J Korean Med Sci.
2023 Jun;38(25):e188. 10.3346/jkms.2023.38.e188.
All-Cause and Cause-Specific Mortality Attributable to Seasonal Influenza: A Nationwide Matched Cohort Study
- Affiliations
-
- 1Department of Preventive Medicine, Yonsei University College of Medicine, Seoul, Korea
- 2Institute of Human Complexity and Systems Science, Yonsei University, Incheon, Korea
- 3Institute for Environmental Research, Yonsei University College of Medicine, Seoul, Korea
- 4National Health Insurance Service, Wonju, Korea
- 5Gyeongnam Regional Center, Korea Disease Control and Prevention Agency, Busan, Korea
- 6Division of Public Health Science, Graduate School of Public Health, Seoul National University, Seoul, Korea
- 7Department of Preventive Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea
- KMID: 2543979
- DOI: http://doi.org/10.3346/jkms.2023.38.e188
Abstract
- Background
Although influenza poses substantial mortality burden, most studies have estimated excess mortality using time-aggregated data. Here, we estimated mortality risk and population attributable fraction (PAF) attributed to seasonal influenza using individual-level data from a nationwide matched cohort.
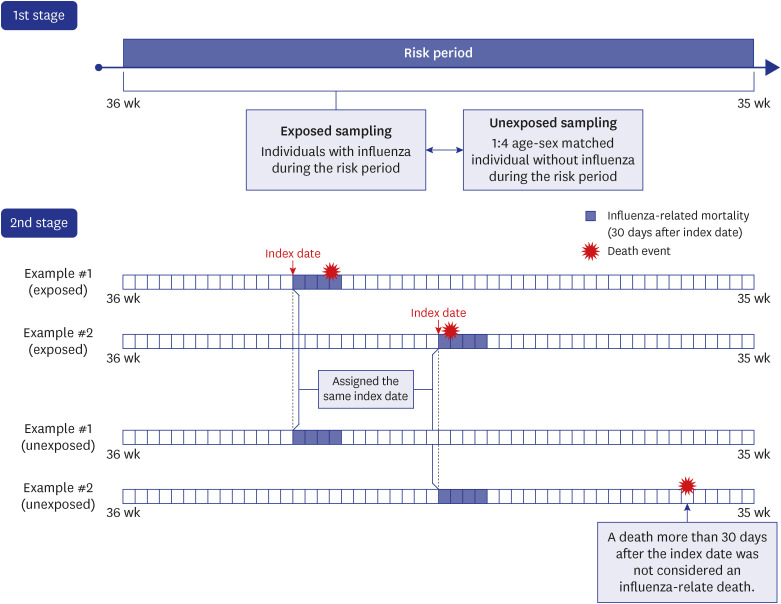
Methods
Individuals with influenza during four consecutive influenza seasons (2013–2017) (n = 5,497,812) and 1:4 age- and sex-matched individuals without influenza (n = 20,990,683) were identified from a national health insurance database. The endpoint was mortality within 30 days after influenza diagnosis. All-cause and cause-specific mortality risk ratios (RRs) attributed to influenza were estimated. Excess mortality, mortality RR, and PAF of mortality were determined, including for underlying disease subgroups.
Results
Excess mortality rate, mortality RR, and PAF of all-cause mortality were 49.5 per 100,000, 4.03 (95% confidence interval [CI], 3.63–4.48), and 5.6% (95% CI, 4.5–6.7%). Cause-specific mortality RR (12.85; 95% CI, 9.40–17.55) and PAF (20.7%; 95% CI, 13.2– 27.0%) were highest for respiratory diseases. In subgroup analysis according to underlying disorders, PAF of all-cause mortality was 5.9% (95% CI, 0.6–10.7%) for liver disease, 5.8% (95% CI, 2.9–8.5%) for respiratory disease, and 3.8% (95% CI, 1.4–6.1%) for cancer.
Conclusion
Individuals with influenza had a 4-fold higher mortality risk than individuals without influenza. Preventing seasonal influenza may lead to 5.6% and 20.7% reductions in all-cause and respiratory mortality, respectively. Individuals with respiratory disease, liver disease, and cancer may benefit from prioritization when establishing influenza prevention strategies.
Keyword
Figure
Reference
-
1. Glezen WP. Serious morbidity and mortality associated with influenza epidemics. Epidemiol Rev. 1982; 4(1):25–44. PMID: 6754408.2. World Health Organization. Influenza, fact sheet No. 211. Updated 2014. Accessed September 24, 2021. https://www.who.int/en/news-room/fact-sheets/detail/influenza-(seasonal) .3. Putri WC, Muscatello DJ, Stockwell MS, Newall AT. Economic burden of seasonal influenza in the United States. Vaccine. 2018; 36(27):3960–3966. PMID: 29801998.4. Paget J, Spreeuwenberg P, Charu V, Taylor RJ, Iuliano AD, Bresee J, et al. Global mortality associated with seasonal influenza epidemics: new burden estimates and predictors from the GLaMOR Project. J Glob Health. 2019; 9(2):020421. PMID: 31673337.5. Bai L, Zhao Y, Dong J, Liang S, Guo M, Liu X, et al. Coinfection with influenza A virus enhances SARS-CoV-2 infectivity. Cell Res. 2021; 31(4):395–403. PMID: 33603116.6. Cuadrado-Payán E, Montagud-Marrahi E, Torres-Elorza M, Bodro M, Blasco M, Poch E, et al. SARS-CoV-2 and influenza virus co-infection. Lancet. 2020; 395(10236):e84. PMID: 32423586.7. Centers for Disease Control and Prevention. People at higher risk of flu complications. Updated 2021. Accessed September 24, 2021. https://www.cdc.gov/flu/highrisk/index.htm .8. Seong SC, Kim YY, Khang YH, Park JH, Kang HJ, Lee H, et al. Data resource profile: the National Health Information Database of the National Health Insurance Service in South Korea. Int J Epidemiol. 2017; 46(3):799–800. PMID: 27794523.9. Kim IS. Epidemiological usefulness of registered death information in Korea. Korean J Epidemiol. 1989; 11(2):143–149.10. Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005; 43(11):1130–1139. PMID: 16224307.11. Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010; 137(2):263–272. PMID: 19762550.12. Kaplan RM, Koehler J, Ziegler PD, Sarkar S, Zweibel S, Passman RS. Stroke risk as a function of atrial fibrillation duration and CHA2DS2-VASc score. Circulation. 2019; 140(20):1639–1646. PMID: 31564126.13. Altman DG, Bland JM. Interaction revisited: the difference between two estimates. BMJ. 2003; 326(7382):219. PMID: 12543843.14. Li J, Chen Y, Wang X, Yu H. Influenza-associated disease burden in mainland China: a systematic review and meta-analysis. Sci Rep. 2021; 11(1):2886. PMID: 33536462.15. Quandelacy TM, Viboud C, Charu V, Lipsitch M, Goldstein E. Age- and sex-related risk factors for influenza-associated mortality in the United States between 1997-2007. Am J Epidemiol. 2014; 179(2):156–167. PMID: 24190951.16. Hong K, Sohn S, Chun BC. Estimating influenza-associated mortality in Korea: the 2009-2016 seasons. J Prev Med Public Health. 2019; 52(5):308–315. PMID: 31588700.17. Cooper BS, Kotirum S, Kulpeng W, Praditsitthikorn N, Chittaganpitch M, Limmathurotsakul D, et al. Mortality attributable to seasonal influenza A and B infections in Thailand, 2005-2009: a longitudinal study. Am J Epidemiol. 2015; 181(11):898–907. PMID: 25899091.18. Cunningham E, Kohli R, Venuto RC. Influenza-associated myoglobinuric renal failure. JAMA. 1979; 242(22):2428–2429. PMID: 490855.19. World Health Organization. WHO Guidelines for Pharmacological Management of Pandemic Influenza A (H1N1) 2009 and Other Influenza Viruses: Part II Review of Evidence. Geneva, Switzerland: World Health Organization;2010.20. Mertz D, Kim TH, Johnstone J, Lam PP, Science M, Kuster SP, et al. Populations at risk for severe or complicated influenza illness: systematic review and meta-analysis. BMJ. 2013; 347:f5061. PMID: 23974637.21. Kim SH, Park HY, Jung H, Zo S, Kim S, Park DW, et al. Trends and factors associated with influenza vaccination in subjects with asthma: analysis of the Korea National Health and Nutrition Examination Survey between 2010 and 2019. Ther Adv Chronic Dis. 2022; 13:20406223221123979. PMID: 36213169.22. Lee H, Choi H, Jo YS. Trends in influenza vaccination rates in participants with airflow limitation: the Korea National Health and Nutrition Examination Survey 2007-2018. Front Med (Lausanne). 2022; 9(9):870617. PMID: 35592859.23. Byeon KH, Kim J, Choi BY, Kim JY, Lee N. Factors affecting the incidence of hospitalized pneumonia after influenza infection in Korea using the National Health Insurance Research Database, 2014-2018: focusing on the effect of antiviral therapy in the 2017 flu season. J Korean Med Sci. 2020; 35(38):e318. PMID: 32989929.24. Park HJ, Byun MK, Kim T, Rhee CK, Kim K, Kim BY, et al. Frequent outpatient visits prevent exacerbation of chronic obstructive pulmonary disease. Sci Rep. 2020; 10(1):6049. PMID: 32269274.25. Park HJ, Byun MK, Kim HJ, Ahn CM, Rhee CK, Kim K, et al. Regular follow-up visits reduce the risk for asthma exacerbation requiring admission in Korean adults with asthma. Allergy Asthma Clin Immunol. 2018; 14(1):29. PMID: 30002684.26. Thompson WW, Shay DK, Weintraub E, Brammer L, Cox N, Anderson LJ, et al. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA. 2003; 289(2):179–186. PMID: 12517228.27. Warren-Gash C, Smeeth L, Hayward AC. Influenza as a trigger for acute myocardial infarction or death from cardiovascular disease: a systematic review. Lancet Infect Dis. 2009; 9(10):601–610. PMID: 19778762.28. Fiore AE, Fry A, Shay D, Gubareva L, Bresee JS, Uyeki TM, et al. Antiviral agents for the treatment and chemoprophylaxis of influenza --- recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2011; 60(1):1–24.29. Centers for Disease Control and Prevention. Influenza: the disease. Updated 2022. Accessed November 24, 2021. http://www.cdc.gov/flu/about/disease/index.htm .30. Bader MS. Immunization for the elderly. Am J Med Sci. 2007; 334(6):481–486. PMID: 18091370.31. Leung NH, Xu C, Ip DK, Cowling BJ. The fraction of influenza virus infections that are asymptomatic: a systematic review and meta-analysis. Epidemiology. 2015; 26(6):862–872. PMID: 26133025.32. Korea Disease Control and Prevention Agency. Influenza vaccination coverage statistics. Updated 2021. Accessed September 27, 2021. https://health.kdca.go.kr/healthinfo/biz/pblcVis/details.do?ctgrSn=71 .33. Byeon KH, Kim J, Choi B, Choi BY. The coverage rates for influenza vaccination and related factors in Korean adults aged 50 and older with chronic disease: based on 2016 Community Health Survey data. Epidemiol Health. 2018; 40:e2018034. PMID: 30056640.34. Cha SH, Paik JH, Lee MR, Yang H, Park SG, Jeon YJ, et al. Influenza vaccination coverage rate according to the pulmonary function of Korean adults aged 40 years and over: analysis of the fifth Korean National Health and Nutrition Examination Survey. J Korean Med Sci. 2016; 31(5):709–714. PMID: 27134491.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Interpretation of Positive Result for Influenza A and Negative Result for Novel Influenza A/H1N1 in Reverse Transcriptase PCR for Novel Influenza A/H1N1
- The National Influenza Surveillance System of Korea
- Estimating Influenza-associated Mortality in Korea: The 2009–2016 Seasons
- Seasonal influenza and vaccine herd effect
- Prevention and Treatment of Influenza