Cancer Res Treat.
2023 Jul;55(3):910-917. 10.4143/crt.2022.1432.
Overview of the National Cancer Screening Program for Colorectal Cancer in Korea over 14 Years (2004-2017)
- Affiliations
-
- 1Department of Preventive Medicine, Chung-Ang University College of Medicine, Seoul, Korea
- 2National Cancer Control Institute, National Cancer Center, Goyang, Korea
- 3Graduate School of Cancer Science and Policy, National Cancer Center, Goyang, Korea
- KMID: 2544171
- DOI: http://doi.org/10.4143/crt.2022.1432
Abstract
- Purpose
This study aimed to evaluate the participation and follow-up test compliance rates and key performance indicators of the National Cancer Screening Program (NCSP) for colorectal cancer (CRC) from 2004 to 2017.
Materials and Methods
The overall outcomes of the NCSP for CRC were analyzed using the NCSP data collected from 2004 to 2017 and the Korean Central Cancer Registry for CRC from 2005 to 2017. We cross-sectionally analyzed the participation and follow-up test compliance rates and performance indicators for each year. The trend of participation rates as an annual percentage change was assessed, and other statistical analyses were performed.
Results
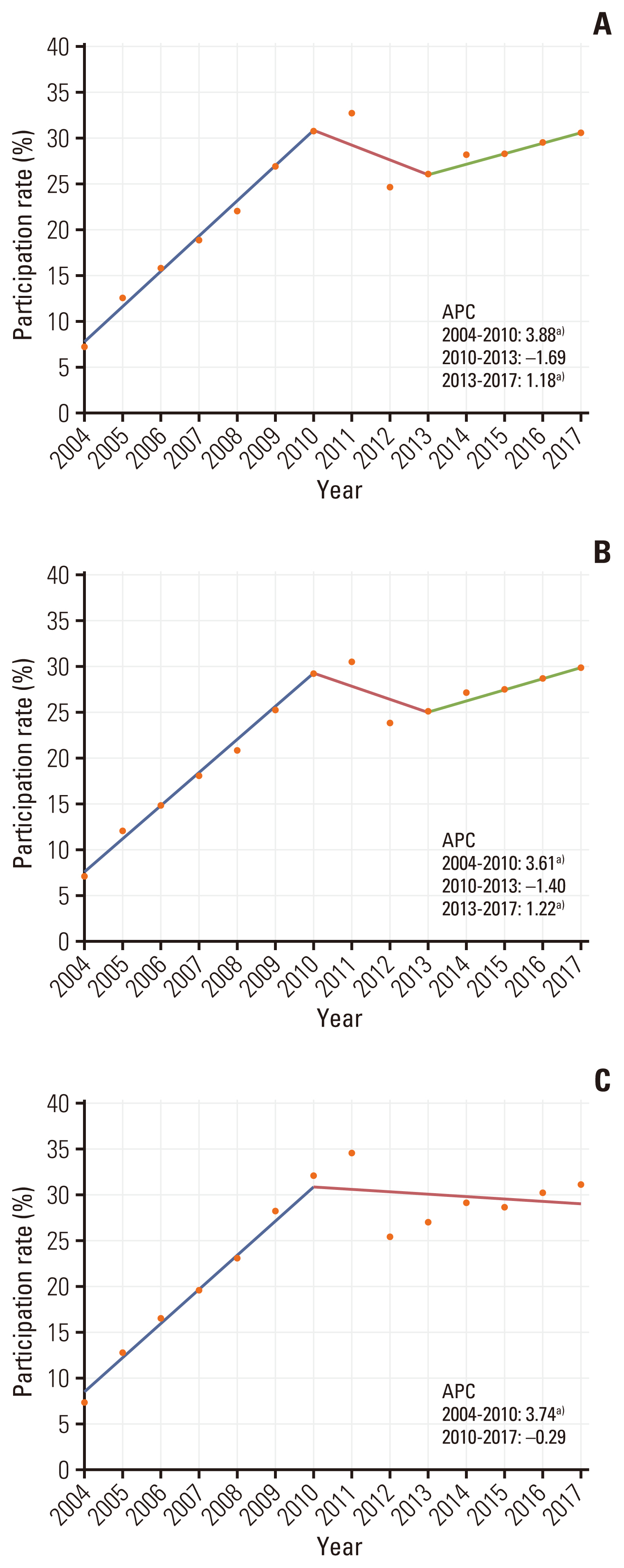
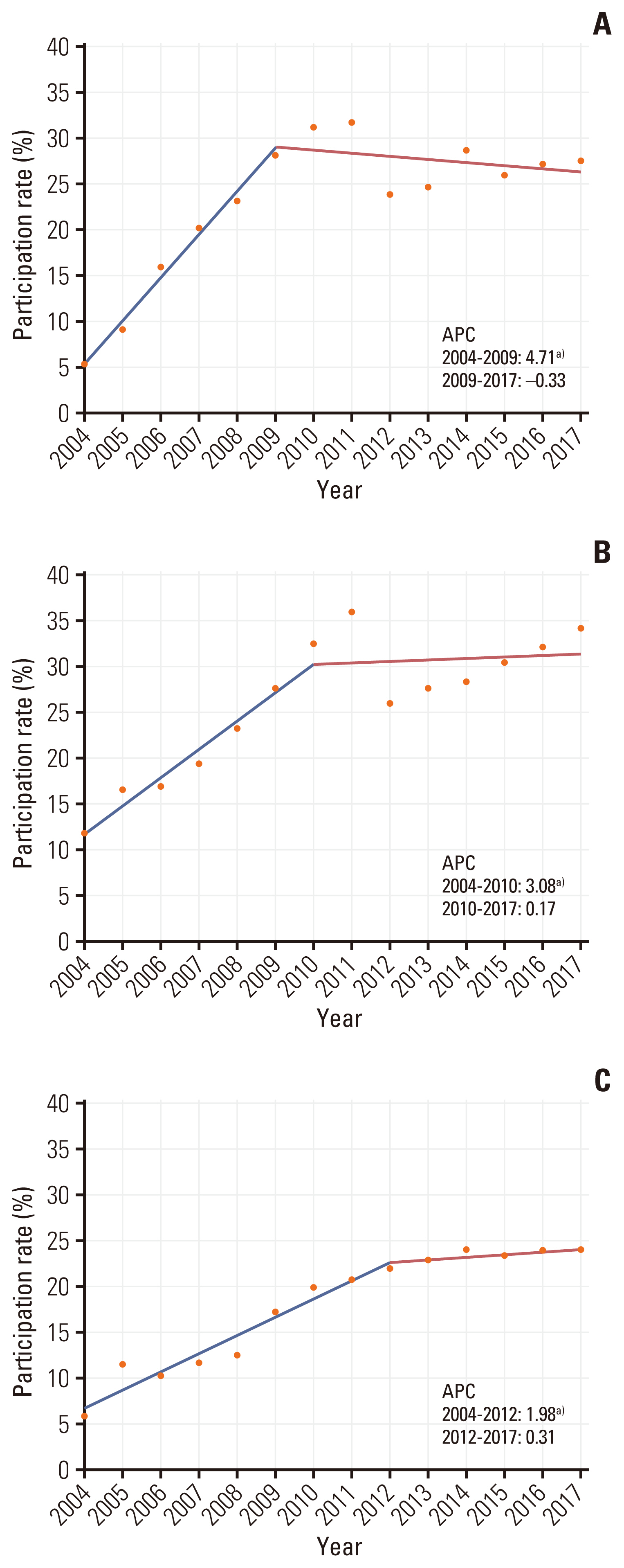
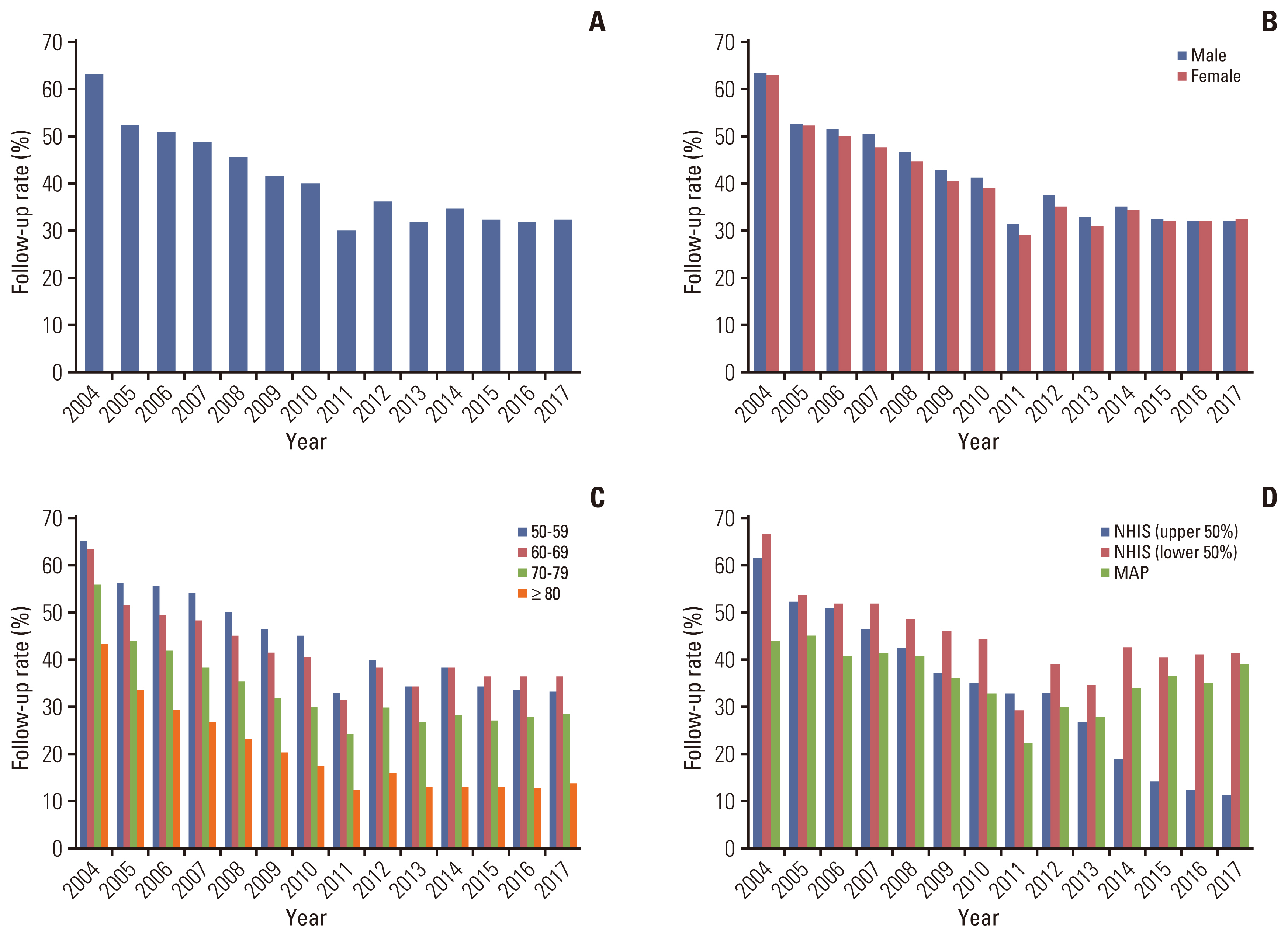
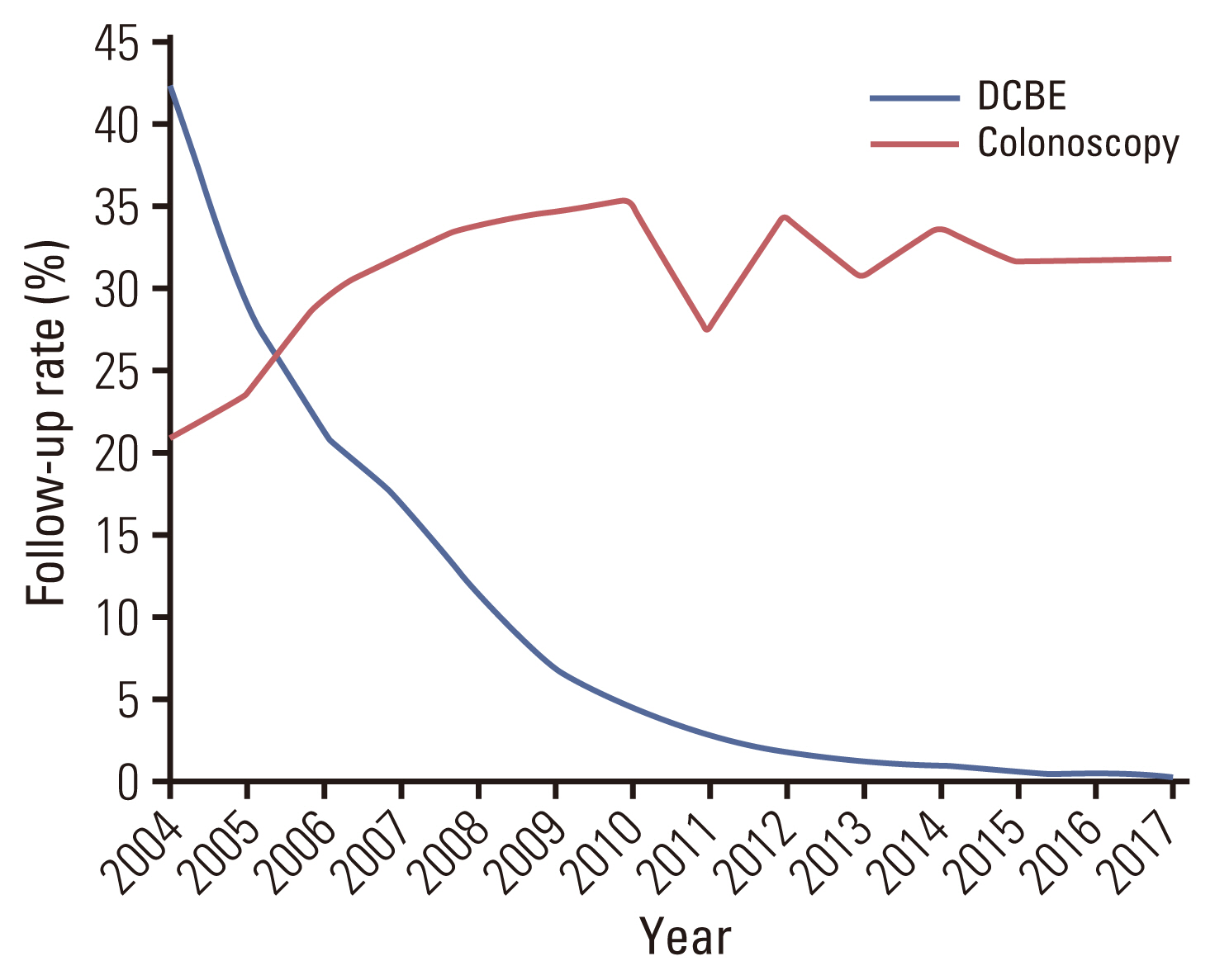
The screening participation rates increased from 7.3% in 2004 to 30.5% in 2017. Additionally, the screening rates were higher among individuals aged 60-69 years and National Health Insurance Service beneficiaries of low-income status. However, the adherence to the follow-up test decreased from 63% in 2004 to 32% in 2017. The follow-up tests using the double-contrast barium enema method decreased from 42.2% in 2004 to 0.3% in 2017. However, follow-up tests by colonoscopy increased from 21.0% in 2004 to 31.8% in 2017. Furthermore, the positivity, false-positive, and interval CRC rates decreased, whereas the specificity increased from 2004 to 2016, indicating improved performance of CRC.
Conclusion
The participation rates and performance of the NCSP for CRC have steadily improved, whereas adherence to follow-up tests has decreased. Additionally, there is a rapid growth in colonoscopy volume as a follow-up test. Continued efforts are required to improve the follow-up rates.
Figure
Cited by 2 articles
-
National cancer screening program for colorectal cancer in Korea
Seung Min Baik, Ryung-Ah Lee
Ann Surg Treat Res. 2023;105(6):333-340. doi: 10.4174/astr.2023.105.6.333.Association between Endoscopist Volume and Interval Cancers after Colonoscopy: Results from the National Colorectal Cancer Screening Program in Korea
Dong Jun Kim, Nan-He Yoon, Jae Kwan Jun, Mina Suh, Sunhwa Lee, Seongju Kim, Ji Eun Kim, Hooyeon Lee
Cancer Res Treat. 2024;56(4):1164-1170. doi: 10.4143/crt.2024.009.
Reference
-
References
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018; 68:394–424.
Article2. Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Abate D, Abbasi N, Abbastabar H, Abd-Allah F, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2017: a systematic analysis for the Global Burden of Disease Study. JAMA Oncol. 2019; 5:1749–68.3. Kang MJ, Won YJ, Lee JJ, Jung KW, Kim HJ, Kong HJ, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2019. Cancer Res Treat. 2022; 54:330–44.
Article4. Siegel R, Desantis C, Jemal A. Colorectal cancer statistics, 2014. CA Cancer J Clin. 2014; 64:104–17.5. Levin B, Lieberman DA, McFarland B, Andrews KS, Brooks D, Bond J, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology. 2008; 134:1570–95.
Article6. Smith RA, von Eschenbach AC, Wender R, Levin B, Byers T, Rothenberger D, et al. American Cancer Society guidelines for the early detection of cancer: update of early detection guidelines for prostate, colorectal, and endometrial cancers. Also: update 2001--testing for early lung cancer detection. CA Cancer J Clin. 2001; 51:38–75.
Article7. Whitlock EP, Lin JS, Liles E, Beil TL, Fu R. Screening for colorectal cancer: a targeted, updated systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2008; 149:638–58.
Article8. Chiu HM, Chang LC, Hsu WF, Chou CK, Wu MS. Non-invasive screening for colorectal cancer in Asia. Best Pract Res Clin Gastroenterol. 2015; 29:953–65.
Article9. Schreuders EH, Ruco A, Rabeneck L, Schoen RE, Sung JJ, Young GP, et al. Colorectal cancer screening: a global overview of existing programmes. Gut. 2015; 64:1637–49.
Article10. Kim Y, Jun JK, Choi KS, Lee HY, Park EC. Overview of the National Cancer Screening Programme and the cancer screening status in Korea. Asian Pac J Cancer Prev. 2011; 12:725–30.11. Final recommendation statement. Colorectal cancer: screening. Clinical considerations [Internet]. Rockville, MD: U.S. Preventive Services Task Force;2017. [cited 2020 Oct 27]. Available from: https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/colorectal-cancer-screening2#consider.12. Colorectal cancer facts & figures 2017–2019 [Internet]. Atlanta, GA: American Cancer Society;2020. [cited 2020 Oct 27]. Available from: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/colorectal-cancer-facts-and-figures/colorectal-cancerfacts-and-figures-2017-2019.pdf.13. Segnan N, Patnick J, von Karsa L. European guidelines for quality assurance in colorectal cancer screening and diagnosis. Luxembourg: Publications Office of the European Union;2010.14. Colorectal cancer screening. IARC Handbooks of Cancer Prevention. 17:[Internet]. Lyon: International Agency for Research on Cancer;2019. [cited 2020 Oct 27]. Available from: https://publications.iarc.fr/Book-And-Report-Series/Iarc-Handbooks-Of-Cancer-Prevention/Colorectal-Cancer-Screening-2019.15. Choi JH, Cha JM, Yoon JY, Kwak MS, Jeon JW, Shin HP. The current capacity and quality of colonoscopy in Korea. Intest Res. 2019; 17:119–26.16. Hong S, Lee YY, Lee J, Kim Y, Choi KS, Jun JK, et al. Trends in cancer screening rates among Korean men and women: results of the Korean National Cancer Screening Survey, 2004–2018. Cancer Res Treat. 2021; 53:330–8.
Article17. Kim YJ, Shim JI, Park E, Kang M, Kang S, Lee J, et al. Adherence to follow-up examination after positive fecal occult blood test results affects colorectal cancer mortality: a Korea population-based cohort study. Dig Liver Dis. 2021; 53:631–8.
Article18. Cho YH, Kim DH, Cha JM, Jeen YT, Moon JS, Kim JO, et al. Patients’ preferences for primary colorectal cancer screening: a survey of the National Colorectal Cancer Screening Program in Korea. Gut Liver. 2017; 11:821–7.
Article19. Park B, Jun JK, Kim BC, Choi KS, Suh M; The Expert Advisory Committee, et al. Korean colonoscopy screening pilot study (K-cospi) for screening colorectal cancer: study protocol for the multicenter, community-based clinical trial. BMC Gastroenterol. 2021; 21:36.
Article20. Sohn DK, Kim MJ, Park Y, Suh M, Shin A, Lee HY, et al. The Korean guideline for colorectal cancer screening. J Korean Med Assoc. 2015; 58:420–32.
Article21. Jones RM, Devers KJ, Kuzel AJ, Woolf SH. Patient-reported barriers to colorectal cancer screening: a mixed-methods analysis. Am J Prev Med. 2010; 38:508–16.22. Kweon SS, Kim MG, Kang MR, Shin MH, Choi JS. Difference of stage at cancer diagnosis by socioeconomic status for four target cancers of the National Cancer Screening Program in Korea: Results from the Gwangju and Jeonnam cancer registries. J Epidemiol. 2017; 27:299–304.
Article23. Lee YY, Jun JK, Suh M, Park BY, Kim Y, Choi KS. Barriers to cancer screening among medical aid program recipients in the Republic of Korea: a qualitative study. Asian Pac J Cancer Prev. 2014; 15:589–94.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Screening strategy for colorectal cancer according to risk
- National cancer screening program for colorectal cancer in Korea
- Screening of gastric cancer
- Trends in Cancer Screening Rates among Korean Men and Women: Results from the Korean National Cancer Screening Survey (KNCSS), 2004-2011
- Trends in Participation Rates for the National Cancer Screening Program in Korea, 2002-2012