Neurointervention.
2023 Jul;18(2):135-139. 10.5469/neuroint.2023.00150.
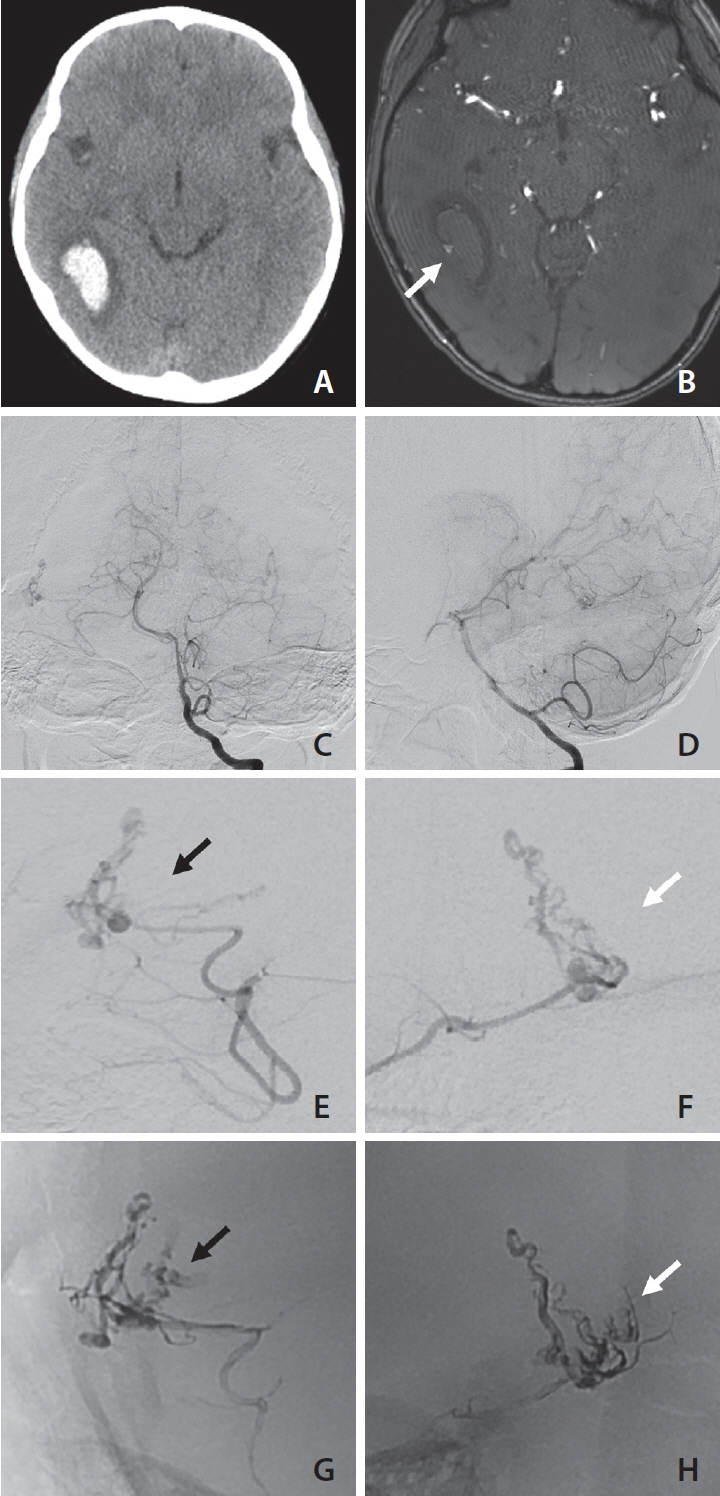
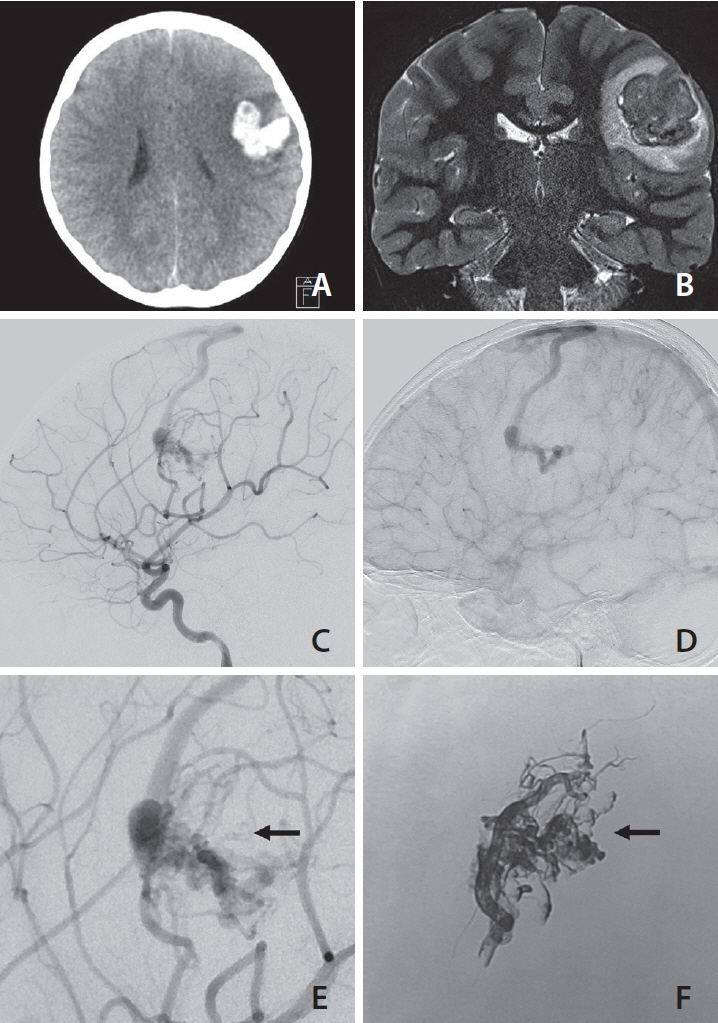
Obscured Segments of Ruptured Brain Arteriovenous Malformations: Insights from Their Visualization during Emergency Transarterial Embolization
- Affiliations
-
- 1Department of Radiology, Pusan National University Yangsan Hospital, Yangsan, Korea
- 2Department of Neurosurgery, Pusan National University Yangsan Hospital, Yangsan, Korea
- KMID: 2543369
- DOI: http://doi.org/10.5469/neuroint.2023.00150
Abstract
- A ruptured brain arteriovenous malformation (bAVM) presenting with a hematoma may have unseen parts of the shunts in diagnostic angiography in the acute phase, which may lead to innate incomplete evaluation for the whole angioarchitecture of the bAVM. Even though it is generally accepted that the nidus of a ruptured bAVM may be underestimated in angiography during the acute phase due to hematoma compression, documentation of the underestimated parts has not been described in the literature. The authors report 2 cases of ruptured bAVMs in which the obscured segments were cast with liquid embolic material, which suggests a potential presence of obscured segments in bAVMs.
Figure
Reference
-
1. Iosif C, Mendes GA, Saleme S, Ponomarjova S, Silveira EP, Caire F, et al. Endovascular transvenous cure for ruptured brain arteriovenous malformations in complex cases with high Spetzler-Martin grades. J Neurosurg. 2015; 122:1229–1238.
Article2. Mansur A, Kostynskyy A, Krings T, Agid R, Radovanovic I, Mendes Pereira V. The safety profile and angioarchitectural changes after acute targeted embolization of ruptured arteriovenous malformations. J Neurosurg. 2021; 135:1598–1607.
Article3. Signorelli F, Gory B, Pelissou-Guyotat I, Guyotat J, Riva R, Dailler F, et al. Ruptured brain arteriovenous malformations associated with aneurysms: safety and efficacy of selective embolization in the acute phase of hemorrhage. Neuroradiology. 2014; 56:763–769.
Article4. van Rooij WJ, Jacobs S, Sluzewski M, Beute GN, van der Pol B. Endovascular treatment of ruptured brain AVMs in the acute phase of hemorrhage. AJNR Am J Neuroradiol. 2012; 33:1162–1166.
Article5. Alexander MD, Cooke DL, Hallam DK, Kim H, Hetts SW, Ghodke BV. Less can be more: targeted embolization of aneurysms associated with arteriovenous malformations unsuitable for surgical resection. Interv Neuroradiol. 2016; 22:445–451.
Article6. Jin H, Lenck S, Krings T, Agid R, Fang Y, Li Y, et al. Interval angioarchitectural evolution of brain arteriovenous malformations following rupture. J Neurosurg. 2018; 131:96–103.
Article7. Pellettieri L, Svendsen P, Wikholm G, Carlsson CA. Hidden compartments in AVMs--a new concept. Acta Radiol. 1997; 38:2–7.8. Yamada S, Brauer FS, Colohan AR, Won DJ, Siddiqi J, Johnson WD, et al. Concept of arteriovenous malformation compartments and surgical management. Neurol Res. 2004; 26:288–300.
Article9. Kader A, Goodrich JT, Sonstein WJ, Stein BM, Carmel PW, Michelsen WJ. Recurrent cerebral arteriovenous malformations after negative postoperative angiograms. J Neurosurg. 1996; 85:14–18.
Article10. Copelan A, Drocton G, Caton MT, Smith ER, Cooke DL, Nelson J, UCSF Center For Cerebrovascular Research and UCSF Pediatric Brain Center, et al. Brain arteriovenous malformation recurrence after apparent microsurgical cure: increased risk in children who present with arteriovenous malformation rupture. Stroke. 2020; 51:2990–2996.
Article11. Ali MJ, Bendok BR, Rosenblatt S, Rose JE, Getch CC, Batjer HH. Recurrence of pediatric cerebral arteriovenous malformations after angiographically documented resection. Pediatr Neurosurg. 2003; 39:32–38.
Article12. Aboukaïs R, Vinchon M, Quidet M, Bourgeois P, Leclerc X, Lejeune JP. Reappearance of arteriovenous malformations after complete resection of ruptured arteriovenous malformations: true recurrence or false-negative early postoperative imaging result? J Neurosurg. 2017; 126:1088–1093.
Article13. Sorenson TJ, Brinjikji W, Bortolotti C, Kaufmann G, Lanzino G. Recurrent brain arteriovenous malformations (AVMs): a systematic review. World Neurosurg. 2018; 116:e856–e866.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of transarterial n-BCA and Onyx embolization of brain arteriovenous malformations: A single-center 18-year retrospective analysis
- Cases of Transarterial embolization in Arteriovenous Malformation of Uterus
- Dural Arteriovenous Fistula Involving Transverse Sinus: Successful Embolization Using Onyx(R)
- Treatment of mandibular arteriovenous malformation by embolization : a case report
- Embolization of brain arteriovenous malformations using Tracker catheter