J Korean Assoc Oral Maxillofac Surg.
2023 Jun;49(3):107-113. 10.5125/jkaoms.2023.49.3.107.
Mandibular midline osteotomy for correction of bimaxillary transverse discrepancy: a technical note
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Shimane University Faculty of Medicine, Izumo, Japan
- KMID: 2544312
- DOI: http://doi.org/10.5125/jkaoms.2023.49.3.107
Abstract
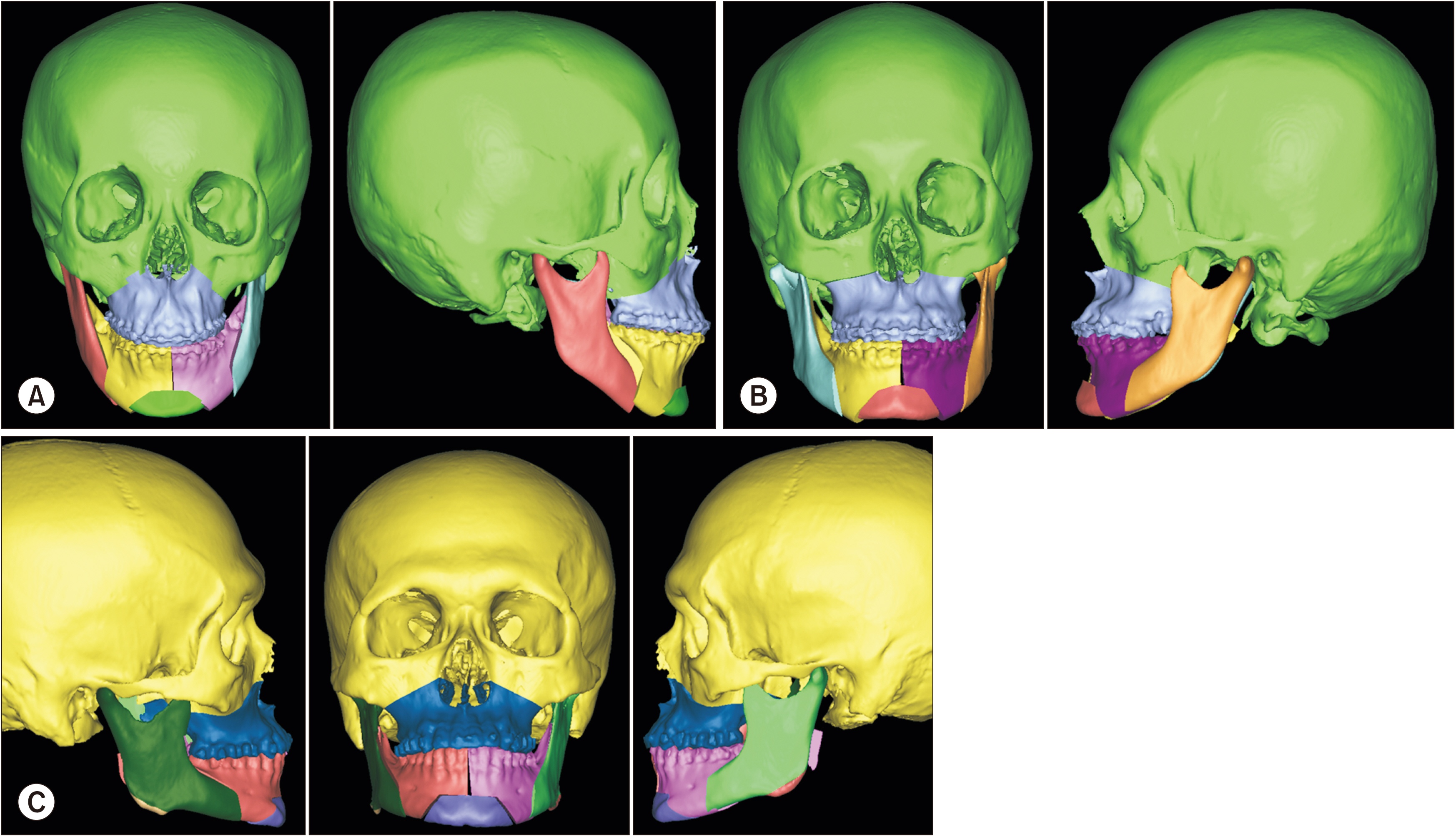
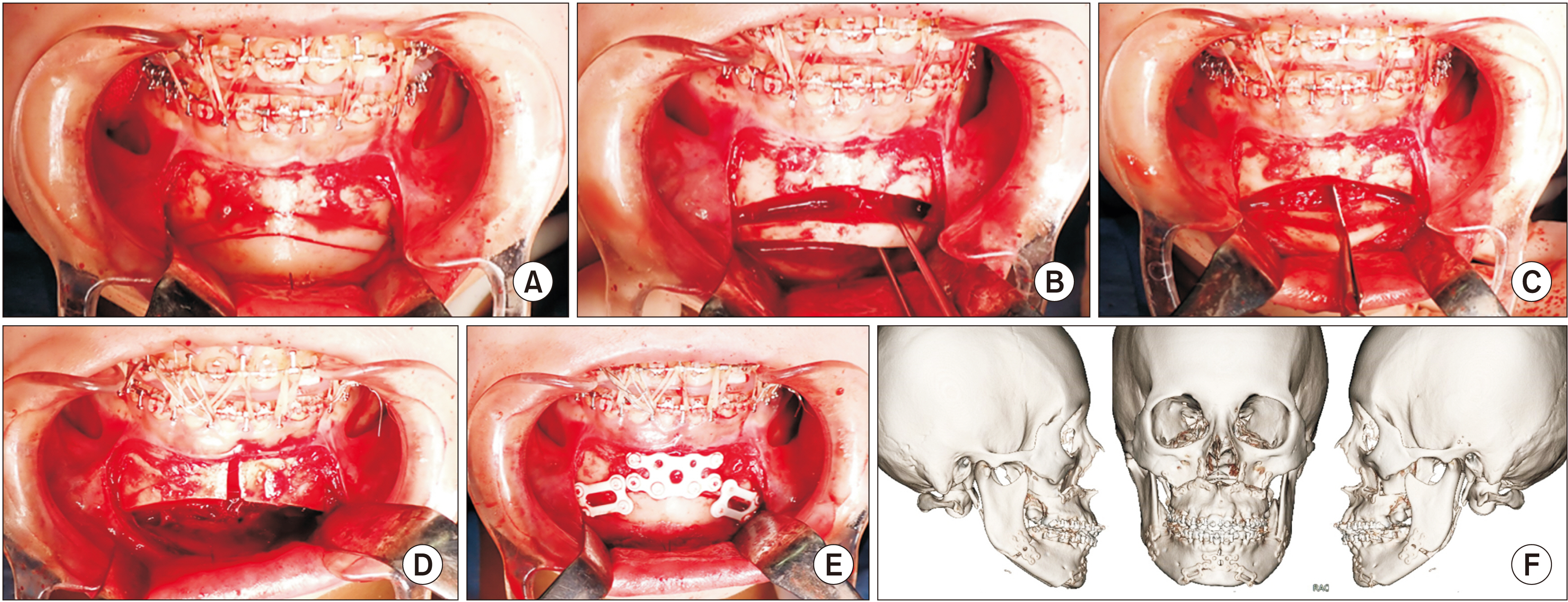
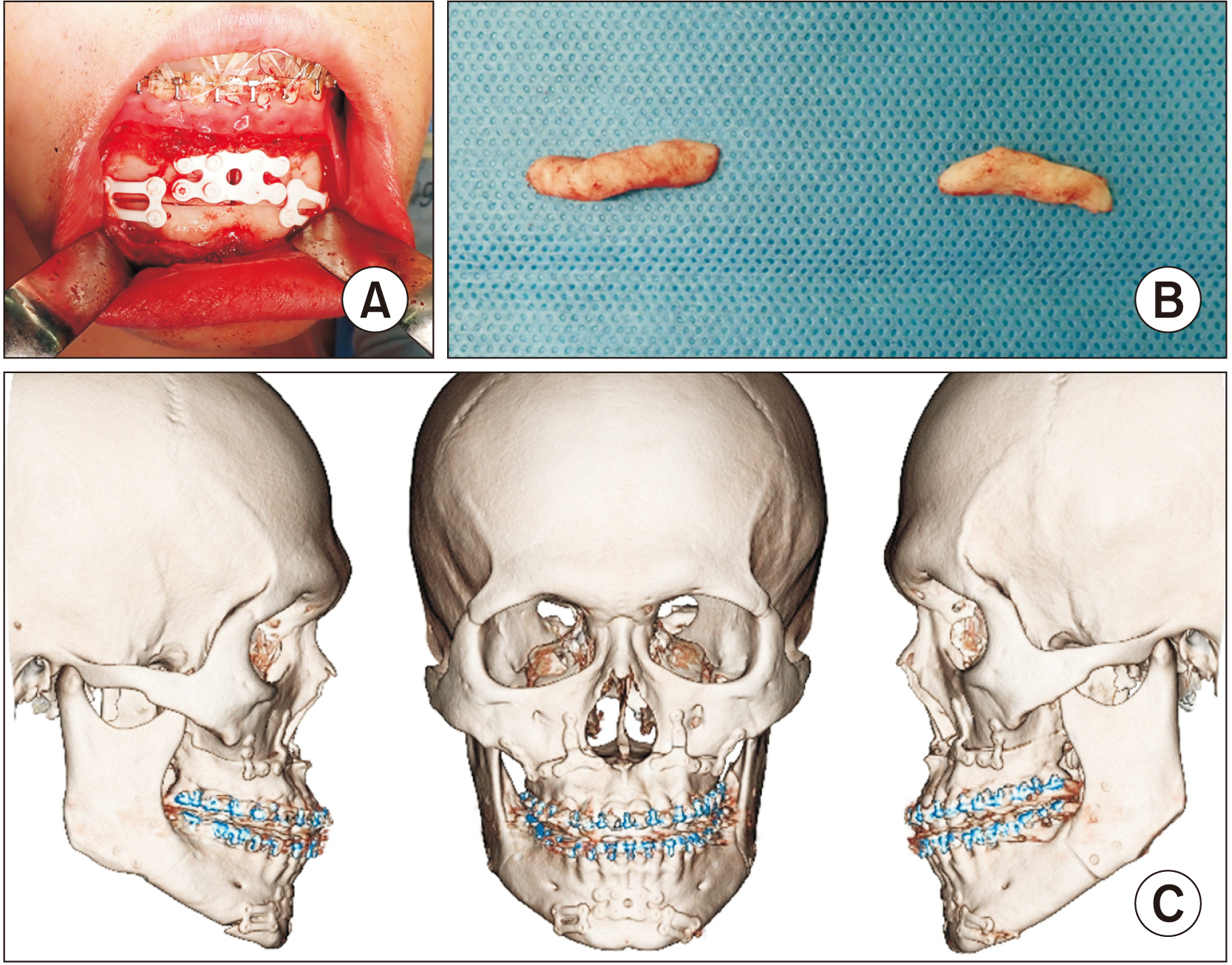
- Bimaxillary transverse width discrepancies are commonly encountered among patients with dentofacial deformities. Skeletal discrepancies should be diagnosed and managed appropriately with possible surgical corrections. Transverse width deficiencies can present in varieties of combinations involving the maxilla and mandible. We observed that in a significant proportion of cases, the maxilla is normal, and the mandible showed deficiency in the transverse dimension after pre-surgical orthodontics. We designed novel osteotomy techniques to enhance mandibular transverse width correction, as well as simultaneous genioplasty. Chin repositioning along any plane is applicable concomitant with mandibular midline arch widening. When there is a requirement for larger widening, gonial angle reduction may be necessary. This technical note focuses on key points in management of patients with transversely deficient mandible and the factors affecting the outcome and stability. Further research on the maximum amount of stable widening will be conducted. We believe that developing evidence-based additional modifications to existing conventional surgical procedures can aid precise correction of complex dentofacial deformities.
Figure
Reference
-
References
1. Andrucioli MCD, Matsumoto MAN. 2020; Transverse maxillary deficiency: treatment alternatives in face of early skeletal maturation. Dental Press J Orthod. 25:70–9. https://doi.org/10.1590/2177-6709.25.1.070-079.bbo. DOI: 10.1590/2177-6709.25.1.070-079.bbo. PMID: 32215481. PMCID: PMC7077945.
Article2. Starch-Jensen T, Blæhr TL. 2016; Transverse expansion and stability after segmental Le Fort I osteotomy versus surgically assisted rapid maxillary expansion: a systematic review. J Oral Maxillofac Res. 7:e1. https://doi.org/10.5037/jomr.2016.7401. DOI: 10.5037/jomr.2016.7401. PMID: 28154745. PMCID: PMC5279767.
Article3. Corega C, Corega M, Băciuţ M, Vaida L, Wangerin K, Bran S, et al. 2010; Bimaxillary distraction osteogenesis--an effective approach for the transverse jaw discrepancies in adults. Chirurgia (Bucur). 105:571–5. PMID: 20941985.4. Aktop P, Biren S, Aktop S, Motro M, Delilbasi C, Gurler G, et al. 2018; Evaluation of two different rapid maxillary expansion surgical techniques and their effects on the malar complex based on 3d cone-beam computed tomography. Niger J Clin Pract. 21:13–21. https://doi.org/10.4103/1119-3077.224794. DOI: 10.4103/1119-3077.224794. PMID: 29411717.
Article5. Lee HW, Kim SJ, Kwon YD. 2015; Salvage rapid maxillary expansion for the relapse of maxillary transverse expansion after Le Fort I with parasagittal osteotomy. J Korean Assoc Oral Maxillofac Surg. 41:97–101. https://doi.org/10.5125/jkaoms.2015.41.2.97. DOI: 10.5125/jkaoms.2015.41.2.97. PMID: 25922822. PMCID: PMC4411735.
Article6. Morgan TA, Fridrich KL. 2001; Effects of the multiple-piece maxillary osteotomy on the periodontium. Int J Adult Orthodon Orthognath Surg. 16:255–65. PMID: 12390003.7. Hara S, Mitsugi M, Hirose H, Tatemoto Y. 2015; Combination of mandibular constriction and intraoral vertical ramus osteotomies for a transverse jaw discrepancy. Plast Reconstr Surg Glob Open. 3:e521. https://doi.org/10.1097/gox.0000000000000505. DOI: 10.1097/GOX.0000000000000505. PMID: 26495234. PMCID: PMC4596446.
Article8. Chaudhary DC, Sharma R, Bagga DS, Sharma V. 2015; Management of bimaxillary transverse discrepancy with vertical excess. J Indian Orthod Soc. 49:213–9. https://doi.org/10.4103/0301-5742.171315. DOI: 10.4103/0301-5742.171315.
Article9. Betts NJ, Sturtz DH, Aldrich DA. 2004; Treatment of transverse (width) discrepancies in patients who require isolated mandibular surgery: the case for maxillary expansion. J Oral Maxillofac Surg. 62:361–4. https://doi.org/10.1016/j.joms.2003.08.018. DOI: 10.1016/j.joms.2003.08.018. PMID: 15015171.
Article10. García Menéndez M, Perdomo Gutiérrez L, Valdés Massó D. 2021; Negative maxillary transverse discrepancy and cephalometric lateral differences according to the width of upper arch. Rev Cubana Estomatol. 58:e3627.11. Kim H, Cha KS. 2018; Evaluation of the stability of maxillary expansion using cone-beam computed tomography after segmental Le Fort I osteotomy in adult patients with skeletal Class III malocclusion. Korean J Orthod. 48:63–70. https://doi.org/10.4041/kjod.2018.48.1.63. DOI: 10.4041/kjod.2018.48.1.63. PMID: 29423378. PMCID: PMC5799308.
Article12. Housley JA, Nanda RS, Currier GF, McCune DE. 2003; Stability of transverse expansion in the mandibular arch. Am J Orthod Dentofacial Orthop. 124:288–93. https://doi.org/10.1016/s0889-5406(03)00450-5. DOI: 10.1016/S0889-5406(03)00450-5. PMID: 12970662.
Article13. Rougier G, Diner PA, Rachwalski M, Galliani E, Tomat C, Picard A, et al. 2019; Mandibular symphyseal distraction osteogenesis: 20 years of experience treating transverse deficiencies with an internal hybrid device. J Craniomaxillofac Surg. 47:586–91. https://doi.org/10.1016/j.jcms.2019.01.001. DOI: 10.1016/j.jcms.2019.01.001. PMID: 30718215.
Article14. Bloomquist D, Joondeph D. Naini FB, Gill DS, editors. 2017. Mandibular midline osteotomy. Orthognathic surgery: principles, planning and practice. Wiley-Blackwell;p. 630–4. DOI: 10.1002/9781119004370.ch37.
Article15. Bloomquist DS. 2007; Anterior segmental mandibular osteotomies for the correction of facial-skeletal deformities. Oral Maxillofac Surg Clin North Am. 19:369–79. vihttps://doi.org/10.1016/j.coms.2007.04.005. DOI: 10.1016/j.coms.2007.04.005. PMID: 18088891.
Article16. Mommaerts MY, Voisin C, Joshi Otero J, Loomans NAJ. 2019; Mandibular feminization osteotomy-preliminary results. Int J Oral Maxillofac Surg. 48:597–600. https://doi.org/10.1016/j.ijom.2018.10.003. DOI: 10.1016/j.ijom.2018.10.003. PMID: 30342756.
Article17. Guerrero CA, Bell WH, Contasti GI, Rodriguez AM. 1997; Mandibular widening by intraoral distraction osteogenesis. Br J Oral Maxillofac Surg. 35:383–92. https://doi.org/10.1016/s0266-4356(97)90712-9. DOI: 10.1016/S0266-4356(97)90712-9. PMID: 9486441.
Article18. Anghinoni ML, Magri AS, Di Blasio A, Toma L, Sesenna E. 2009; Midline mandibular osteotomy in an asymmetric patient. Angle Orthod. 79:1008–14. https://doi.org/10.2319/102908-550.1. DOI: 10.2319/102908-550.1. PMID: 19705948.
Article19. Guerrero CA, Bell WH, Mujica EV, Gonzalez M, Dominguez E. Fonseca RJ, editor. 2018. Intraoral distraction osteogenesis. Oral and maxillofacial surgery. 3rd ed. Elsevier;p. 196–221. DOI: 10.1016/s0278-2391(00)80016-6.20. Mani V. Bonanthaya K, Panneerselvam E, Manuel S, Kumar VV, Rai A, editors. 2021. Orthognathic surgery for mandible. Oral and maxillofacial surgery for the clinician. Springer;Singapore: p. 1477–512. DOI: 10.1007/978-981-15-1346-6_68.
Article21. Kanno T, Sukegawa S, Furuki Y, Nariai Y, Sekine J. 2018; Overview of innovative advances in bioresorbable plate systems for oral and maxillofacial surgery. Jpn Dent Sci Rev. 54:127–38. https://doi.org/10.1016/j.jdsr.2018.03.003. DOI: 10.1016/j.jdsr.2018.03.003. PMID: 30128060. PMCID: PMC6094489.
Article22. Budhraja NJ, Shenoi RS, Badjate SJ, Bang KO, Ingole PD, Kolte VS. 2018; Three-dimensional locking plate and conventional miniplates in the treatment of mandibular anterior fractures. Ann Maxillofac Surg. 8:73–7. https://doi.org/10.4103/ams.ams_175_17. DOI: 10.4103/ams.ams_175_17. PMID: 29963428. PMCID: PMC6018293.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sublingual hematoma as a complication of mandibular midline osteotomy: a case report and literature review
- Orthodontic treatment of Class III bimaxillary protrusion combined with subapical segmental osteotomy
- Surgical and Orthognathic Treatment of Skeletal Class III Featuring Severe Transversal and Sagittal Discrepancy: A Case Report
- Consideration of Transverse Movement of Posterior Maxilla in Orthognathic Surgery of Facial Asymmetry: Case Reports
- Stability of bimaxillary surgery involving intraoral vertical ramus osteotomy with or without presurgical miniscrew-assisted rapid palatal expansion in adult patients with skeletal Class III malocclusion