J Cerebrovasc Endovasc Neurosurg.
2023 Jun;25(2):160-174. 10.7461/jcen.2023.E2022.07.007.
Long-term outcomes of carotid artery stenting in patients with carotid artery stenosis: A single-center 14-year retrospective analysis
- Affiliations
-
- 1Department of Neurosurgery, Soonchunhyang University Cheonan Hospital, Cheonan, Korea
- KMID: 2543512
- DOI: http://doi.org/10.7461/jcen.2023.E2022.07.007
Abstract
Objective
Carotid artery stenting (CAS) is currently widely used for the treatment of carotid artery stenosis. The objective of this study was to analyze the outcomes of CAS performed in a single institution.
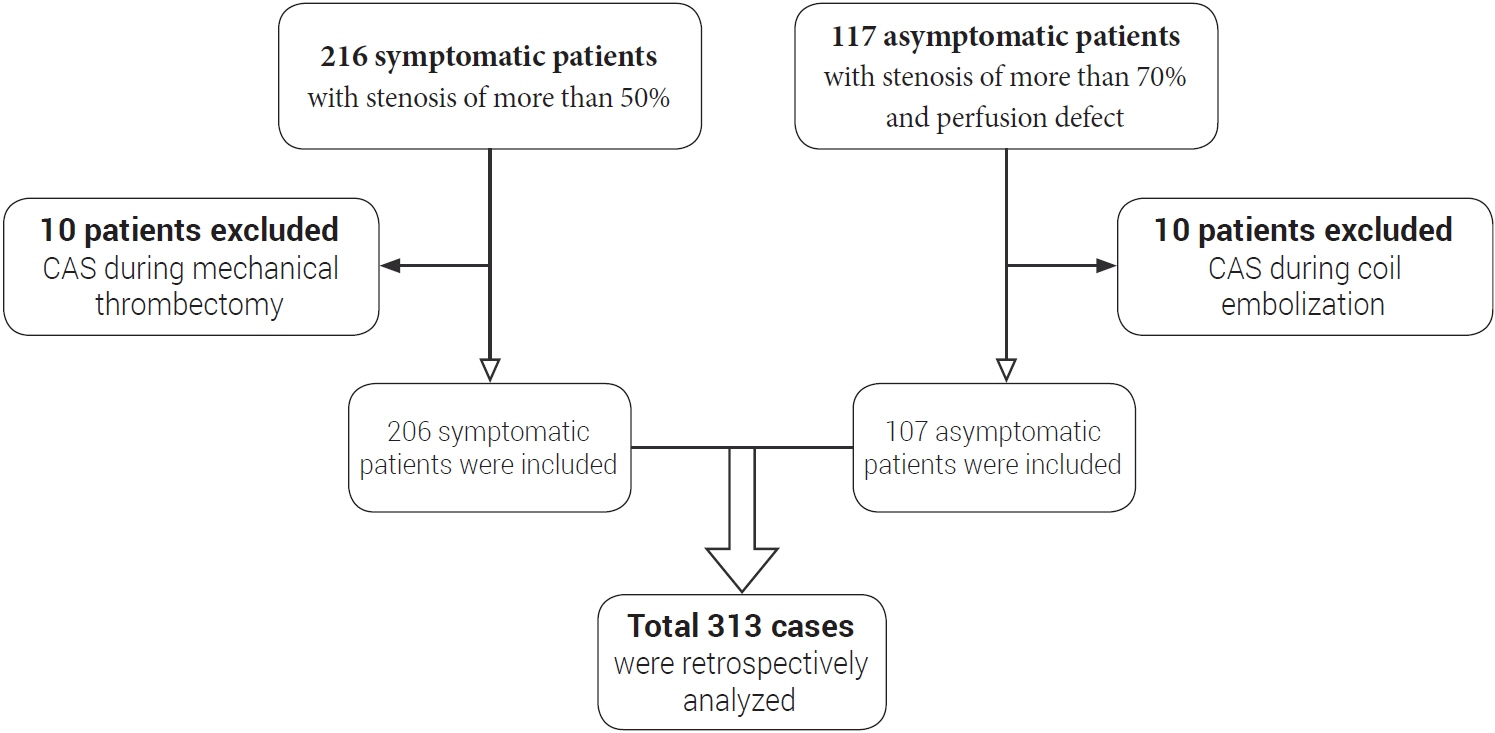
Methods
We retrospectively analyzed 313 CAS cases from January 2007 to December 2020, including 206 (66%) symptomatic and 107 (34%) asymptomatic cases. Procedure-related morbidity and mortality were assessed. Rates of periprocedural (≤30 days after CAS) and postprocedural ipsilateral strokes (>30 days after CAS) were also assessed. Logistic regression analysis was used to identify risk factors for the periprocedural complication, in-stent restenosis (ISR), and ipsilateral stroke.
Results
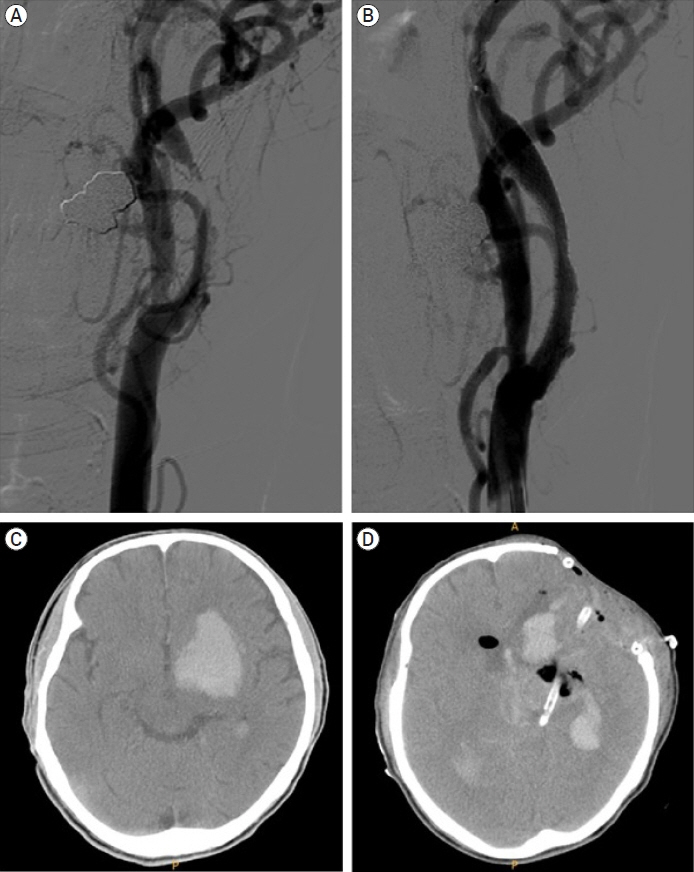
The success rate of CAS was 98%. Among 313 cases, 1 patient died due to hyperperfusion-related intracerebral hemorrhage (ICH). The CAS-related mortality rate was 0.31%. The overall incidence of periprocedural complications is 5.1%. A risk factor for periprocedural complication was a symptomatic carotid artery stenosis (7.3% vs. 0.9%, p=0.016). Twenty cases of ISR occurred during 63.7±42.1 months of follow-up. The overall incidence of ISR was 10.2% (20/196). A risk factors for ISR were diabetes mellitus (17.6% vs. 5.7%, p=0.008) and patients who used Open-cell stents (19.6% vs. 6.9%, p=0.010). The overall incidence of ipsilateral stroke is 5.6%. A risk factors for ipsilateral stroke was ISR (95% CI, p=0.002).
Conclusions
CAS is a safe and effective procedure for carotid artery stenosis. Although the incidence of complications is low, fatal complication such as hyperperfusion- related ICH can occur. To prevent hyperperfusion-related ICH, several methods such as strict blood pressure (BP) control, intentional less widening of stenotic segment should be used. To prevent ISR or stroke occurrence, special attention should be paid to patients who have ISR or ipsilateral stroke risk factors.
Keyword
Figure
Reference
-
1. Abou-Chebl A, Yadav JS, Reginelli JP, Bajzer C, Bhatt D, Krieger DW. Intracranial hemorrhage and hyperperfusion syndrome following carotid artery stenting: risk factors, prevention, and treatment. J Am Coll Cardiol. 2004; May. 43(9):1596–601.2. AbuRahma AF, Abu-Halimah S, Hass SM, Nanjundappa A, Stone PA, Mousa A, et al. Carotid artery stenting outcomes are equivalent to carotid endarterectomy outcomes for patients with post-carotid endarterectomy stenosis. J Vasc Surg. 2010; Nov. 52(5):1180–7.3. AbuRahma AF, AbuRahma ZT, Santini A, Beasley M, Davis M, Lee A, et al. A single-center experience of 30-day perioperative and one year clinical outcomes of transcarotid artery revascularization in 100 consecutive patients. Vascular. 2022; May. 17085381221106330.
Article4. Bonati LH, Dobson J, Featherstone RL, Ederle J, van der Worp HB, de Borst GJ, et al. Long-term outcomes after stenting versus endarterectomy for treatment of symptomatic carotid stenosis: the International Carotid Stenting Study (ICSS) randomised trial. Lancet. 2015; Feb. 385(9967):529–38.
Article5. Bosiers M, de Donato G, Deloose K, Verbist J, Peeters P, Castriota F, et al. Does free cell area influence the outcome in carotid artery stenting? Eur J Vasc Endovasc Surg. 2007; Feb. 33(2):135–41. discussion 42-3.
Article6. Brott TG, Howard G, Roubin GS, Meschia JF, Mackey A, Brooks W, et al. Long-term results of stenting versus endarterectomy for carotid-artery stenosis. N Engl J Med. 2016; Mar. 374(11):1021–31.
Article7. Chakhtoura EY, Hobson RW 2nd, Goldstein J, Simonian GT, Lal BK, Haser PB, et al. In-stent restenosis after carotid angioplasty-stenting: incidence and management. J Vasc Surg. 2001; Feb. 33(2):220–5. discussion 225-6.
Article8. Diyora B, Chheda RM, Dhall G, Gupta P, Dewani K, Mulla M, et al. Carotid endarterectomy and carotid artery stenting for symptomatic carotid stenosis: an experience of a hybrid neurosurgeon in a developing nation. Neurol India. 2022; JanFeb. 70(1):94–101.
Article9. Doig D, Turner EL, Dobson J, Featherstone RL, Lo RT, Gaines PA, et al. Predictors of stroke, myocardial infarction or death within 30 days of carotid artery stenting: results from the international carotid stenting study. Eur J Vasc Endovasc Surg. 2016; Mar. 51(3):327–34.
Article10. Eckstein HH. European society for vascular surgery guidelines on the management of atherosclerotic carotid and vertebral artery disease. Eur J Vasc Endovasc Surg. 2018; Jan. 55(1):1–2.
Article11. Fanelli F, Boatta E, Cannavale A, Corona M, Lucatelli P, Wlderk A, et al. Carotid artery stenting: analysis of a 12-year singlecenter experience. J Endovasc Ther. 2012; Dec. 19(6):749–56.
Article12. Farooq MU, Goshgarian C, Min J, Gorelick PB. Pathophysiology and management of reperfusion injury and hyperperfusion syndrome after carotid endarterectomy and carotid artery stenting. Exp Transl Stroke Med. 2016; Sep. 8(1):7.13. Furie KL, Kasner SE, Adams RJ, Albers GW, Bush RL, Fagan SC, et al. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011; Jan. 42(1):227–76.
Article14. Gensicke H, van der Worp HB, Nederkoorn PJ, Macdonald S, Gaines PA, van der Lugt A, et al. Ischemic brain lesions after carotid artery stenting increase future cerebrovascular risk. J Am Coll Cardiol. 2015; Feb. 65(6):521–9.15. Gorgulu S, Sahin M, Norgaz NT, Pala S, Sari M, Yalcin AA, et al. Carotid artery stenting without embolic protection: A randomized multicenter trial (the CASWEP trial). Interv Neuroradiol. 2022; Apr. 15910199221094388.
Article16. Hobson RW 2nd, Mackey WC, Ascher E, Murad MH, Calligaro KD, Comerota AJ, et al. Management of atherosclerotic carotid artery disease: clinical practice guidelines of the Society for Vascular Surgery. J Vasc Surg. 2008; Aug. 48(2):480–6.
Article17. Hunter GC. Edgar J. Poth Memorial/W.L. Gore and Associates, Inc. Lectureship. The clinical and pathological spectrum of recurrent carotid stenosis. Am J Surg. 1997; Dec. 174(6):583–8.18. Jansen C, Sprengers AM, Moll FL, Vermeulen FE, Hamerlijnck RP, van Gijn J, et al. Prediction of intracerebral haemorrhage after carotid endarterectomy by clinical criteria and intraoperative transcranial Doppler monitoring. Eur J Vasc Surg. 1994; May. 8(3):303–8.
Article19. Jansen O, Fiehler J, Hartmann M, Bruckmann H. Protection or nonprotection in carotid stent angioplasty: the influence of interventional techniques on outcome data from the SPACE Trial. Stroke. 2009; Mar. 40(3):841–6.20. Kashiwazaki D, Kuwayama N, Akioka N, Noguchi K, Kuroda S. Carotid plaque with expansive arterial remodeling is a risk factor for ischemic complication following carotid artery stenting. Acta Neurochir (Wien). 2017; Jul. 159(7):1299–304.
Article21. Kim NY, Choi JW, Whang K, Cho SM, Koo YM, Kim JY. Neurologic complications in patients with carotid artery stenting. J Cerebrovasc Endovasc Neurosurg. 2019; Jun. 21(2):86–93.
Article22. Koklu E, Arslan S, Sarionder Gencer E, Bayar N, Avci R, Ozgunoglu EC. Six-year outcomes of carotid artery stenting performed with multidisciplinary management in a single center. Anatol J Cardiol. 2021; Jun. 25(6):385–94.23. Koklu E, Arslan S, Sarionder Gencer E, Bayar N, Ureyen CM, Erkal Z, et al. Asymptomatic cerebral emboli following carotid artery stenting: a diffusion-weighted MRI study. Anatol J Cardiol. 2022; Apr. 26(4):298–304.
Article24. Lal BK, Beach KW, Roubin GS, Lutsep HL, Moore WS, Malas MB, et al. Restenosis after carotid artery stenting and endarterectomy: a secondary analysis of CREST, a randomised controlled trial. Lancet Neurol. 2012; Sep. 11(9):755–63.
Article25. Lal BK, Hobson RW 2nd, Goldstein J, Geohagan M, Chakhtoura E, Pappas PJ, et al. In-stent recurrent stenosis after carotid artery stenting: life table analysis and clinical relevance. J Vasc Surg. 2003; Dec. 38(6):11162–8. discussion 1169.
Article26. Macfarlane R, Moskowitz MA, Sakas DE, Tasdemiroglu E, Wei EP, Kontos HA. The role of neuroeffector mechanisms in cerebral hyperperfusion syndromes. J Neurosurg. 1991; Dec. 75(6):845–55.27. Megaly M, Alani F, Cheng CI, Ragina N. Risk factors for the development of carotid artery in-stent restenosis: multivariable analysis. Cardiovasc Revasc Med. 2021; Mar. 24:65–9.
Article28. Miyachi S. Carotid angioplasty and stenting for occlusive diseases. Adv Tech Stand Neurosurg. 2022; 44:209–23.29. Mo D, Luo G, Wang B, Ma N, Gao F, Sun X, et al. Staged carotid artery angioplasty and stenting for patients with high-grade carotid stenosis with high risk of developing hyperperfusion injury: a retrospective analysis of 44 cases. Stroke Vasc Neurol. 2016; Dec. 1(4):147–53.
Article30. Montorsi P, Galli S, Teruzzi G, Troiano S, Caputi L, Gili S, et al. Case report: a cluster of complications during carotid artery stenting managed with peripheral, coronary, and imaging techniques. Front Cardiovasc Med. 2021; Sep. 8:712963.
Article31. Moore WS, Kempczinski RF, Nelson JJ, Toole JF. Recurrent carotid stenosis: results of the asymptomatic carotid atherosclerosis study. Stroke. 1998; Oct. 29(10):2018–25.32. Ogasawara K, Sakai N, Kuroiwa T, Hosoda K, Iihara K, Toyoda K, et al. Intracranial hemorrhage associated with cerebral hyperperfusion syndrome following carotid endarterectomy and carotid artery stenting: retrospective review of 4494 patients. J Neurosurg. 2007; Dec. 107(6):1130–6.
Article33. Ogasawara K, Yukawa H, Kobayashi M, Mikami C, Konno H, Terasaki K, et al. Prediction and monitoring of cerebral hyperperfusion after carotid endarterectomy by using single-photon emission computerized tomography scanning. J Neurosurg. 2003; Sep. 99(3):504–10.
Article34. Ouriel K, Shortell CK, Illig KA, Greenberg RK, Green RM. Intracerebral hemorrhage after carotid endarterectomy: incidence, contribution to neurologic morbidity, and predictive factors. J Vasc Surg. 1999; Jan. 29(1):82–7. discussion 87-9.
Article35. Pendlebury ST, Rothwell PM. Prevalence, incidence, and factors associated with pre-stroke and post-stroke dementia: a systematic review and meta-analysis. Lancet Neurol. 2009; Nov. 8(11):1006–18.
Article36. Reimers B, Corvaja N, Moshiri S, Sacca S, Albiero R, Di Mario C, et al. Cerebral protection with filter devices during carotid artery stenting. Circulation. 2001; Jul. 104(1):12–5.
Article37. Setacci C, de Donato G, Setacci F, Pieraccini M, Cappelli A, Trovato RA, et al. In-stent restenosis after carotid angioplasty and stenting: a challenge for the vascular surgeon. Eur J Vasc Endovasc Surg. 2005; Jun. 29(6):601–7.38. Shahidi S, Owen-Falkenberg A, Gottschalksen B, Ellemann K. Risk of early recurrent stroke in symptomatic carotid stenosis after best medical therapy and before endarterectomy. Int J Stroke. 2016; Jan. 11(1):41–51.
Article39. Simonetti G, Gandini R, Versaci F, Pampana E, Fabiano S, Stefanini M, et al. Carotid artery stenting: findings based on 8 years’ experience. Radiol Med. 2009; Feb. 114(1):95–110.
Article40. Son S, Choi DS, Kim SK, Kang H, Park KJ, Choi NC, et al. Carotid artery stenting in patients with near occlusion: a single-center experience and comparison with recent studies. Clin Neurol Neurosurg. 2013; Oct. 115(10):1976–81.
Article41. Sprouse LR 2nd, Peeters P, Bosiers M. . The capture of visible debris by distal cerebral protection filters during carotid artery stenting: Is it predictable? J Vasc Surg. 2005; Jun. 41(6):950–5.
Article42. Stilo F, Montelione N, Calandrelli R, Distefano M, Spinelli F, Di Lazzaro V, et al. The management of carotid restenosis: a comprehensive review. Ann Transl Med. 2020; Oct. 8(19):1272.43. Stilo F, Sirignano P, Montelione N, Mansour W, Capoccia L, Catanese V, et al. Bypass for symptomatic in-stent carotid restenosis. Int J Cardiol. 2017; Dec. 249:392–5.
Article44. Texakalidis P, Tzoumas A, Giannopoulos S, Jonnalagadda AK, Jabbour P, Rangel-Castilla L, et al. Risk factors for restenosis after carotid revascularization: a meta-analysis of hazard ratios. World Neurosurg. 2019; May. 125:414–24.
Article45. Trisal V, Paulson T, Hans SS, Mittal V. Carotid artery restenosis: an ongoing disease process. Am Surg. 2002; Mar. 68(3):275–9. discussion 279-80.
Article46. Tsai CH, Chen YH, Lin MS, Huang CC, Hung CS, Yeh CF, et al. The periprocedural and 30-day outcomes of carotid stenting in patients with carotid artery near-occlusion. Sci Rep. 2021; Nov. 11(1):21876.
Article47. Willfort-Ehringer A, Ahmadi R, Gessl A, Gschwandtner ME, Haumer A, Lang W, et al. Neointimal proliferation within carotid stents is more pronounced in diabetic patients with initial poor glycaemic state. Diabetologia. 2004; Mar. 47(3):400–6.
Article48. Willfort-Ehringer A, Ahmadi R, Gruber D, Gschwandtner ME, Haumer A, Haumer M, et al. Arterial remodeling and hemodynamics in carotid stents: a prospective duplex ultrasound study over 2 years. J Vasc Surg. 2004; Apr. 39(4):728–34.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Transseptal Approach to Carotid Artery Stenting in Right Internal Carotid Stenosis
- Carotid Artery Stenting
- Recurrent Carotid Artery Stenosis
- Carotid artery stenting in patients with symptomatic coronary artery disease
- Stenting for Symptomatic Vertebral Artery Stenosis Associated with Bilateral Carotid Rete Mirabile: The Long-Term Clinical and Angiographic Outcome