J Korean Assoc Oral Maxillofac Surg.
2023 Jun;49(3):135-141. 10.5125/jkaoms.2023.49.3.135.
Prediction of medication-related osteonecrosis of the jaw (MRONJ) using automated machine learning in patients with osteoporosis associated with dental extraction and implantation: a retrospective study
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, College of Dentistry, Dankook University, Cheonan, Korea
- KMID: 2544315
- DOI: http://doi.org/10.5125/jkaoms.2023.49.3.135
Abstract
Objectives
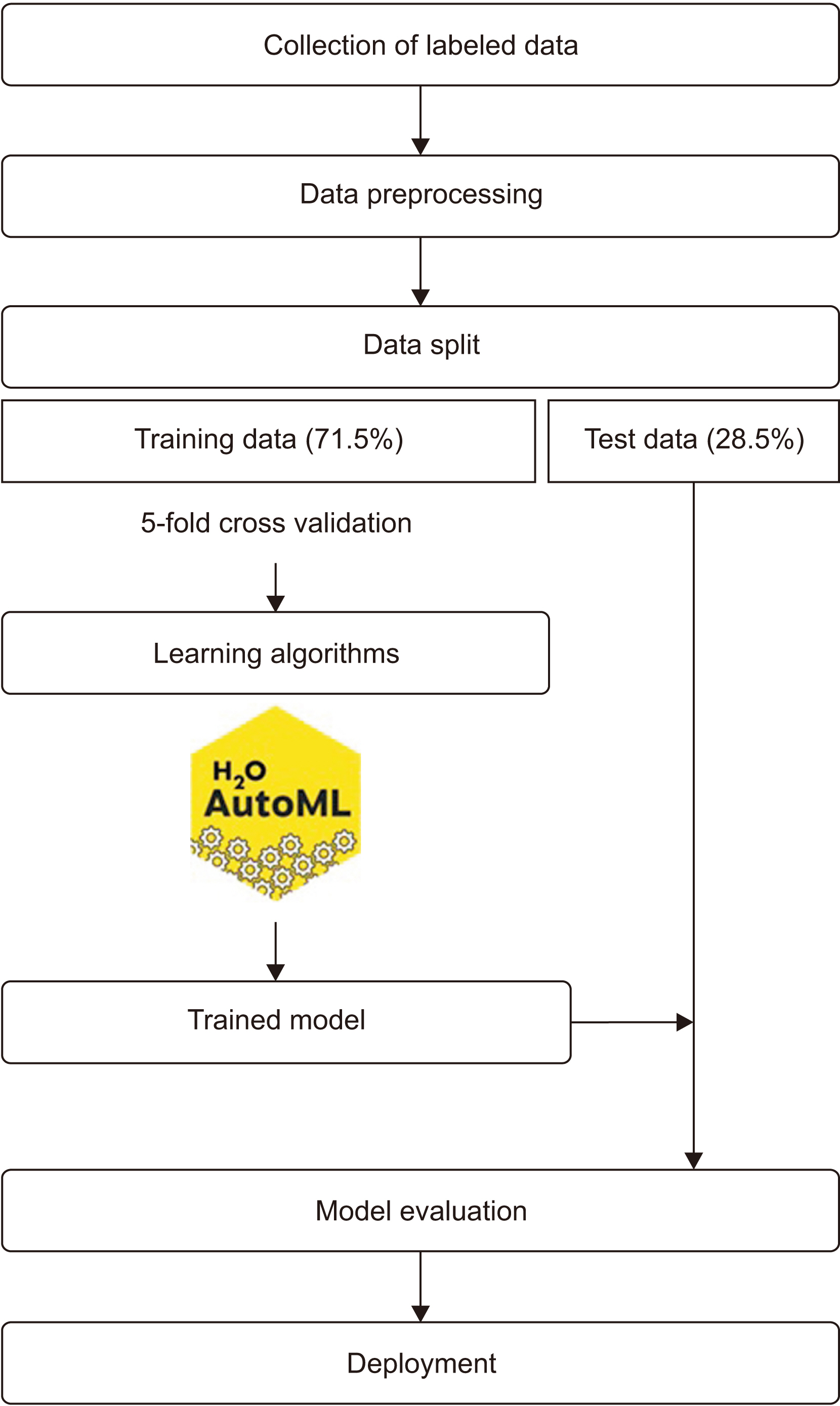
This study aimed to develop and validate machine learning (ML) models using H 2 O-AutoML, an automated ML program, for predicting medication-related osteonecrosis of the jaw (MRONJ) in patients with osteoporosis undergoing tooth extraction or implantation.
Patients and Methods
We conducted a retrospective chart review of 340 patients who visited Dankook University Dental Hospital between Janu-ary 2019 and June 2022 who met the following inclusion criteria: female, age ≥55 years, osteoporosis treated with antiresorptive therapy, and recent dental extraction or implantation. We considered medication administration and duration, demographics, and systemic factors (age and medical history). Local factors, such as surgical method, number of operated teeth, and operation area, were also included. Six algorithms were used to generate the MRONJ prediction model.
Results
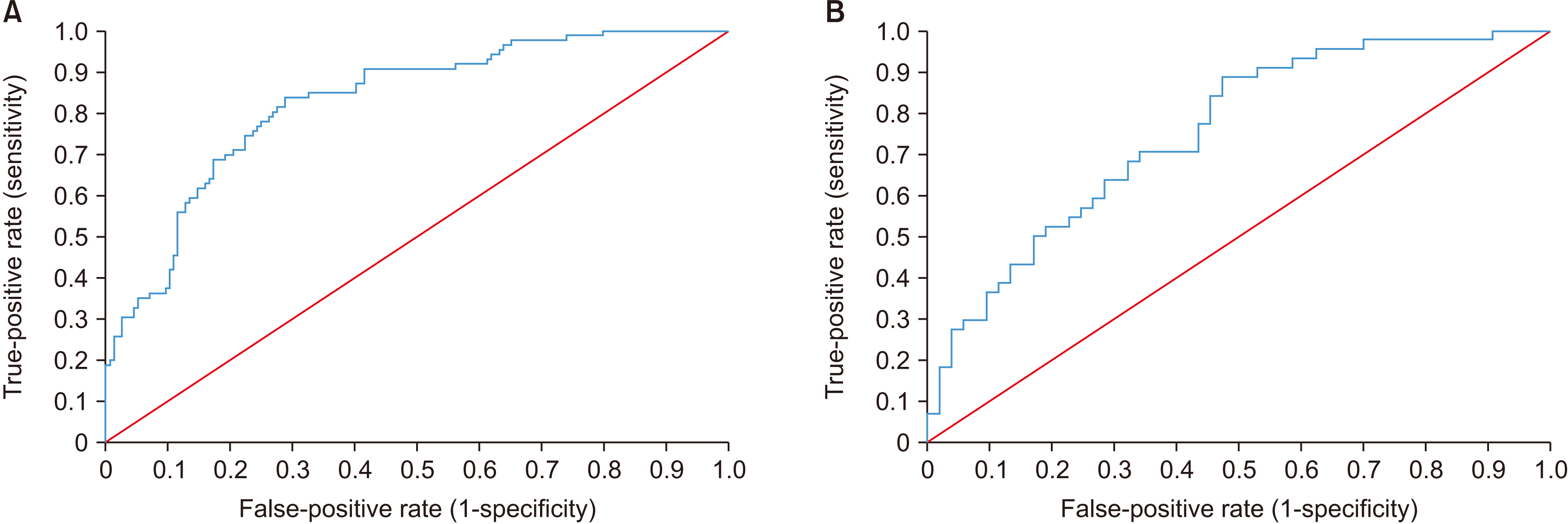
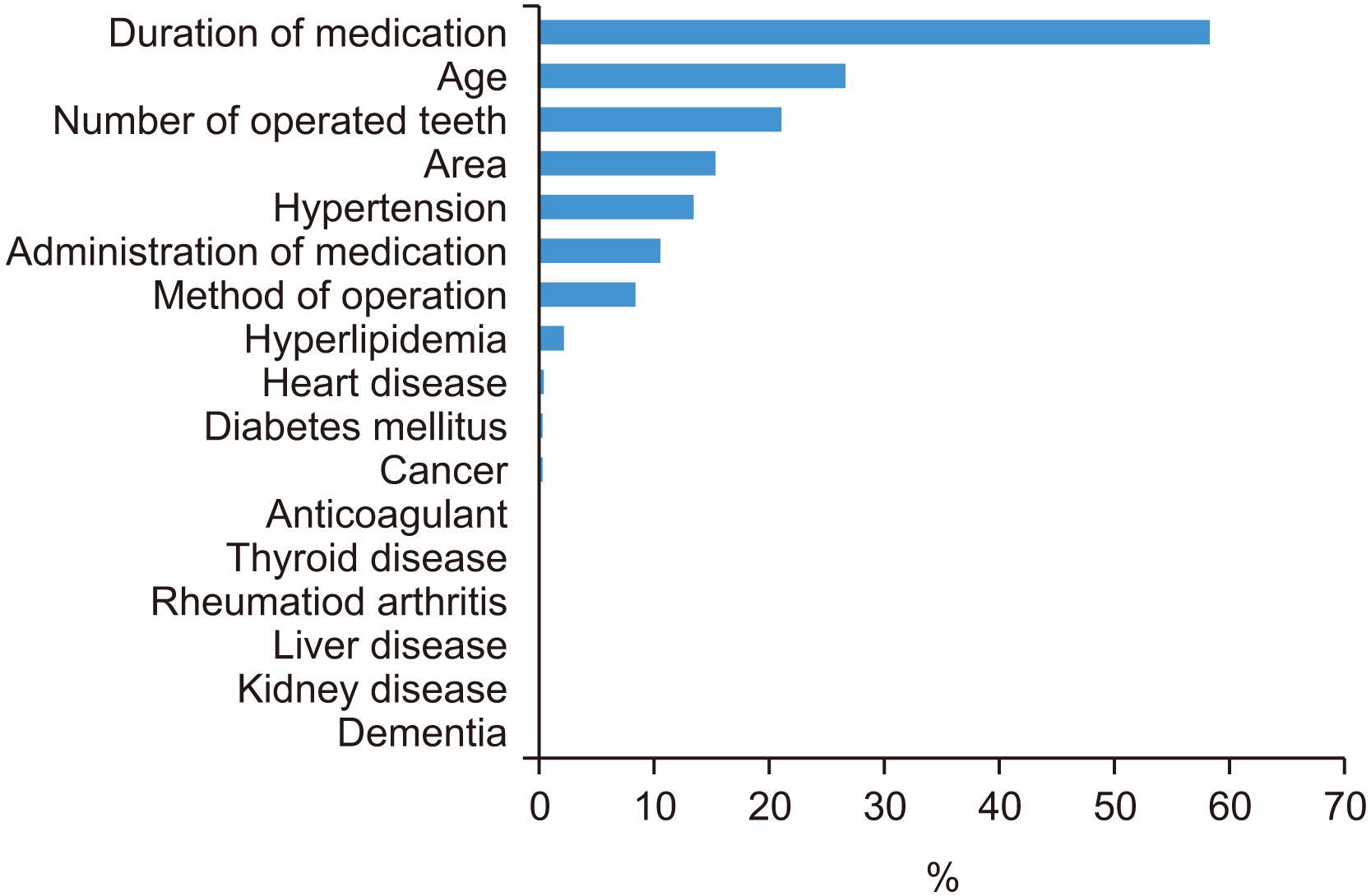
Gradient boosting demonstrated the best diagnostic accuracy, with an area under the receiver operating characteristic curve (AUC) of 0.8283. Validation with the test dataset yielded a stable AUC of 0.7526. Variable importance analysis identified duration of medication as the most important variable, followed by age, number of teeth operated, and operation site.
Conclusion
ML models can help predict MRONJ occurrence in patients with osteoporosis undergoing tooth extraction or implantation based on questionnaire data acquired at the first visit.
Keyword
Figure
Reference
-
References
1. Kim DW, Kim H, Nam W, Kim HJ, Cha IH. 2018; Machine learning to predict the occurrence of bisphosphonate-related osteonecrosis of the jaw associated with dental extraction: a preliminary report. Bone. 116:207–14. https://doi.org/10.1016/j.bone.2018.04.020. DOI: 10.1016/j.bone.2018.04.020. PMID: 29698784.
Article2. Heo J, Yoo J, Lee H, Lee IH, Kim JS, Park E, et al. 2022; Prediction of hidden coronary artery disease using machine learning in patients with acute ischemic stroke. Neurology. 99:e55–65. https://doi.org/10.1212/wnl.0000000000200576. DOI: 10.1212/WNL.0000000000200576. PMID: 35470135.
Article3. Chen YW, Stanley K, Att W. 2020; Artificial intelligence in dentistry: current applications and future perspectives. Quintessence Int. 51:248–57. https://doi.org/10.3290/j.qi.a43952. DOI: 10.3290/j.qi.a43952. PMID: 32020135.
Article4. Lee JH, Kim DH, Jeong SN, Choi SH. 2018; Detection and diagnosis of dental caries using a deep learning-based convolutional neural network algorithm. J Dent. 77:106–11. https://doi.org/10.1016/j.jdent.2018.07.015. DOI: 10.1016/j.jdent.2018.07.015. PMID: 30056118.
Article5. Jung SK, Kim TW. 2016; New approach for the diagnosis of extractions with neural network machine learning. Am J Orthod Dentofacial Orthop. 149:127–33. https://doi.org/10.1016/j.ajodo.2015.07.030. DOI: 10.1016/j.ajodo.2015.07.030. PMID: 26718386.
Article6. Ben-Israel D, Jacobs WB, Casha S, Lang S, Ryu WHA, de Lotbiniere-Bassett M, et al. 2020; The impact of machine learning on patient care: a systematic review. Artif Intell Med. 103:101785. https://doi.org/10.1016/j.artmed.2019.101785. DOI: 10.1016/j.artmed.2019.101785. PMID: 32143792.
Article7. Jordan MI, Mitchell TM. 2015; Machine learning: trends, perspectives, and prospects. Science. 349:255–60. https://doi.org/10.1126/science.aaa8415. DOI: 10.1126/science.aaa8415. PMID: 26185243.
Article8. Truong A, Walters A, Goodsitt J, Hines K, Bruss CB, Farivar R. 2019; Towards automated machine learning: evaluation and comparison of AutoML approaches and tools. 2019 IEEE 31st International Conference on Tools with Artificial Intelligence (ICTAI). 1471–9. https://doi.org/10.1109/ICTAI.2019.00209. DOI: 10.1109/ICTAI.2019.00209.
Article9. Ruggiero SL, Dodson TB, Aghaloo T, Carlson ER, Ward BB, Kademani D. 2022; American Association of Oral and Maxillofacial Surgeons' position paper on medication-related osteonecrosis of the jaws-2022 update. J Oral Maxillofac Surg. 80:920–43. https://doi.org/10.1016/j.joms.2022.02.008. DOI: 10.1016/j.joms.2022.02.008. PMID: 35300956.
Article10. Yamagata K, Nagai H, Baba O, Uchida F, Kanno N, Hasegawa S, et al. 2016; A case of brain abscess caused by medication-related osteonecrosis of the jaw. Case Rep Dent. 2016:7038618. https://doi.org/10.1155/2016/7038618. DOI: 10.1155/2016/7038618. PMID: 26949551. PMCID: PMC4754463.
Article11. Uddin S, Khan A, Hossain ME, Moni MA. 2019; Comparing different supervised machine learning algorithms for disease prediction. BMC Med Inform Decis Mak. 19:281. https://doi.org/10.1186/s12911-019-1004-8. DOI: 10.1186/s12911-019-1004-8. PMID: 31864346. PMCID: PMC6925840.
Article12. Sahin EK. 2020; Assessing the predictive capability of ensemble tree methods for landslide susceptibility mapping using XGBoost, gradient boosting machine, and random forest. SN Appl Sci. 2:1308. https://doi.org/10.1007/s42452-020-3060-1. DOI: 10.1007/s42452-020-3060-1.
Article13. Li D, Liu Z, Armaghani DJ, Xiao P, Zhou J. 2022; Novel ensemble intelligence methodologies for rockburst assessment in complex and variable environments. Sci Rep. 12:1844. https://doi.org/10.1038/s41598-022-05594-0. DOI: 10.1038/s41598-022-05594-0. PMID: 35115585. PMCID: PMC8814189.
Article14. Graczyk M, Lasota T, Trawiński B, Trawiński K. Nguyen NT, Le MT, Świątek J, editors. ACIIDS 2010: intelligent information and database systems. 2010. Comparison of bagging, boosting and stacking ensembles applied to real estate appraisal. Lecture Notes in Computer Science. Vol. 5991:Springer;p. 430–50. DOI: 10.1007/978-3-642-12101-2_35.
Article15. LeCun Y, Bengio Y, Hinton G. 2015; Deep learning. Nature. 521:436–44. https://doi.org/10.1038/nature14539. DOI: 10.1038/nature14539. PMID: 26017442. PMCID: PMC10308283.
Article16. Lee JK, Kim KW, Choi JY, Moon SY, Kim SG, Kim CH, et al. 2013; Bisphosphonates-related osteonecrosis of the jaw in Korea: a preliminary report. J Korean Assoc Oral Maxillofac Surg. 39:9–13. https://doi.org/10.5125/jkaoms.2013.39.1.9. DOI: 10.5125/jkaoms.2013.39.1.9. PMID: 24471011. PMCID: PMC3858159.
Article17. Sim IW, Borromeo GL, Tsao C, Hardiman R, Hofman MS, Papatziamos Hjelle C, et al. 2020; Teriparatide promotes bone healing in medication-related osteonecrosis of the jaw: a placebo-controlled, randomized trial. J Clin Oncol. 38:2971–80. https://doi.org/10.1200/jco.19.02192. DOI: 10.1200/JCO.19.02192. PMID: 32614699.
Article18. Lo JC, O'Ryan FS, Gordon NP, Yang J, Hui RL, Martin D, et al. 2010; ; Predicting Risk of Osteonecrosis of the Jaw with Oral Bisphosphonate Exposure (PROBE) Investigators. Prevalence of osteonecrosis of the jaw in patients with oral bisphosphonate exposure. J Oral Maxillofac Surg. 68:243–53. https://doi.org/10.1016/j.joms.2009.03.050. DOI: 10.1016/j.joms.2009.03.050. PMID: 19772941. PMCID: PMC10159647.
Article19. Aljohani S, Fliefel R, Ihbe J, Kühnisch J, Ehrenfeld M, Otto S. 2017; What is the effect of anti-resorptive drugs (ARDs) on the development of medication-related osteonecrosis of the jaw (MRONJ) in osteoporosis patients: a systematic review. J Craniomaxillofac Surg. 45:1493–502. https://doi.org/10.1016/j.jcms.2017.05.028. DOI: 10.1016/j.jcms.2017.05.028. PMID: 28687467.
Article20. Buchbender M, Bauerschmitz C, Pirkl S, Kesting MR, Schmitt CM. 2022; A retrospective data analysis for the risk evaluation of the development of drug-associated jaw necrosis through dentoalveolar interventions. Int J Environ Res Public Health. 19:4339. https://doi.org/10.3390/ijerph19074339. DOI: 10.3390/ijerph19074339. PMID: 35410020. PMCID: PMC8998225.
Article21. Wick A, Bankosegger P, Otto S, Hohlweg-Majert B, Steiner T, Probst F, et al. 2022; Risk factors associated with onset of medication-related osteonecrosis of the jaw in patients treated with denosumab. Clin Oral Investig. 26:2839–52. https://doi.org/10.1007/s00784-021-04261-4. DOI: 10.1007/s00784-021-04261-4. PMID: 34812959. PMCID: PMC8898220.
Article22. McGowan K, McGowan T, Ivanovski S. 2018; Risk factors for medication-related osteonecrosis of the jaws: a systematic review. Oral Dis. 24:527–36. https://doi.org/10.1111/odi.12708. DOI: 10.1111/odi.12708. PMID: 28656643.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The effect of bisphosphonate discontinuation on the incidence of postoperative medication-related osteonecrosis of the jaw after tooth extraction
- Associated systemic diseases and etiologies of medication‑related osteonecrosis of the jaw: a retrospective study of 265 surgical cases
- Medication-Related Osteonecrosis of the Jaws: A Literature Review
- Management of osteoporosis patients for prosthetic restoration
- Incidence and severity of medication-related osteonecrosis of the jaw in patients with osteoporosis using data from a Korean nationwide sample cohort in 2002 to 2019: a retrospective study