Korean J Transplant.
2023 Jun;37(2):124-128. 10.4285/kjt.23.0006.
Right lumbar lymph trunk injury after right laparoscopic donor nephrectomy: a case report
- Affiliations
-
- 1Department of Radiology, Viet Duc University Hospital, Hanoi, Vietnam
- 2Department of Radiology, University of Medicine and Pharmacy (VNU-UMP), Vietnam National University, Hanoi, Vietnam
- 3Organ Transplantation Center, Viet Duc University Hospital, Hanoi, Vietnam
- 4Department of Urology, University of Medicine and Pharmacy (VNU-UMP), Vietnam National University, Hanoi, Vietnam
- KMID: 2544117
- DOI: http://doi.org/10.4285/kjt.23.0006
Abstract
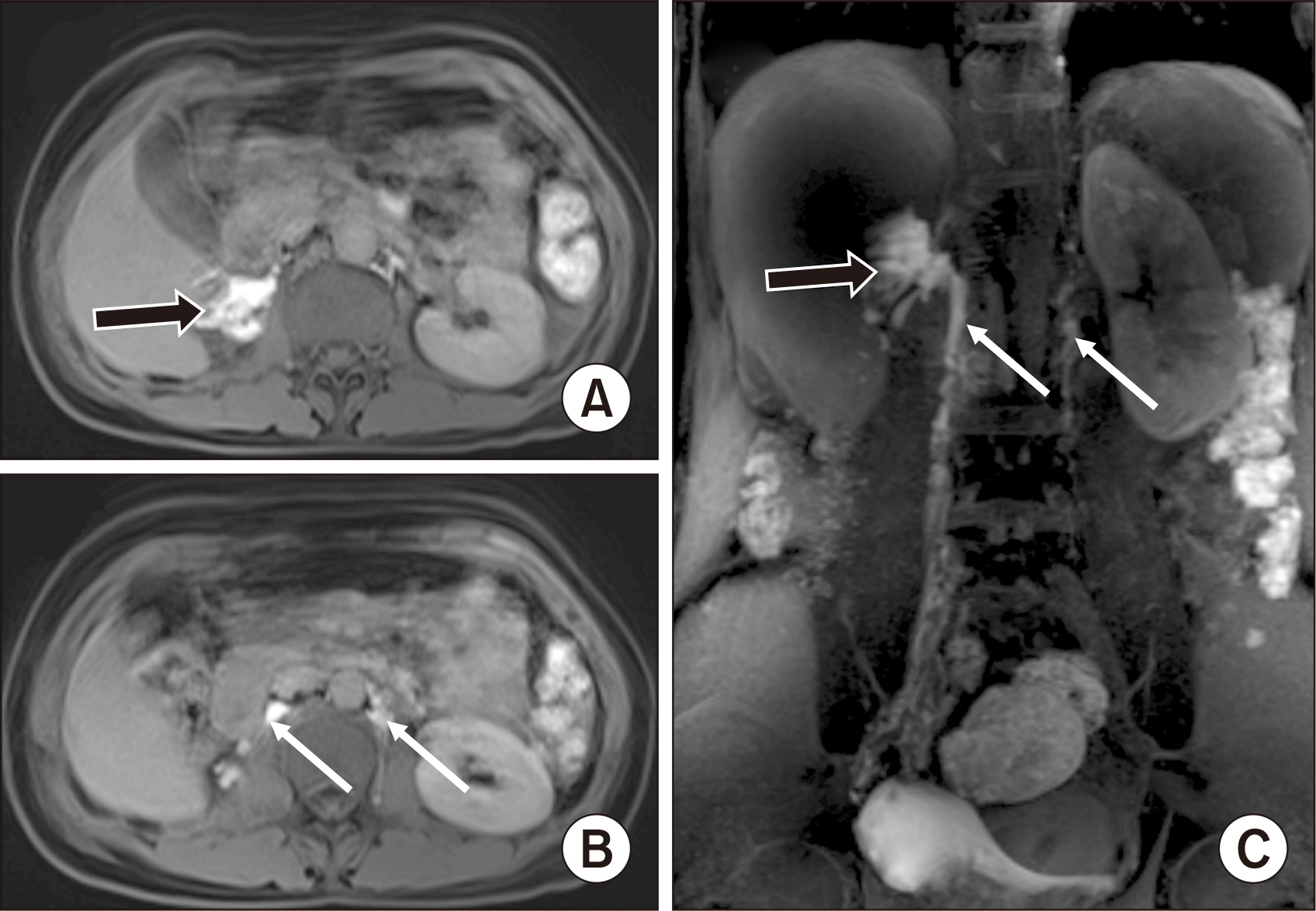
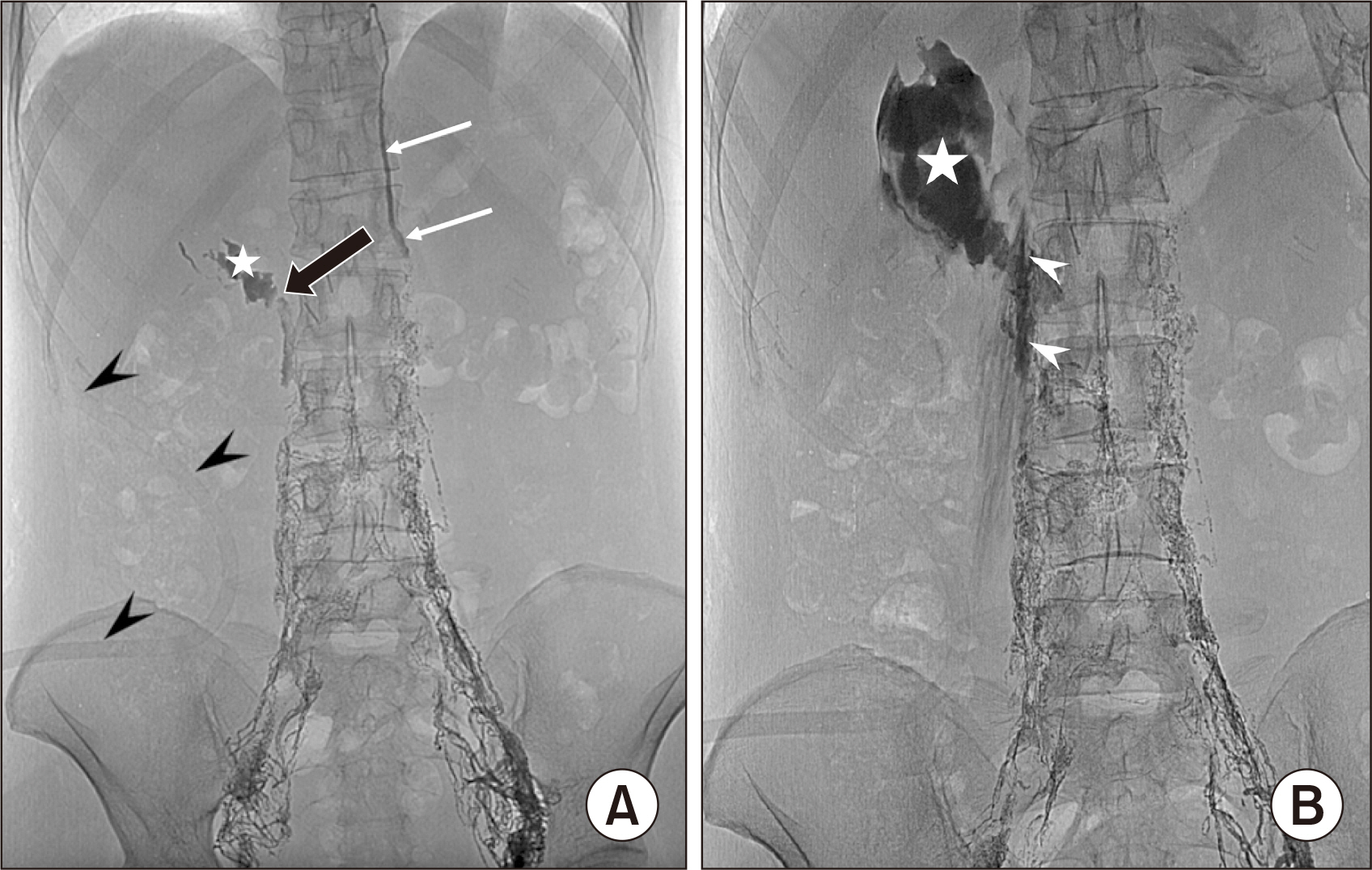
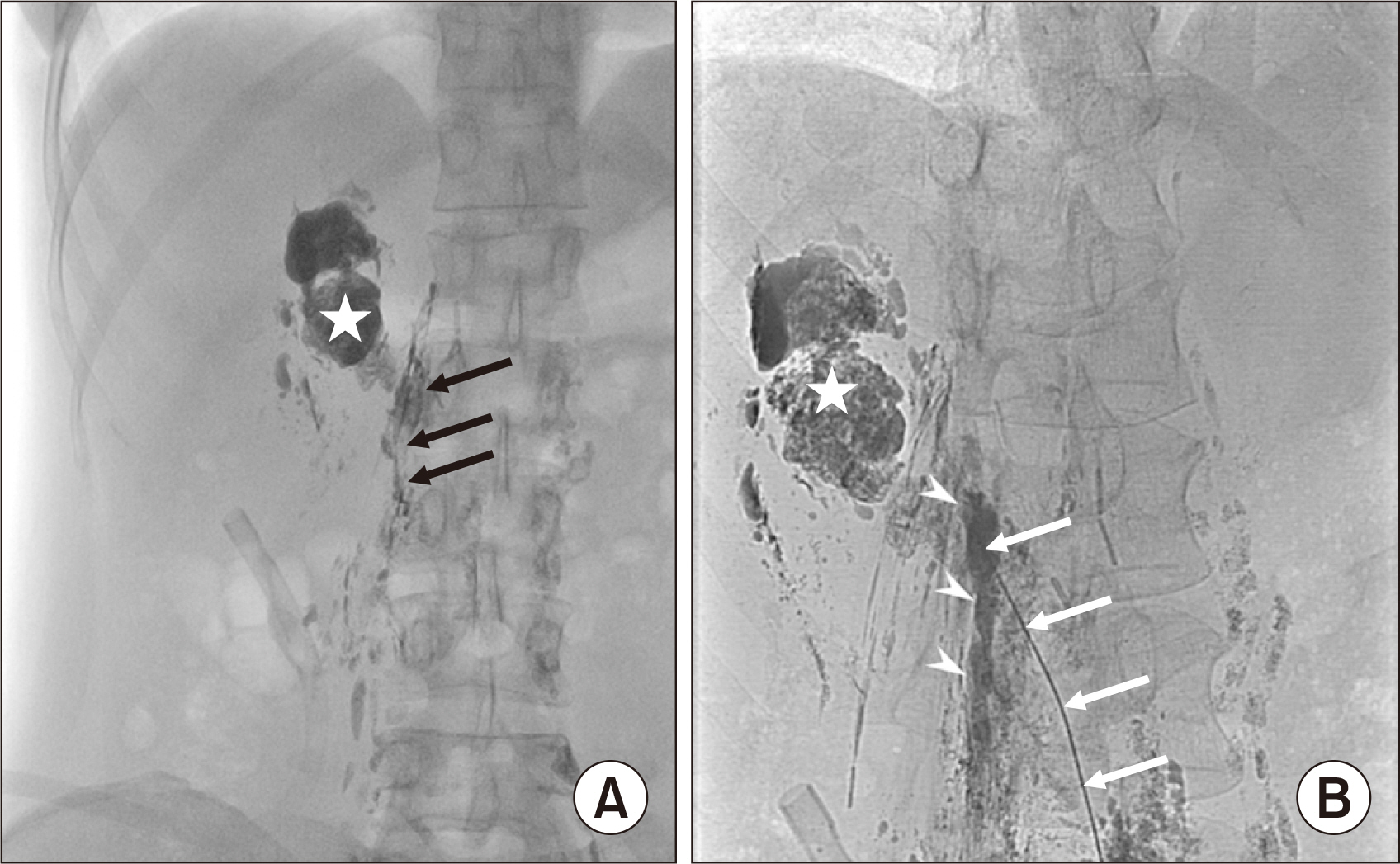
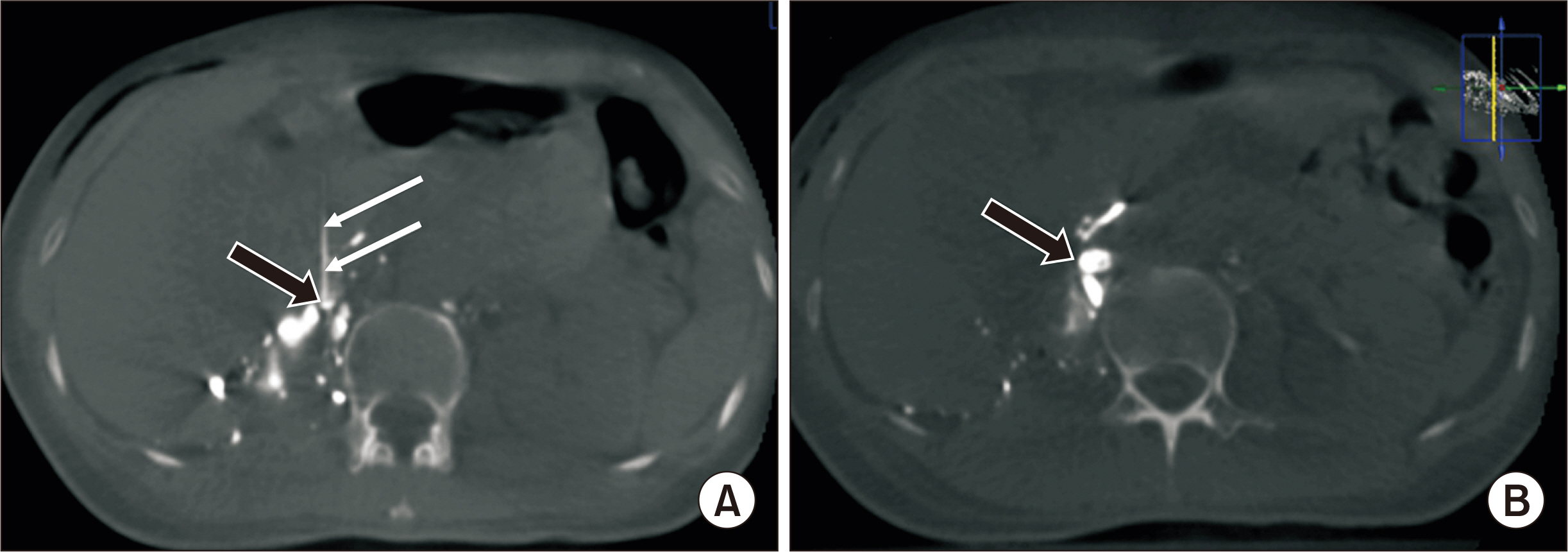
- Laparoscopic donor nephrectomy (LDN) is increasingly popular because of its advantages over open surgery. Chyle leak after donor nephrectomy is a rare but potentially lethal complication if not treated appropriately. We describe a case of a 43-year-old female patient with no remarkable history who presented a chyle leak on day 2 after right transperitoneal LDN. Since conservative treatment failed, the patient underwent magnetic resonance imaging (MRI) and intranodal lipiodol lymphangiography, which confirmed the chyle leak from the right lumbar lymph trunk into the right renal fossa. The chyle leak was percutaneously embolized twice, on postoperative day (POD) 5 and POD 10, by a mixture of N-butyl-2-cyanoacrylate and lipiodol. The drainage fluid decreased significantly after the second embolization. The subhepatic drainage tube was withdrawn on POD 14, and the patient was discharged on POD 17. MRI lymphangiography and intranodal lipiodol lymphangiography effectively identified the chyle leak point. Percutaneous embolization seems to be a safe, effective method for treating high-output chyle leaks.
Figure
Reference
-
1. Shafizadeh S, McEvoy JR, Murray C, Baillie GM, Ashcraft E, Sill T, et al. 2000; Laparoscopic donor nephrectomy: impact on an established renal transplant program. Am Surg. 66:1132–5. DOI: 10.1177/000313480006601208. PMID: 11149584.
Article2. Simon SD, Castle EP, Ferrigni RG, Lamm DL, Swanson SK, Novicki DE, et al. 2004; Complications of laparoscopic nephrectomy: the Mayo Clinic experience. J Urol. 171:1447–50. DOI: 10.1097/01.ju.0000117942.61971.41. PMID: 15017195.
Article3. Minnee RC, Idu MM. 2010; Laparoscopic donor nephrectomy. Neth J Med. 68:199–206.4. Seth A, Sharma A, Kenwar DB, Singh S. 2019; Chylous ascites: complication of laparoscopic donor nephrectomy. Case report and review of literature. Transplantation. 103:e74–8. DOI: 10.1097/TP.0000000000002514. PMID: 30399121.
Article5. Capocasale E, Iaria M, Vistoli F, Signori S, Mazzoni MP, Dalla Valle R, et al. 2012; Incidence, diagnosis, and treatment of chylous leakage after laparoscopic live donor nephrectomy. Transplantation. 93:82–6. DOI: 10.1097/TP.0b013e31823b2d8e. PMID: 22143459.
Article6. Bachmann A, Ruszat R, Dickenmann M, Giannini O, Mayr M, Steiger J, et al. 2005; Chyloretroperitoneum with secondary chylothorax after retroperitoneoscopic donor nephrectomy. Urology. 66:881. DOI: 10.1016/j.urology.2005.04.025. PMID: 16230168.
Article7. Leibovitch I, Mor Y, Golomb J, Ramon J. 2002; The diagnosis and management of postoperative chylous ascites. J Urol. 167(2 Pt 1):449–57. DOI: 10.1016/S0022-5347(01)69064-5. PMID: 11792897.
Article8. Lv S, Wang Q, Zhao W, Han L, Wang Q, Batchu N, et al. 2017; A review of the postoperative lymphatic leakage. Oncotarget. 8:69062–75. DOI: 10.18632/oncotarget.17297. PMID: 28978181. PMCID: PMC5620321.
Article9. Simon SP, Thomas J, Nair TB, Bhat SH. 2020; A rare complication after laparoscopic donor nephrectomy: chyle leak-a case report. Indian J Transplant. 14:374–6. DOI: 10.4103/ijot.ijot_43_20.
Article10. Kalia S, Narkhede A, Yadav AK, Bhalla AK, Gupta A. 2022; Retrograde transvenous selective lymphatic duct embolization in post donor nephrectomy chylous ascites. CEN Case Rep. 11:1–5. DOI: 10.1007/s13730-021-00618-6. PMID: 34218419. PMCID: PMC8811106.
Article11. Jairath A, Singh A, Ganpule A, Mishra S, Sabnis R, Desai M. 2015; Management protocol for chylous ascites after laparoscopic nephrectomy. Urology. 86:521–8. DOI: 10.1016/j.urology.2015.06.001. PMID: 26210005.
Article12. Pinto PS, Sirlin CB, Andrade-Barreto OA, Brown MA, Mindelzun RE, Mattrey RF. 2004; Cisterna chyli at routine abdominal MR imaging: a normal anatomic structure in the retrocrural space. Radiographics. 24:809–17. DOI: 10.1148/rg.243035086. PMID: 15143230.
Article13. Kwon LM, Hur S, Jeong CW, Jae HJ, Chung JW. 2021; Glue embolization of lymphopseudoaneurysm for chylous ascites after retroperitoneal surgery. Korean J Radiol. 22:376–83. DOI: 10.3348/kjr.2020.0056. PMID: 32901460. PMCID: PMC7909856.
Article14. Vu LN, Nghia NQ, Thanh DT, Giang TB, Nga VT, Bui LM, et al. 2019; Laparoscopic living donor right nephrectomy: assessment of outcome and association of BMI to length of right renal vein. Actas Urol Esp (Engl Ed). 43:536–42. DOI: 10.1016/j.acuroe.2019.05.009.
Article15. Tiong HY, Goel RK, White WM, Goldfarb DA, Kaouk JH. 2015; Chylous ascites after laparoscopic donor nephrectomy. Asian J Endosc Surg. 8:34–9. DOI: 10.1111/ases.12144. PMID: 25384614.
Article16. Itou C, Koizumi J, Myojin K, Yamashita T, Mori N, Imai Y. 2013; A case of refractory chylous ascites after nephrectomy successfully treated with percutaneous obliteration using adhesive glue. Jpn J Radiol. 31:71–4. DOI: 10.1007/s11604-012-0146-8. PMID: 23065489.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Severe Hypercarbia by Subcutaneous Emphysema Occurring during Hand Assisted Laparoscopic Donor Nephrectomy: A case report
- Video Assisted Minilaparotomy Surgery (VAMS) - Live Donor Nephrectomy: 239 Cases
- Video Assisted Minilaparotomy Surgery (VAMS) Live Donor Nephrectomy
- Lumbar plexopathy after radical nephrectomy: A case report
- Rhabdomyolysis after laparoscopic radical nephrectomy: A case report