Kosin Med J.
2023 Jun;38(2):138-143. 10.7180/kmj.22.123.
Sigmoid colon plexiform neurofibroma as a colonic subepithelial mass: a case report
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Inje University Busan Paik Hospital, Inje University College of Medicine, Busan, Korea
- 2Department of Surgery, Inje University Busan Paik Hospital, Inje University College of Medicine, Busan, Korea
- KMID: 2543334
- DOI: http://doi.org/10.7180/kmj.22.123
Abstract
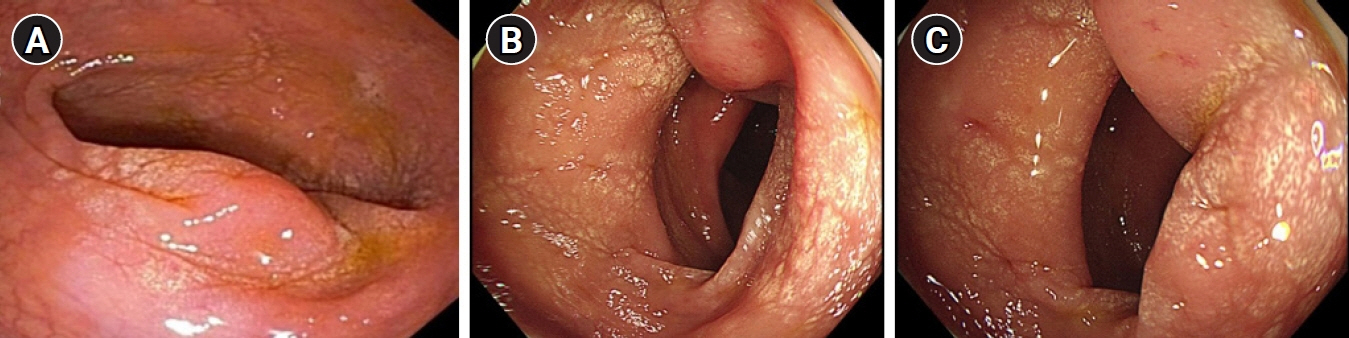
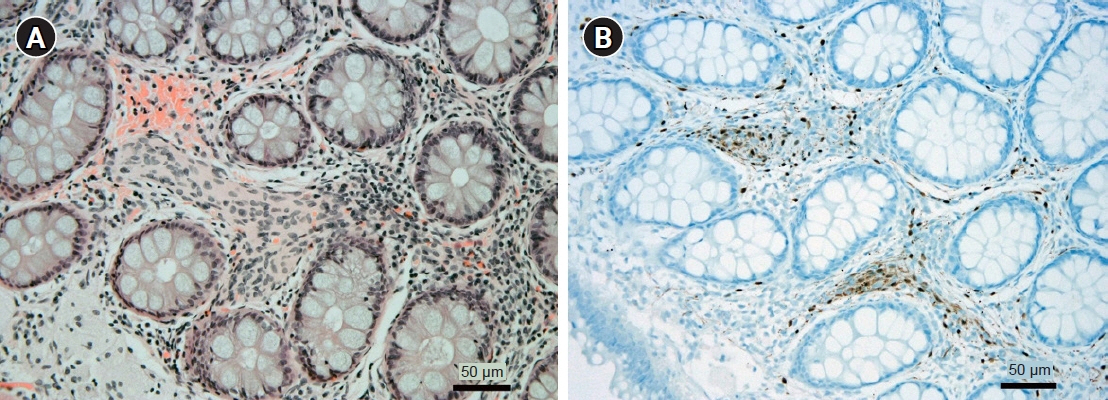
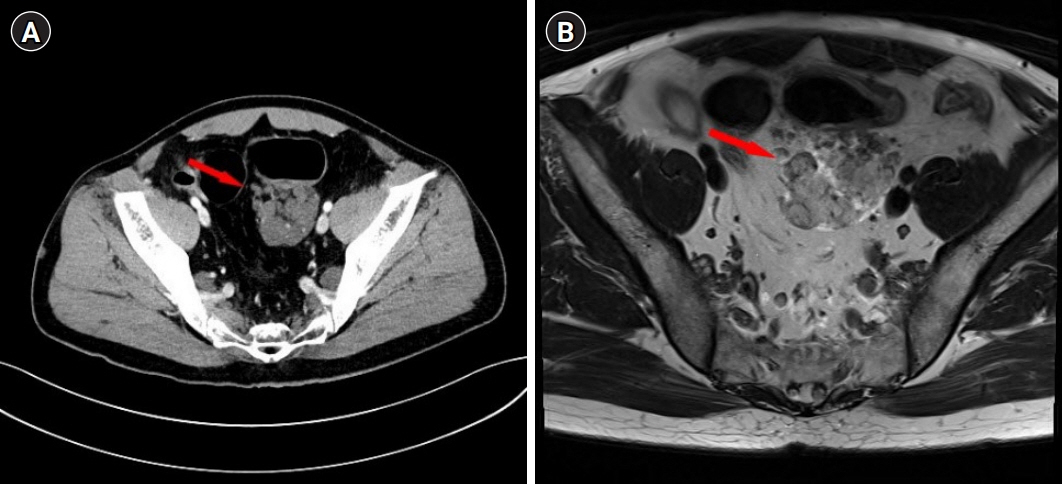
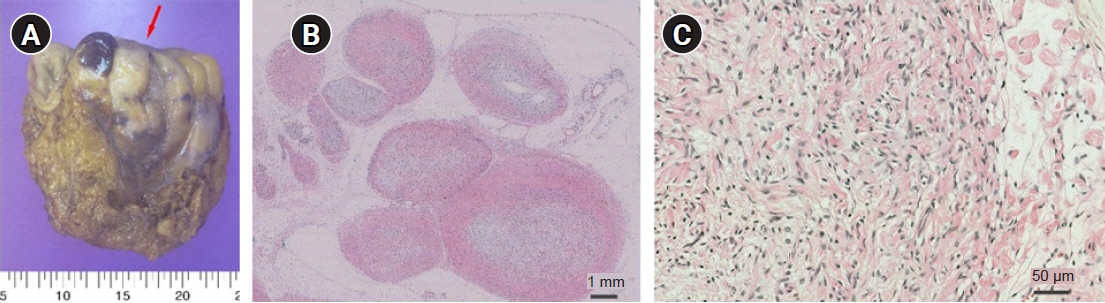
- Plexiform neurofibroma (PN) is an uncommon benign tumor, usually associated with neurofibromatosis type 1. As most PNs involve the craniomaxillofacial region, PN of the colon is very rare. Here we present a case of PN involving the sigmoid colon. A 43-year-old male patient presented to the outpatient clinic for the evaluation of an incidentally discovered sigmoid colon mass. A colonoscopic biopsy was performed for the mass, and the result revealed neuronal proliferation. The patient visited the outpatient clinic a year later with symptoms of abdominal pain and stool caliber change. Biopsy was repeated for the sigmoid colon mass, and the results showed mucosal Schwann cell proliferation and S-100 immunostaining positivity. Computed tomography and magnetic resonance imaging were performed for further evaluation, and neurofibroma or schwannoma was suspected based on the imaging studies. For an accurate diagnosis, the patient underwent surgery to remove the sigmoid colon mass. The final diagnosis of the mass was confirmed as PN. We hereby report a rare case of PN involving the sigmoid colon that could not be diagnosed before surgery.
Figure
Reference
-
References
1. Shi L, Liu FJ, Jia QH, Guan H, Lu ZJ. Solitary plexiform neurofibroma of the stomach: a case report. World J Gastroenterol. 2014; 20:5153–6.2. Wiesen A, Davidoff S, Sideridis K, Greenberg R, Bank S, Falkowski O. Neurofibroma in the colon. J Clin Gastroenterol. 2006; 40:85–6.3. An GH, Jun BY, Jung MH, Jeong HK, Jin JY, Lee KH. A case of plexiform neurofibroma involving the mediastinum and abdomen in a patient with neurofibromatosis. Korean J Med. 2010; 79:443–7.4. Tchernev G, Chokoeva AA, Patterson JW, Bakardzhiev I, Wollina U, Tana C. Plexiform neurofibroma: a case report. Medicine (Baltimore). 2016; 95:e2663.5. Park SJ, Choi SI, Lee SH, Lee KY. Plexiform neurofibroma involving the ascending colonic mesentery in neurofibromatosis type I. J Korean Soc Coloproctol. 2009; 25:259–63.6. Ahn S, Chung CS, Kim KM. Neurofibroma of the colon: a diagnostic mimicker of gastrointestinal stromal tumor. Case Rep Gastroenterol. 2016; 10:674–8.7. Dare AJ, Gupta AA, Thipphavong S, Miettinen M, Gladdy RA. Abdominal neoplastic manifestations of neurofibromatosis type 1. Neurooncol Adv. 2020; 2(Suppl 1):i124–33.8. Donk W, Poyck P, Westenend P, Lesterhuis W, Hesp F. Recurrent abdominal complaints caused by a cecal neurofibroma: a case report. World J Gastroenterol. 2011; 17:3953–6.9. Grouls V, Vaih S, Bindewald H. Involvement of the large intestine in neurofibromatosis type 1. Pathologe. 1996; 17:133–8.10. Yang KH, Rhim H, Cho OK, Ko BH, Kim Y, Lee HW, et al. Segmental colonic involvement of plexiform neurofibroma in neurofibromatosis type 1. J Comput Assist Tomogr. 2002; 26:129–31.11. Sathe PA, Kulkarni VM, Raut AA, Deolekar SS, Joshi AS. Ileal polyposis as manifestation of neurofibromatosis syndrome. Indian J Gastroenterol. 2006; 25:159–60.12. de Rezende NA, Arantes V, de Toledo LL, Ferreira MC, Toppa NH, Martins GM, et al. Plexiform neurofibroma: an unusual cause of GI bleeding and intestinal obstruction. Gastrointest Endosc. 2009; 70:396–8.13. Calligaris L, Marchetti F, Ventura A. Intestinal plexiform neurofibromas. Dig Liver Dis. 2008; 40:578.14. Fu CY, Lin CH, Peng YJ, Yu TC, Lu TC, Chen TW. Acute abdominal pain caused by spontaneous hemorrhagic infarction of a solitary plexiform neurofibroma of lesser omentum. Z Gastroenterol. 2008; 46:344–7.15. Agaimy A, Vassos N, Croner RS. Gastrointestinal manifestations of neurofibromatosis type 1 (Recklinghausen’s disease): clinicopathological spectrum with pathogenetic considerations. Int J Clin Exp Pathol. 2012; 5:852–62.16. Grover DS, Kundra DR, Grover DH, Gupta DV, Gupta DR. Imaging diagnosis of plexiform neurofibroma- unravelling the confounding features: a report of two cases. Radiol Case Rep. 2021; 16:2824–33.17. Tinguria M. An isolated colonic neurofibroma: a rare colonic neoplasm: case report with clinicopathologic features and review of literature. Hum Pathol Rep. 2022; 28:300650.18. Lee HJ, Koh BK, Ha SJ, Kim JW. A case of isolated plexiform neurofibroma. Ann Dermatol. 2000; 12:271–4.19. Ferner RE, Huson SM, Thomas N, Moss C, Willshaw H, Evans DG, et al. Guidelines for the diagnosis and management of individuals with neurofibromatosis 1. J Med Genet. 2007; 44:81–8.20. Hirbe AC, Gutmann DH. Neurofibromatosis type 1: a multidisciplinary approach to care. Lancet Neurol. 2014; 13:834–43.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Plexiform Neurofibroma Involving the Ascending Colonic Mesentery in Neurofibromatosis Type I
- Solitary Plexiform Neurofibroma on the Median Nerve: A Case Report
- A Case of Plexiform Neurofibroma Developed under the Overlying Speckled Lentiginous Nevus
- A Case of Isolated Plexiform Neurofibroma
- A Case of Plexiform Neurofibroma with Multiple Skeletal Abnormalities and Giant Pigmentation