Arch Hand Microsurg.
2023 Jun;28(2):97-105. 10.12790/ahm.23.0004.
Comparison of fasciocutaneous and fascial anterolateral thigh free flaps in foot reconstruction
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Gwangmyeong Sungae General Hospital, Gwangmyeong, Korea
- KMID: 2542560
- DOI: http://doi.org/10.12790/ahm.23.0004
Abstract
- Purpose
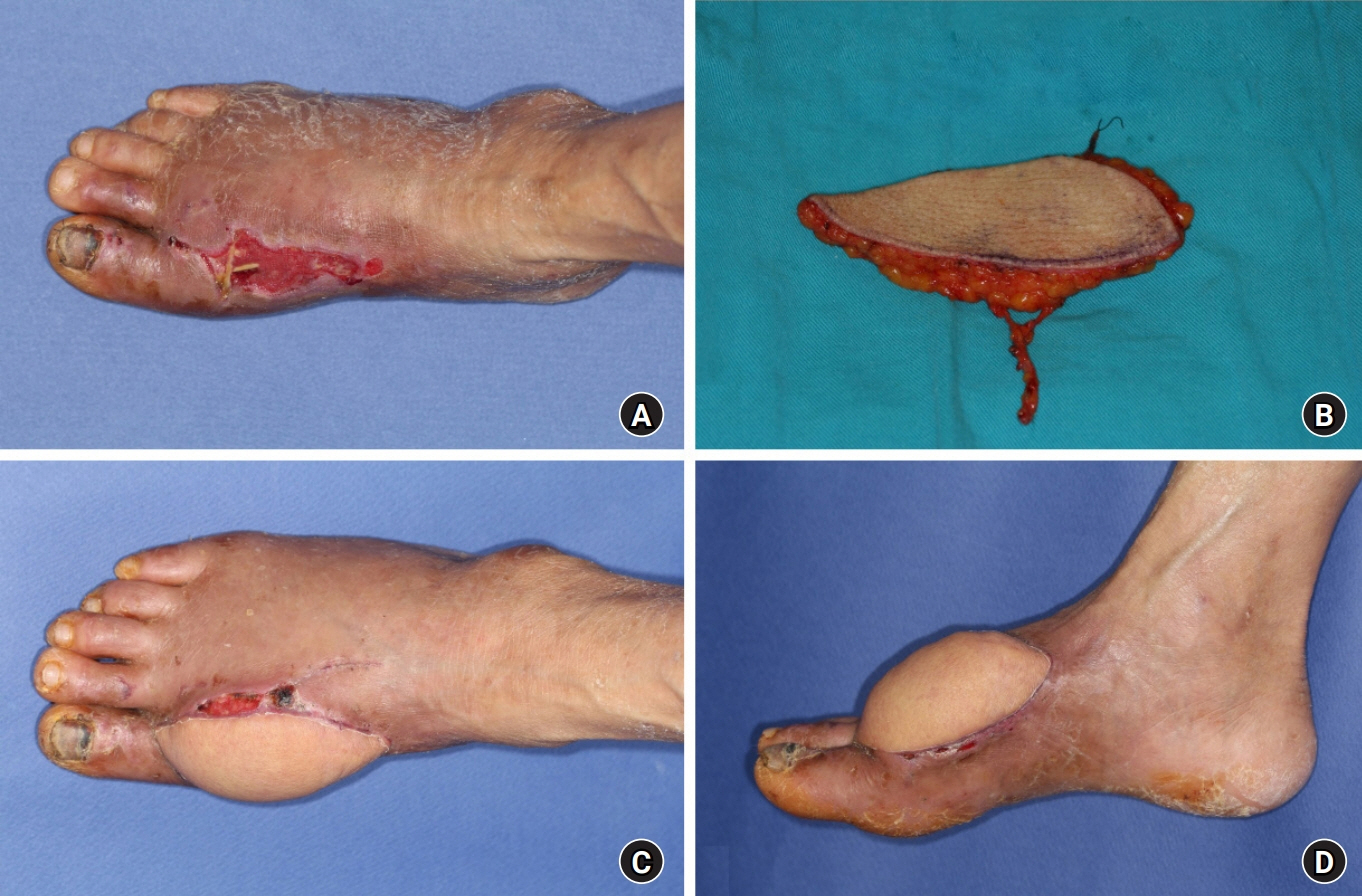
This study compared the surgical outcomes and quality of life of patients who underwent fasciocutaneous and fascial anterolateral thigh (ALT) free flaps for the reconstruction of traumatic soft tissue defects in the foot.
Methods
A single-institution retrospective review of medical data from 2008 to 2021 was conducted on 20 patients who underwent a fasciocutaneous ALT free flap or fascial ALT free flap in the foot. Information was collected on patients’ baseline information, preoperative characteristics, and postoperative courses. Quality of life was measured through the Foot and Ankle Disability Index (FADI) score. A questionnaire survey was administered to evaluate aesthetic satisfaction and subjective improvement of dryness and sensory function at the surgical site.
Results
The mean flap dimensions were 13.96×4.58 cm and 10.75×3.50 cm in the fasciocutaneous and fascial groups, respectively. The overall flap failure and complication rates were higher in the fasciocutaneous group (total necrosis in one case, partial flap loss in two cases, and vascular complications in three cases). While aesthetic satisfaction and functional outcomes (FADI Sports) showed better outcomes in the fascial group, subjective improvement of dryness and sensory recovery showed better results in the fasciocutaneous group.
Conclusion
In comparison to fasciocutaneous flaps, fascial free flaps demonstrated lower rates of wound complications, higher aesthetic satisfaction, and better functional outcomes, but less improvement in dryness and sensory recovery at the flap site. Therefore, the choice of a flap for foot reconstruction should depend on the plastic surgeon’s discretion and a thorough discussion with the patient.
Figure
Reference
-
References
1. Mulligan ME. Ankle and foot trauma. Semin Musculoskelet Radiol. 2000; 4:241–53.
Article2. Song YG, Chen GZ, Song YL. The free thigh flap: a new free flap concept based on the septocutaneous artery. Br J Plast Surg. 1984; 37:149–59.
Article3. Lee YC, Chiu HY, Shieh SJ. The clinical application of anterolateral thigh flap. Plast Surg Int. 2011; 2011:127353.
Article4. Yang WG, Chiang YC, Wei FC, Feng GM, Chen KT. Thin anterolateral thigh perforator flap using a modified perforator microdissection technique and its clinical application for foot resurfacing. Plast Reconstr Surg. 2006; 117:1004–8.
Article5. Smith RA. The free fascial scalp flap. Plast Reconstr Surg. 1980; 66:204–9.
Article6. Hsieh CH, Yang CC, Kuo YR, Tsai HH, Jeng SF. Free anterolateral thigh adipofascial perforator flap. Plast Reconstr Surg. 2003; 112:976–82.
Article7. Nasajpour H, Steele MH. Anterolateral thigh free flap for “head-to-toe” reconstruction. Ann Plast Surg. 2011; 66:530–3.
Article8. Ozkan O, Coşkunfirat OK, Ozgentaş HE. The use of free anterolateral thigh flap for reconstructing soft tissue defects of the lower extremities. Ann Plast Surg. 2004; 53:455–61.
Article9. Wei FC, Jain V, Celik N, Chen HC, Chuang DC, Lin CH. Have we found an ideal soft-tissue flap?: an experience with 672 anterolateral thigh flaps. Plast Reconstr Surg. 2002; 109:2219–30.
Article10. Brenner P, Rammelt S, Gavlik JM, Zwipp H. Early soft tissue coverage after complex foot trauma. World J Surg. 2001; 25:603–9.
Article11. Sato T, Yana Y, Ichioka S. Free flap reconstruction for diabetic foot limb salvage. J Plast Surg Hand Surg. 2017; 51:399–404.
Article12. Kolbenschlag J, Hellmich S, Germann G, Megerle K. Free tissue transfer in patients with severe peripheral arterial disease: functional outcome in reconstruction of chronic lower extremity defects. J Reconstr Microsurg. 2013; 29:607–14.
Article13. Lähteenmäki T, Waris T, Asko-Seljavaara S, Sundell B. Recovery of sensation in free flaps. Scand J Plast Reconstr Surg Hand Surg. 1989; 23:217–22.
Article14. Lowrey CR, Strzalkowski ND, Bent LR. Skin sensory information from the dorsum of the foot and ankle is necessary for kinesthesia at the ankle joint. Neurosci Lett. 2010; 485:6–10.
Article15. El-Gammal TA, El-Sayed A, Kotb MM, et al. Dorsal foot resurfacing using free anterolateral thigh (ALT) flap in children. Microsurgery. 2013; 33:259–64.
Article16. Rhodius P, Haddad A, Matsumine H, et al. Noninvasive flap preconditioning by foam-mediated external suction improves the survival of fasciocutaneous axial-pattern flaps in a type 2 diabetic murine model. Plast Reconstr Surg. 2018; 142:872e–883e.
Article17. Lee ZH, Abdou SA, Ramly EP, et al. Larger free flap size is associated with increased complications in lower extremity trauma reconstruction. Microsurgery. 2020; 40:473–8.
Article18. Boca R, Kuo YR, Hsieh CH, Huang EY, Jeng SF. A reliable parameter for primary closure of the free anterolateral thigh flap donor site. Plast Reconstr Surg. 2010; 126:1558–62.
Article19. Custozzo A, Frank K, Schenck TL, et al. Anatomy of the dorsum of the foot and its relevance for nonsurgical cosmetic procedures. Plast Reconstr Surg. 2020; 146:64–72.
Article20. Sanchez BY, Gallardo DD, Espinoza JA, Soto DF. Subunit Principle: key element for plantar reconstruction with free sensate flaps. Arch Hand Microsurg. 2021; 26:43–9.
Article21. Lee MG, Kim JS, Lee DC, Roh SY, Lee KJ, Choi BK. Fascial free flap for reconstruction of the dorsolateral hand and digits: the advantage of a thin contour. Arch Plast Surg. 2016; 43:551–8.
Article22. Seyhan T. Split-thickness skin grafts. In : Marcia Spear, editor. Skin grafts: indications, applications and current research. Rijeka, Croatia: IntechOpen;2011.23. Kimura N, Satoh K. Consideration of a thin flap as an entity and clinical applications of the thin anterolateral thigh flap. Plast Reconstr Surg. 1996; 97:985–92.
Article24. Kimura N, Satoh K, Hasumi T, Ostuka T. Clinical application of the free thin anterolateral thigh flap in 31 consecutive patients. Plast Reconstr Surg. 2001; 108:1197–210.
Article25. Sharabi SE, Hatef DA, Koshy JC, Jain A, Cole PD, Hollier LH Jr. Is primary thinning of the anterolateral thigh flap recommended? Ann Plast Surg. 2010; 65:555–9.
Article26. Agostini T, Lazzeri D, Spinelli G. Anterolateral thigh flap thinning: techniques and complications. Ann Plast Surg. 2014; 72:246–52.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reconstruction of Tissue Defects with Anterolateral Thigh Sensate Free Flap
- Reconstruction of Hand using Anterolateral Thigh Fascial Free Flap
- Soft Tissue Reconstruction Using Anterolateral Thigh Flap with Fascia Lata Component
- Total Tongue Reconstruction with Folded Anterolateral Thigh Free Flap
- Pedicled sural flaps versus free anterolateral thigh flaps in reconstruction of dorsal foot and ankle defects in children: a systematic review