Obstet Gynecol. 2021; 58:111–20.66. Steffen HA, Swartz SR, Jackson JB, Kenne KA, Ten Eyck PP, Merryman AS, et al. SARS-CoV-2 infection during pregnancy in a rural midwest all-delivery cohort and associated maternal and neonatal outcomes. Am J Perinatol. 2021; 38:614–21.
Article67. Timircan M, Bratosin F, Vidican I, Suciu O, Tirnea L, Avram V, et al. Exploring pregnancy outcomes associated with SARS-CoV-2 infection. Medicina (Kaunas). 2021; 57:796.
Article68. Trahan MJ, O’Farrell P, Mitric C, Desilets J, Bastrash MP, Malhame I, et al. 364 obstetrical and neonatal outcomes among pregnancies with SARS-CoV-2. Am J Obstet Gynecol. 2021; 224:S237.
Article69. Roffman J, Villarreal J, Pride R, Bazer O, Karmacharya R, Lerou P, et al. Assessing covid-19 effects on neurodevelopment (ACEND): preliminary findings in 12-month-old children exposed to maternal sars-cov-2 infection during pregnancy. Neuropsychopharmacology. 2021; 46:150–1.70. Vousden N, Bunch K, Morris E, Simpson N, Gale C, O’Brien P, et al. The incidence, characteristics and outcomes of pregnant women hospitalized with symptomatic and asymptomatic SARS-CoV-2 infection in the UK from March to September 2020: a national cohort study using the UK obstetric surveillance system (UKOSS). PLoS One. 2021; 16:e0251123.
Article71. Kathuria P, Khetarpal A, Singh P, Khatana S, Yadav G, Ghuman NK. Role of birth companion in COVID-19: indispensable for her and an auxiliary hand for us. Pan Afr Med J. 2020; 37:62.
Article72. Ahn KH, Kim HI, Lee KS, Heo JS, Kim HY, Cho GJ, et al. COVID-19 and vaccination during pregnancy: a systematic analysis using Korea National Health Insurance claims data. Obstet Gynecol Sci. 2022; 65:487–501.
Article73. Lassi ZS, Ana A, Das JK, Salam RA, Padhani ZA, Irfan O, et al. A systematic review and meta-analysis of data on pregnant women with confirmed COVID-19: clinical presentation, and pregnancy and perinatal outcomes based on COVID-19 severity. J Glob Health. 2021; 11:05018.
Article74. Pathirathna ML, Samarasekara BPP, Dasanayake TS, Saravanakumar P, Weerasekara I. Adverse perinatal outcomes in COVID-19 infected pregnant women: a systematic review and meta-analysis. Healthcare (Basel). 2022; 10:203.
Article75. Huntley BJF, Mulder IA, Di Mascio D, Vintzileos WS, Vintzileos AM, Berghella V, et al. Adverse pregnancy outcomes among individuals with and without severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): a systematic review and meta-analysis. Obstet Gynecol. 2021; 137:585–96.76. Wei WH, Mellis S, Geba GP, Sivapalasingam S, Jalbert JJ. Incidence and risk factors for COVID-related urgent medical visits among US patients diagnosed with COVID-19 in the outpatient setting. Pharmacoepidemiol Drug Saf. 2021; 30:22–3.77. Wei SQ, Bilodeau-Bertrand M, Liu S, Auger N. The impact of COVID-19 on pregnancy outcomes: a systematic review and meta-analysis. CMAJ. 2021; 193:E540–8.
Article78. Bastos SNMAN, Barbosa BLF, Cruz LGB, Souza RP, Silva Melo SSE, Luz CCBDS. Clinical and obstetric aspects of pregnant women with COVID-19: a systematic review. Rev Bras Ginecol Obstet. 2021; 43:949–60.
Article79. Jafari M, Pormohammad A, Sheikh Neshin SA, Ghorbani S, Bose D, Alimohammadi S, et al. Clinical characteristics and outcomes of pregnant women with COVID-19 and comparison with control patients: a systematic review and meta-analysis. Rev Med Virol. 2021; 31:1–16.80. Chen S, Huang B, Luo DJ, Li X, Yang F, Zhao Y, et al. Pregnancy with new coronavirus infection: clinical characteristics and placental pathological analysis of three cases. Zhonghua Bing Li Xue Za Zhi. 2020; 49:418–23.81. Pérez-López FR, Savirón-Cornudella R, Chedraui P, López-Baena MT, Pérez-Roncero G, Sanz-Arenal A, et al. Obstetric and perinatal outcomes of pregnancies with COVID 19: a systematic review and meta-analysis. J Matern Fetal Neonatal Med. 2022; 35:9742–58.82. Wang H, Li N, Sun C, Guo X, Su W, Song Q, et al. The association between pregnancy and COVID-19: a systematic review and meta-analysis. Am J Emerg Med. 2022; 56:188–95.83. Conde-Agudelo A, Romero R. SARS-CoV-2 infection during pregnancy and risk of preeclampsia: a systematic review and meta-analysis. Am J Obstet Gynecol. 2022; 226:68–89.e3.84. Garrido-Pontnou M, Navarro A, Camacho J, Crispi F, Alguacil-Guillén M, Moreno-Baró A, et al. Diffuse trophoblast damage is the hallmark of SARS-CoV-2-associated fetal demise. Mod Pathol. 2021; 34:1704–9.85. Hecht JL, Quade B, Deshpande V, Mino-Kenudson M, Ting DT, Desai N, et al. SARS-CoV-2 can infect the placenta and is not associated with specific placental histopathology: a series of 19 placentas from COVID-19-positive mothers. Mod Pathol. 2020; 33:2092–103.
Article86. Berghella V, Boelig R, Roman A, Burd J, Anderson K. Decreased incidence of preterm birth during coronavirus disease 2019 pandemic. Am J Obstet Gynecol MFM. 2020; 2:100258.
Article87. Kourtis AP, Read JS, Jamieson DJ. Pregnancy and infection. N Engl J Med. 2014; 370:2211–8.
Article88. Wastnedge EAN, Reynolds RM, van Boeckel SR, Stock SJ, Denison FC, Maybin JA, et al. Pregnancy and COVID-19. Physiol Rev. 2021; 101:303–18.
Article89. Goodnight WH, Soper DE. Pneumonia in pregnancy. Crit Care Med. 2005; 33:S390–7.
Article90. Wong SF, Chow KM, Leung TN, Ng WF, Ng TK, Shek CC, et al. Pregnancy and perinatal outcomes of women with severe acute respiratory syndrome. Am J Obstet Gynecol. 2004; 191:292–7.
Article91. Alfaraj SH, Al-Tawfiq JA, Memish ZA. Middle east respiratory syndrome coronavirus (MERS-CoV) infection during pregnancy: report of two cases & review of the literature. J Microbiol Immunol Infect. 2019; 52:501–3.
Article92. Jamieson DJ, Theiler RN, Rasmussen SA. Emerging infections and pregnancy. Emerg Infect Dis. 2006; 12:1638–43.
Article93. Zhang L, Jiang Y, Wei M, Cheng BH, Zhou XC, Li J, et al. Analysis of the pregnancy outcomes in pregnant women with COVID-19 in Hubei province. Zhonghua Fu Chan Ke Za Zhi. 2020; 55:166–71.94. Fan C, Lei D, Fang C, Li C, Wang M, Liu Y, et al. Perinatal transmission of 2019 coronavirus disease-associated severe acute respiratory syndrome coronavirus 2: should we worry? Clin Infect Dis. 2021; 72:862–4.
Article95. Ferrazzi E, Frigerio L, Savasi V, Vergani P, Prefumo F, Barresi S, et al. Vaginal delivery in SARS-CoV-2-infected pregnant women in Northern Italy: a retrospective analysis. BJOG. 2020; 127:1116–21.
Article96. Damar Çakırca T, Torun A, Hamidanoğlu M, Portakal RD, Ölçen M, Çakırca G, et al. COVID-19 infection in pregnancy: a single center experience with 75 cases. Ginekol Pol. 2022; 93:410–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The coronavirus disease 2019 infection in pregnancy and adverse pregnancy outcomes: a systematic review and meta-analysis
- Pregnancy outcomes after all modes of conception in patients with genital tuberculosis: a systematic review and meta-analysis
- Unveiling the Outcomes of Mpox in Pregnancy: A Systematic Review and Single-Arm Meta-Analysis
- Prediction of Adverse Outcomes among Women in the Third Trimester of Pregnancy with Coronavirus Disease 2019
- Thyroid disease in pregnancy