Korean J Sports Med.
2023 Jun;41(2):107-110. 10.5763/kjsm.2023.41.2.107.
Exercise Capacity and Pulmonary Capacitance Are Attenuated in Patients with Nonalcoholic Steatohepatitis
- Affiliations
-
- 1Department of Cardiovascular Disease, Mayo Clinic, Rochester, MN, USA
- KMID: 2542982
- DOI: http://doi.org/10.5763/kjsm.2023.41.2.107
Abstract
- Purpose
The study was to investigate exercise capacity (peak oxygen uptake [peak VO2 ]) and pulmonary capacitance (GXcap), which is an estimate of pulmonary vascular capacitance, in patients with nonalcoholic steatohepatitis (NASH).
Methods
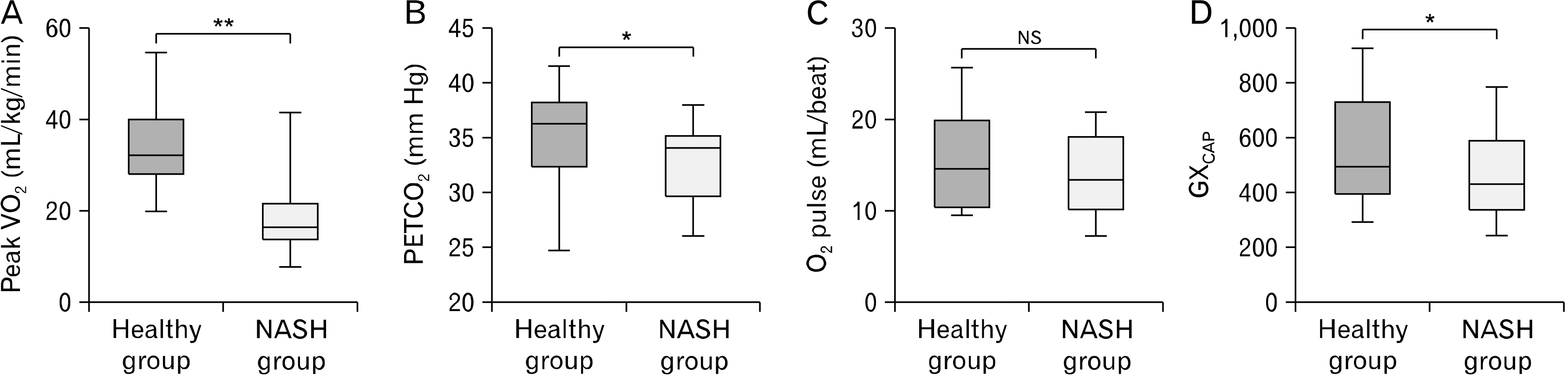
This study utilized a database of patients with NASH (n=26 [17 male and 9 female], aged 58.9±4.3 years) and healthy individuals (n=23 [12 male and 11 female, aged 58.6±7.9 years) who underwent a maximal exercise test on a recumbent cycle ergometer (Corival; Lode) in our laboratory. During cardiopulmonary exercise tests, breathing patterns and respiratory gas exchange including breathing efficiency (VE/VCO2 ) and end-tidal CO2 (PETCO2 ) were measured. In addition, peak VO2 was obtained via averaging the last 30 seconds at peak level and GXcap was obtained by calculation as follows: GXcap=oxygen pulse (O2 pulse)×PETCO2.
Results
The NASH group demonstrated reduced peak VO2 relative to the healthy group (17.5±8.4 mL/kg/min vs. 34±10.2 mL/kg/min, respectively; p< 0.05). In addition, there was a higher VE/VCO2 relationship in the NASH group relative to the healthy group (34.9±5.5 vs. 32.2±4.0, respectively; p< 0.05) and lower PETCO2 in the NASH group compared to the healthy group (32.8±4.0 mm Hg vs. 35.3±3.8 mm Hg, respectively; p< 0.05). Furthermore, the NASH group showed lower GXcap than the healthy group (456±150 vs. 551±202, respectively; p< 0.05).
Conclusion
Patients with NASH had reduced exercise capacity and pulmonary vascular capacitance relative to age-matched healthy adults and this may contribute to pulmonary pathophysiology in NASH.
Figure
Reference
-
1. Gutiérrez-Cuevas J, Lucano-Landeros S, López-Cifuentes D, Santos A, Armendariz-Borunda J. 2022; Epidemiologic, genetic, pathogenic, metabolic, epigenetic aspects involved in NASH-HCC: current therapeutic strategies. Cancers (Basel). 15:23. DOI: 10.3390/cancers15010023.
Article2. Rosato V, Masarone M, Dallio M, Federico A, Aglitti A, Persico M. 2019; NAFLD and extra-hepatic comorbidities: current evidence on a multi-organ metabolic syndrome. Int J Environ Res Public Health. 16:3415. DOI: 10.3390/ijerph16183415. PMID: 31540048. PMCID: PMC6765902.
Article3. Song JU, Jang Y, Lim SY, et al. 2019; Decreased lung function is associated with risk of developing non-alcoholic fatty liver disease: a longitudinal cohort study. PLoS One. 14:e0208736. DOI: 10.1371/journal.pone.0208736. PMID: 30673698. PMCID: PMC6343945.4. Mantovani A, Lonardo A, Vinco G, et al. 2019; Association between non-alcoholic fatty liver disease and decreased lung function in adults: a systematic review and meta-analysis. Diabetes Metab. 45:536–44. DOI: 10.1016/j.diabet.2019.04.008. PMID: 31067493.
Article5. Botello-Manilla AE, López-Sánchez GN, Chávez-Tapia NC, Uribe M, Nuño-Lámbarri N. 2021; Hepatic steatosis and respiratory diseases: a new panorama. Ann Hepatol. 24:100320. DOI: 10.1016/j.aohep.2021.100320. PMID: 33549735.
Article6. Cho J, Johnson BD, Watt KD, Niven AS, Yeo D, Kim CH. 2022; Exercise training attenuates pulmonary inflammation and mitochondrial dysfunction in a mouse model of high-fat high-carbohydrate-induced NAFLD. BMC Med. 20:429. DOI: 10.1186/s12916-022-02629-1. PMID: 36348343. PMCID: PMC9644617.7. McNeill JN, Lau ES, Zern EK, et al. 2021; Association of obesity-related inflammatory pathways with lung function and exercise capacity. Respir Med. 183:106434. DOI: 10.1016/j.rmed.2021.106434. PMID: 33964816. PMCID: PMC8144063.
Article8. Bhambhani Y, Norris S, Bell G. 1994; Prediction of stroke volume from oxygen pulse measurements in untrained and trained men. Can J Appl Physiol. 19:49–59. DOI: 10.1139/h94-003. PMID: 8186762.
Article9. Taylor BJ, Olson TP, Chul-Ho Kim, Maccarter D, Johnson BD. 2013; Use of noninvasive gas exchange to track pulmonary vascular responses to exercise in heart failure. Clin Med Insights Circ Respir Pulm Med. 7:53–60. DOI: 10.4137/CCRPM.S12178. PMID: 24093002. PMCID: PMC3785385.
Article10. Kim CH, Hansen JE, MacCarter DJ, Johnson BD. 2017; Algorithm for predicting disease likelihood from a submaximal exercise test. Clin Med Insights Circ Respir Pulm Med. 11:1179548417719248. DOI: 10.1177/1179548417719248. PMID: 28757799. PMCID: PMC5513526.11. Taylor BJ, Smetana MR, Frantz RP, Johnson BD. 2015; Submaximal exercise pulmonary gas exchange in left heart disease patients with different forms of pulmonary hypertension. J Card Fail. 21:647–55. DOI: 10.1016/j.cardfail.2015.04.003. PMID: 25887446. PMCID: PMC4522389.
Article12. Türker F, Sahın T, Oral A, et al. 2022; Evaluation of predisposing metabolic risk factors for portopulmonary hypertension in patients with NASH cirrhosis. Int J Gen Med. 15:859–65. DOI: 10.2147/IJGM.S339474.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nonalcoholic Steatohepatitis
- Pathology of nonalcoholic steatohepatitis
- Management of Patients with Nonalcoholic Fatty Liver Disease with Lifestyle Modification
- Clinical Predictors Reflecting the Pathologic Severity of Nonalcoholic Steatohepatitis in Patients with Nonalcoholic Fatty Liver
- The Diagnosis of Nonalcoholic Fatty Liver Disease