Pediatr Emerg Med J.
2023 Jul;10(3):77-86. 10.22470/pemj.2023.00675.
Pediatric application of cuffed endotracheal tube: a secondary publication translated into Korean
- Affiliations
-
- 1Department of Emergency Medicine, Ajou University School of Medicine, Suwon, Republic of Korea
- 2Department of Anesthesiology, Ajou University School of Medicine, Suwon, Republic of Korea
- KMID: 2543574
- DOI: http://doi.org/10.22470/pemj.2023.00675
Abstract
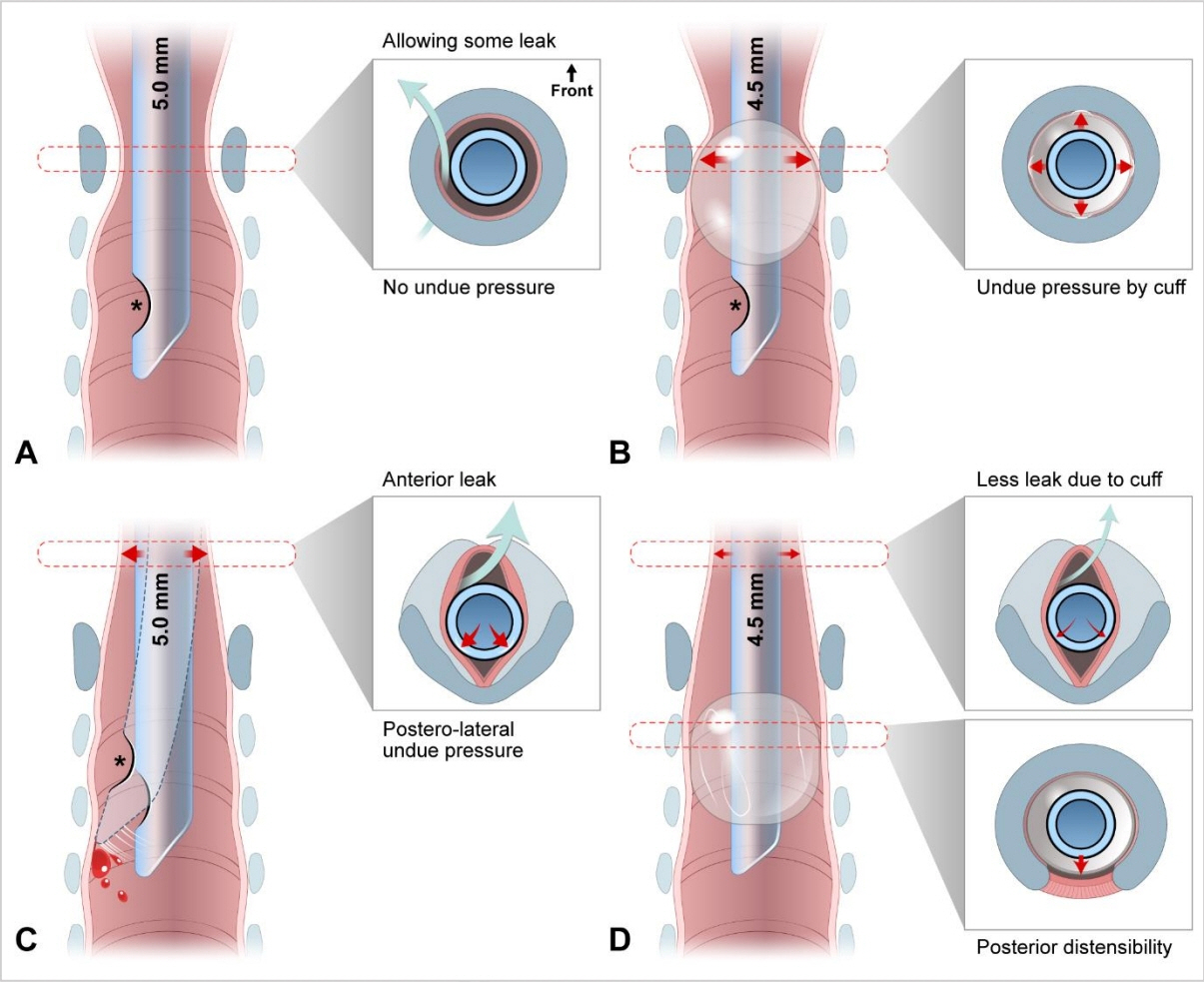
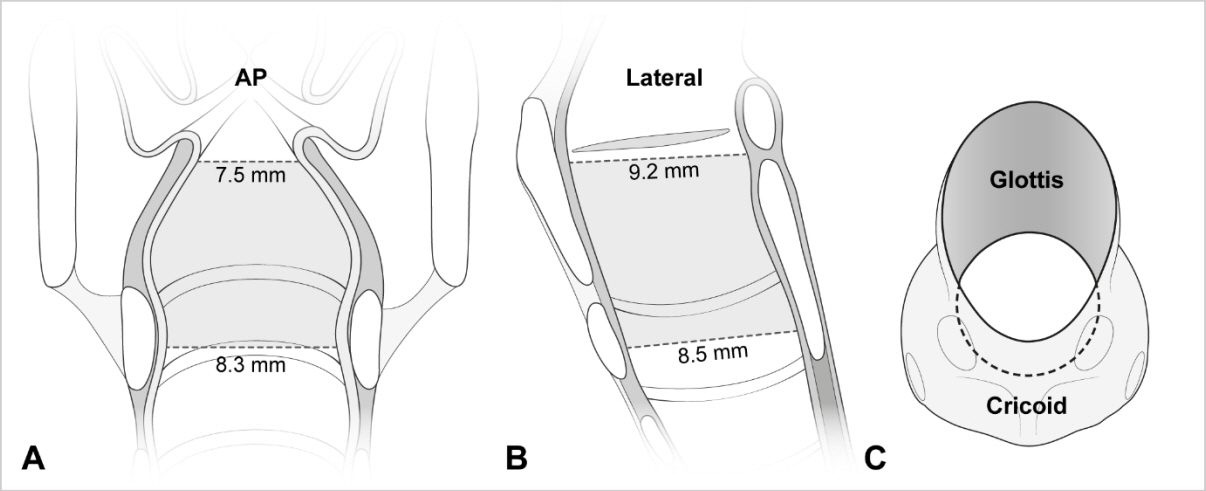
- A young child’s larynx was formerly believed to be narrowest at the cricoid level, circular in section, and funnel shaped. This supported the routine use of uncuffed endotracheal tubes in young children despite the benefits of cuffed tubes, such as lower risk for air leakage and aspiration. In the late 1990s, evidence supporting the pediatric use of cuffed tubes emerged largely from anesthesiology studies, while some technical flaws of the tubes remained a concern. Since the 2000s, imaging-based studies have clarified laryngeal anatomy, revealing that it is narrowest at the glottis, elliptical in section, and cylindrical in shape. The update was contemporaneous with technical advances in the design, size, and material of cuffed tubes. The American Heart Association currently recommends the pediatric use of cuffed tubes. In this review, we present the rationale for using cuffed tubes in young children based on our updated knowledge of pediatric anatomy and technical advances.
Keyword
Figure
Reference
-
References
1. Weiss M, Dullenkopf A. Cuffed tracheal tubes in children: past, present and future. Expert Rev Med Devices. 2007; 4:73–82.
Article2. Tobias JD. Pediatric airway anatomy may not be what we thought: implications for clinical practice and the use of cuffed endotracheal tubes. Paediatr Anaesth. 2015; 25:9–19.
Article3. De Orange FA, Andrade RG, Lemos A, Borges PS, Figueiroa JN, Kovatsis PG. Cuffed versus uncuffed endotracheal tubes for general anaesthesia in children aged eight years and under. Cochrane Database Syst Rev. 2017; 11:CD011954.
Article4. Shah A, Carlisle JB. Cuffed tracheal tubes: guilty now proven innocent. Anaesthesia. 2019; 74:1186–90.
Article5. Bhardwaj N. Pediatric cuffed endotracheal tubes. J Anaesthesiol Clin Pharmacol. 2013; 29:13–8.
Article6. Thomas J, Weiss M, Cannizzaro V, Both CP, Schmidt AR. Work of breathing for cuffed and uncuffed pediatric endotracheal tubes in an in vitro lung model setting. Paediatr Anaesth. 2018; 28:780–7.7. Miller MA, Arndt JL, Konkle MA, Chenoweth CE, Iwashyna TJ, Flaherty KR, et al. A polyurethane cuffed endotracheal tube is associated with decreased rates of ventilator-associated pneumonia. J Crit Care. 2011; 26:280–6.
Article8. Dullenkopf A, Gerber AC, Weiss M. Fit and seal characteristics of a new paediatric tracheal tube with high volume-low pressure polyurethane cuff. Acta Anaesthesiol Scand. 2005; 49:232–7.
Article9. Topjian AA, Raymond TT, Atkins D, Chan M, Duff JP, Joyner BL Jr, et al. Part 4: Pediatric Basic And Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020; 142(16 Suppl 2):S469–523.
Article10. Van de Voorde P, Turner NM, Djakow J, de Lucas N, Martinez-Mejias A, Biarent D, et al. European Resuscitation Council Guidelines 2021: Paediatric Life Support. Resuscitation. 2021; 161:327–87.
Article11. Klabusayova E, Klucka J, Kratochvil M, Musilova T, Vafek V, Skrisovska T, et al. Airway management in pediatric patients: cuff-solved problem? Children (Basel). 2022; 9:1490.
Article12. Clements RS, Steel AG, Bates AT, Mackenzie R. Cuffed endotracheal tube use in paediatric prehospital intubation: challenging the doctrine? Emerg Med J. 2007; 24:57–8.
Article13. Miller KA, Nagler J. Advances in emergent airway management in pediatrics. Emerg Med Clin North Am. 2019; 37:473–91.
Article14. Bayeux R. Laryngeal intubation in croup [Tubage du larynx dans le croup]. Presse Medicale. 1897; 6:29–33.15. Eckenhoff JE. Some anatomic considerations of the infant larynx influencing endotracheal anesthesia. Anesthesiology. 1951; 12:401–10.
Article16. Litman RS, Weissend EE, Shibata D, Westesson PL. Developmental changes of laryngeal dimensions in unparalyzed, sedated children. Anesthesiology. 2003; 98:41–5.
Article17. Dalal PG, Murray D, Messner AH, Feng A, McAllister J, Molter D. Pediatric laryngeal dimensions: an age-based analysis. Anesth Analg. 2009; 108:1475–9.
Article18. Wani TM, Bissonnette B, Rafiq Malik M, Hayes D Jr, Ramesh AS, Al Sohaibani M, et al. Age-based analysis of pediatric upper airway dimensions using computed tomography imaging. Pediatr Pulmonol. 2016; 51:267–71.
Article19. Mizuguchi S, Motomura Y, Maki J, Baba R, Ichimiya Y, Tokuda K, et al. Tracheal size and morphology on the reconstructed CT imaging. Pediatr Crit Care Med. 2019; 20:e366–71.
Article20. Kim Y, Park JE, Kim JH. Plain radiographic analysis of laryngeal dimensions in young children: normal versus croup. Children (Basel). 2022; 9:1532.
Article21. Holzki J, Brown KA, Carroll RG, Cote CJ. The anatomy of the pediatric airway: has our knowledge changed in 120 years?: a review of historic and recent investigations of the anatomy of the pediatric larynx. Paediatr Anaesth. 2018; 28:13–22.
Article22. Holzki JF, Laschat M, Puder C. The pediatric larynx: a complicated organ. Anesth Analg. 2010; 110:1509–10.23. Eckel HE, Koebke J, Sittel C, Sprinzl GM, Pototschnig C, Stennert E. Morphology of the human larynx during the first five years of life studied on whole organ serial sections. Ann Otol Rhinol Laryngol. 1999; 108:232–8.
Article24. Wani TM, Rafiq M, Talpur S, Soualmi L, Tobias JD. Pediatric upper airway dimensions using three-dimensional computed tomography imaging. Paediatr Anaesth. 2017; 27:604–8.25. Benjamin B. Prolonged intubation injuries of the larynx: endoscopic diagnosis, classification, and treatment. Ann Otol Rhinol Laryngol Suppl. 1993; 160:1–15.
Article26. Reidenbach MM, Schmidt HM. Anatomical aspects of postintubational subglottic stenosis. Clin Anat. 1995; 8:273–80.
Article27. Sharma GK, Ahuja GS, Wiedmann M, Osann KE, Su E, Heidari AE, et al. Long-range optical coherence tomography of the neonatal upper airway for early diagnosis of intubation-related subglottic injury. Am J Respir Crit Care Med. 2015; 192:1504–13.
Article28. Lambercy K, Pincet L, Sandu K. Intubation related laryngeal injuries in pediatric population. Front Pediatr. 2021; 9:594832.
Article29. Darras KE, Roston AT, Yewchuk LK. Imaging acute airway obstruction in infants and children. Radiographics. 2015; 35:2064–79.
Article30. Fine GF, Borland LM. The future of the cuffed endotracheal tube. Paediatr Anaesth. 2004; 14:38–42.31. Orliaguet GA, Renaud E, Lejay M, Meyer PG, Schmautz E, Telion C, et al. Postal survey of cuffed or uncuffed tracheal tubes used for paediatric tracheal intubation. Paediatr Anaesth. 2001; 11:277–81.
Article32. Motoyama EK. The shape of the pediatric larynx: cylindrical or funnel shaped? Anesth Analg. 2009; 108:1379–81.
Article33. Khine HH, Corddry DH, Kettrick RG, Martin TM, McCloskey JJ, Rose JB, et al. Comparison of cuffed and uncuffed endotracheal tubes in young children during general anesthesia. Anesthesiology. 1997; 86:627–31.
Article34. Weiss M, Dullenkopf A, Fischer JE, Keller C, Gerber AC; European Paediatric Endotracheal Intubation Study Group. Prospective randomized controlled multi-centre trial of cuffed or uncuffed endotracheal tubes in small children. Br J Anaesth. 2009; 103:867–73.
Article35. Taylor C, Subaiya L, Corsino D. Pediatric cuffed endotracheal tubes: an evolution of care. Ochsner J. 2011; 11:52–6.36. Calder A, Hegarty M, Erb TO, von Ungern-Sternberg BS. Predictors of postoperative sore throat in intubated children. Paediatr Anaesth. 2012; 22:239–43.
Article37. Chambers NA, Ramgolam A, Sommerfield D, Zhang G, Ledowski T, Thurm M, et al. Cuffed vs. uncuffed tracheal tubes in children: a randomised controlled trial comparing leak, tidal volume and complications. Anaesthesia. 2018; 73:160–8.
Article38. El-Boghdadly K, Bailey CR, Wiles MD. Postoperative sore throat: a systematic review. Anaesthesia. 2016; 71:706–17.
Article39. Flynn PE, Black AE, Mitchell V. The use of cuffed tracheal tubes for paediatric tracheal intubation, a survey of specialist practice in the United Kingdom. Eur J Anaesthesiol. 2008; 25:685–8.
Article40. James I. Cuffed tubes in children. Paediatr Anaesth. 2001; 11:259–63.
Article41. Thomas R, Rao S, Minutillo C. Cuffed endotracheal tubes for neonates and young infants: a comprehensive review. Arch Dis Child Fetal Neonatal Ed. 2016; 101:F168–74.
Article42. Krishna SG, Hakim M, Sebastian R, Dellinger HL, Tumin D, Tobias JD. Cuffed endotracheal tubes in children: the effect of the size of the cuffed endotracheal tube on intracuff pressure. Paediatr Anaesth. 2017; 27:494–500.
Article43. Ho AM, Aun CS, Karmakar MK. The margin of safety associated with the use of cuffed paediatric tracheal tubes. Anaesthesia. 2002; 57:173–5.
Article44. Weiss M, Dullenkopf A, Gysin C, Dillier CM, Gerber AC. Shortcomings of cuffed paediatric tracheal tubes. Br J Anaesth. 2004; 92:78–88.45. Dave MH, Frotzler A, Spielmann N, Madjdpour C, Weiss M. Effect of tracheal tube cuff shape on fluid leakage across the cuff: an in vitro study. Br J Anaesth. 2010; 105:538–43.
Article46. Guyton D, Banner MJ, Kirby RR. High-volume, low-pressure cuffs: are they always low pressure? Chest. 1991; 100:1076–81.47. Felten ML, Schmautz E, Delaporte-Cerceau S, Orliaguet GA, Carli PA. Endotracheal tube cuff pressure is unpredictable in children. Anesth Analg. 2003; 97:1612–6.
Article48. Cox RG. Should cuffed endotracheal tubes be used routinely in children? Can J Anaesth. 2005; 52:669–74.
Article49. Dullenkopf A, Gerber A, Weiss M. Fluid leakage past tracheal tube cuffs: evaluation of the new Microcuff endotracheal tube. Intensive Care Med. 2003; 29:1849–53.
Article50. Fischer M, Grass B, Kemper M, Weiss M, Dave MH. Cuffed pediatric endotracheal tubes: outer cuff diameters compared to age-related airway dimensions. Paediatr Anaesth. 2020; 30:424–34.51. Dullenkopf A, Schmitz A, Gerber AC, Weiss M. Tracheal sealing characteristics of pediatric cuffed tracheal tubes. Paediatr Anaesth. 2004; 14:825–30.
Article52. Mariyaselvam MZ, Marsh LL, Bamford S, Smith A, Wise MP, Williams DW. Endotracheal tubes and fluid aspiration: an in vitro evaluation of new cuff technologies. BMC Anesthesiol. 2017; 17:36.
Article53. Boerboom SL, Muthukrishnan SM, de Graaff JC, Jonker G. Cuffed or uncuffed endotracheal tubes in pediatric anesthesia: a survey of current practice in the United Kingdom and The Netherlands. Paediatr Anaesth. 2015; 25:431–2.
Article54. Sathyamoorthy M, Lerman J, Okhomina VI, Penman AD. Use of cuffed tracheal tubes in neonates, infants and children: a practice survey of members of the Society of Pediatric Anesthesia. J Clin Anesth. 2016; 33:266–72.
Article55. Shaffner DH, McCloskey JJ, Schwartz JM. Cuffed endotracheal tube use in children: times (and minds) are ‘a changing. Pediatr Crit Care Med. 2019; 20:789–90.56. Hansen ML, Eriksson C. Intubation and ventilation of infants and children. In : Tintinalli JE, Ma OJ, Yealy DM, Meckler GD, Stapczynski JS, Cline DM, editors. Tintinalli's emergency medicine: a comprehensive study guide. 9th ed. New York: McGraw-Hill Education;2020. p. 710–9.57. Nagler J, Mick NW. Airway management for the pediatric patient. In : Walls RM, Hockberger RS, Gausche-Hill M, Bakes K, Baren JM, Erickson TB, editors. Rosen's emergency medicine: cencepts and clinical practice. 9th ed. Philadelphia (PA): Elsevier;2018. p. 1994–2004.58. Nagler J, Donoghue AJ, Yamamoto LG. Airway. In : Shaw KN, Bachur RG, Chamberlain J, Lavelle J, Nagler J, Shook JE, editors. Fleisher and Ludwig’s textbook of pediatric emergency medicine. 8th ed. Philadelphia (PA): Wolters Kluwer;2021. p. 34–42.59. Hartman ME, Cheifetz IM. Pediatric emergencies and resuscitation. In : Kliegman RM, St Geme III JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, editors. Nelson textbook of pediatrics. 21th ed. Philadelphia (PA): Elsevier;2020. p. 530–47.60. Schneider J, Mulale U, Yamout S, Pollard S, Silver P. Impact of monitoring endotracheal tube cuff leak pressure on postextubation stridor in children. J Crit Care. 2016; 36:173–7.
Article61. Al-Metwalli RR, Al-Ghamdi AA, Mowafi HA, Sadek S, Abdulshafi M, Mousa WF. Is sealing cuff pressure, easy, reliable and safe technique for endotracheal tube cuff inflation?: a comparative study. Saudi J Anaesth. 2011; 5:185–9.
Article62. Manimalethu R, Krishna S, Shafy SZ, Hakim M, Tobias JD. Choosing endotracheal tube size in children: which formula is best? Int J Pediatr Otorhinolaryngol. 2020; 134:110016.
Article63. Bernet V, Dullenkopf A, Maino P, Weiss M. Outer diameter and shape of paediatric tracheal tube cuffs at higher inflation pressures. Anaesthesia. 2005; 60:1123–8.
Article64. Sathyamoorthy M, Lerman J, Asariparampil R, Penman AD, Lakshminrusimha S. Stridor in neonates after using the microcuff(R) and uncuffed tracheal tubes: a retrospective review. Anesth Analg. 2015; 121:1321–4.65. Sathyamoorthy M, Lerman J, Lakshminrusimha S, Feldman D. Inspiratory stridor after tracheal intubation with a MicroCuff(R) tracheal tube in three young infants. Anesthesiology. 2013; 118:748–50.66. Zander D, Grass B, Weiss M, Buehler PK, Schmitz A. Cuffed endotracheal tubes in neonates and infants of less than 3 kg body weight: a retrospective audit. Paediatr Anaesth. 2021; 31:604–10.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Survey of Appropriate Cuff Volume and Pressure during General Anesthesia in Pediatric Patients
- Tube-in-tube airway management in a patient with Montgomery T-tube in situ -a case report-
- Oral endotracheal intubation in pediatric anesthesia
- Endotracheal Tube Obstruction due to Mucous Crust after General Anesthesia
- A Case Report of Airway Obstruction with Armored Endotracheal Tube