Arch Hand Microsurg.
2023 Jun;28(2):75-86. 10.12790/ahm.23.0005.
Management of metacarpal and phalangeal fractures
- Affiliations
-
- 1Department of Orthopedic Surgery, Daegu Catholic University Hospital, Daegu Catholic University College of Medicine, Daegu, Korea
- 2Department of Orthopedic Surgery, Bucheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Bucheon, Korea
- KMID: 2542557
- DOI: http://doi.org/10.12790/ahm.23.0005
Abstract
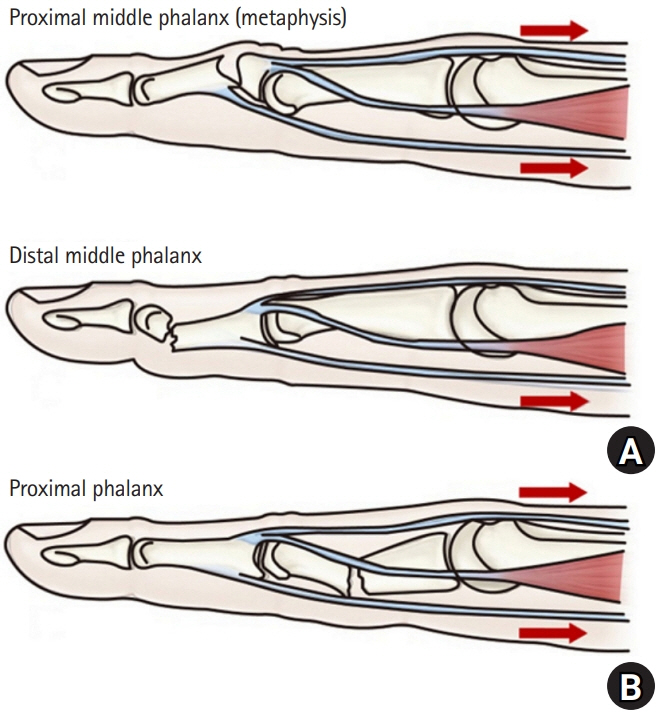
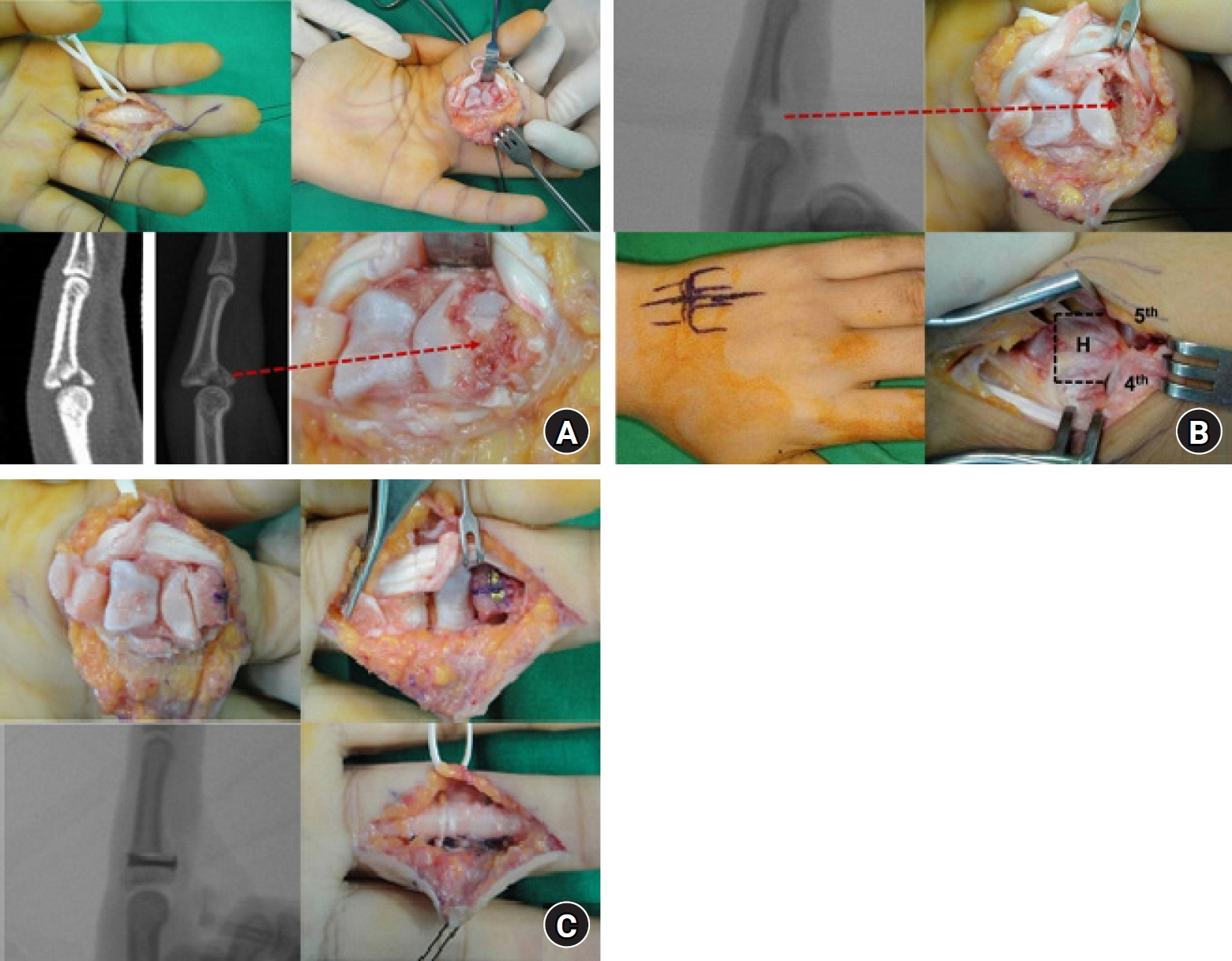
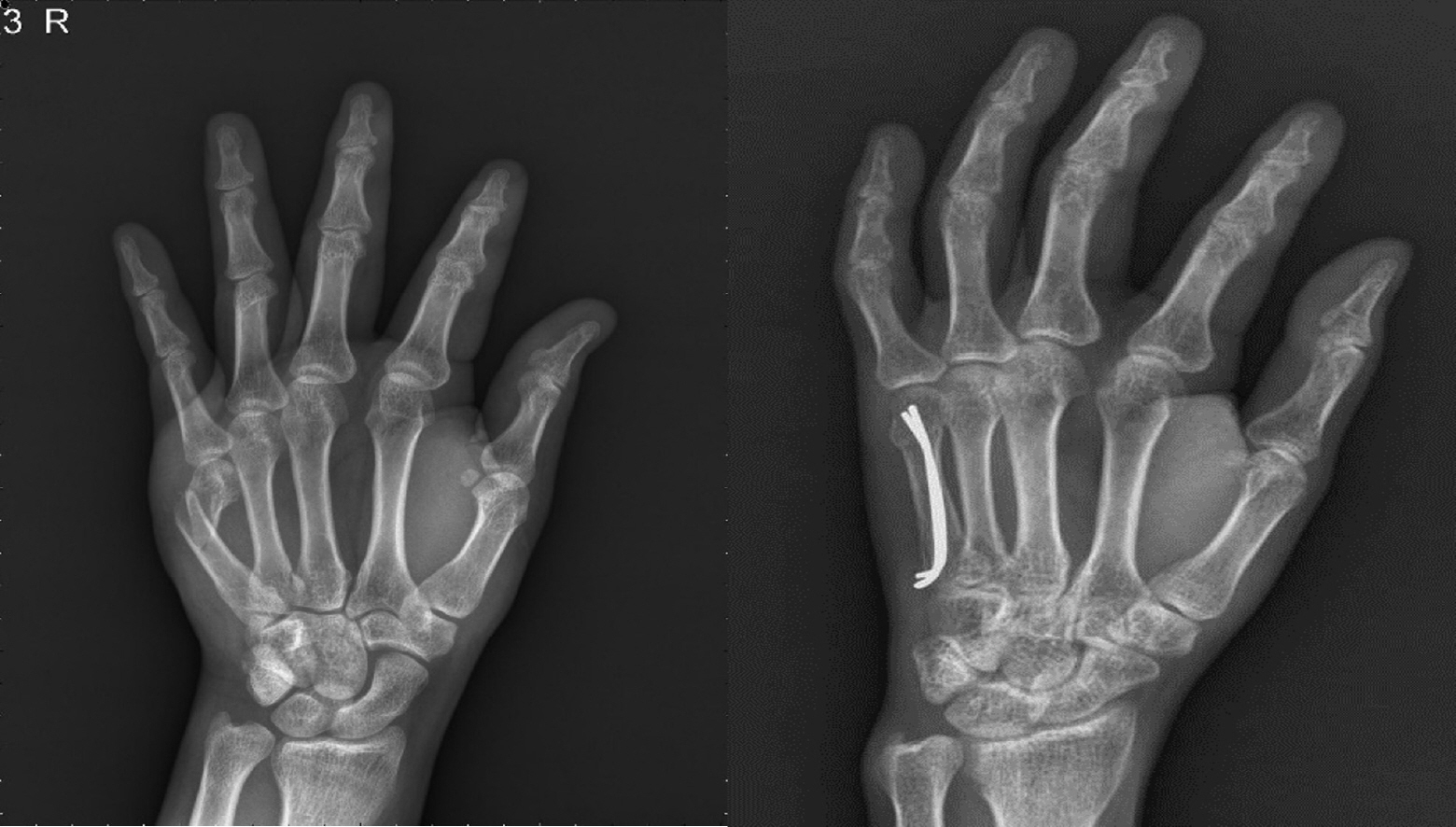
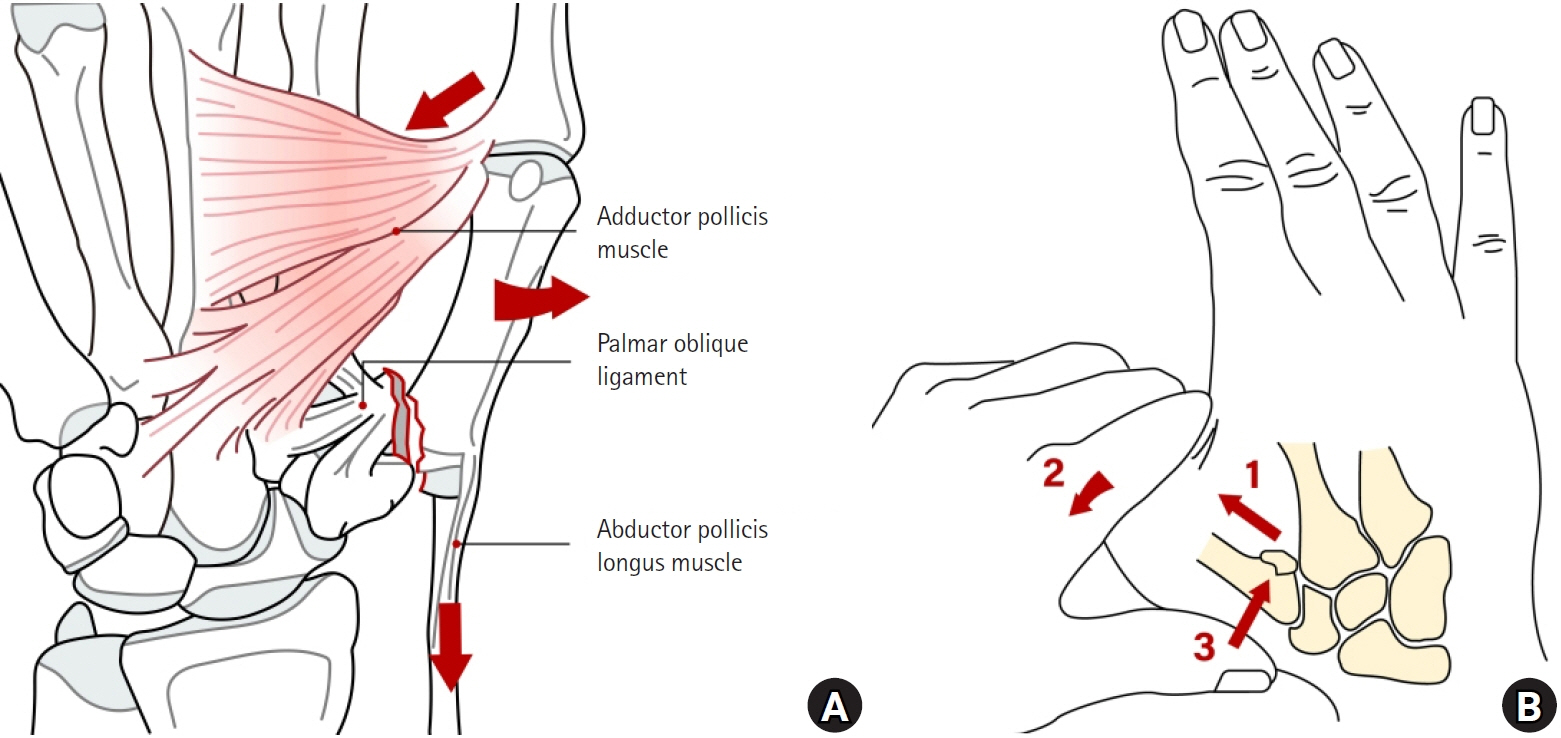
- Hand fractures are the most common fractures in orthopedic surgery. In most cases, conservative treatment is sufficient for stable fractures, but surgical treatment is required for unstable fractures, fractures that cannot be maintained after reduction, and fractures with severe soft tissue injuries. In the management of hand fractures, the focus should be on restoring the function of the hand after fracture healing. Rapid rehabilitation exercises are an important factor in restoring the function of the hand by reducing swelling at the fracture site, preventing joint stiffness, and reducing soft tissue adhesion. Therefore, conservative treatment that can minimize soft tissue damage is usually prioritized, and in specific situations, if surgical intervention can help facilitate early rehabilitation exercises, then it could be a desirable choice. This review article aims to help readers decide on a treatment method by presenting various treatment methods for hand fractures and the academic basis for those options.
Keyword
- 수지; 중수골; 골절; 고정; 손; Phalangeal; Metacarpal; Fracture; Fixation; Hand
Figure
Cited by 1 articles
-
A novel finger brace for preventing finger stiffness after trauma or surgery: a preliminary report with a case series
Dae-Geun Kim, Hyo Jun Park
Arch Hand Microsurg. 2023;28(4):239-249. doi: 10.12790/ahm.23.0033.
Reference
-
References
1. Taghinia AH, Talbot SG. Phalangeal and metacarpal fractures. Clin Plast Surg. 2019; 46:415–23.
Article2. Jordan DJ, Leow JM, Stirling PH, Lam WL, et al. Revisiting the dogma of the Edinburgh position for safe immobilization. J Hand Surg Eur. 2021; 46:37–44.
Article3. Leddy JP, Packer JW. Avulsion of the profundus tendon insertion in athletes. J Hand Surg Am. 1977; 2:66–9.
Article4. Figl M, Weninger P, Hofbauer M, Pezzei C, Schauer J, Leixnering M. Results of dynamic treatment of fractures of the proximal phalanx of the hand. J Trauma. 2011; 70:852–6.
Article5. Williams RM, Kiefhaber TR, Sommerkamp TG, Stern PJ. Treatment of unstable dorsal proximal interphalangeal fracture/dislocations using a hemi-hamate autograft. J Hand Surg Am. 2003; 28:856–65.
Article6. Kiefhaber TR, Stern PJ. Fracture dislocations of the proximal interphalangeal joint. J Hand Surg Am. 1998; 23:368–80.
Article7. Cheah AE, Yao J. Hand fractures: indications, the tried and true and new innovations. J Hand Surg Am. 2016; 41(6):712–22.
Article8. Vitale MA, White NJ, Strauch RJ. A percutaneous technique to treat unstable dorsal fracture-dislocations of the proximal interphalangeal joint. J Hand Surg Am. 2011; 36:1453–9.
Article9. Waris E, Alanen V. Percutaneous, intramedullary fracture reduction and extension block pinning for dorsal proximal interphalangeal fracture-dislocations. J Hand Surg Am. 2010; 35:2046–52.
Article10. Culp RW, Johnson JW. Arthroscopically assisted percutaneous fixation of bennett fractures. J Hand Surg Am. 2010; 35:137–40.
Article11. Ozer K. Temporary bridge plate fixation of pilon fractures of the proximal interphalangeal joint. J Hand Surg Am. 2019; 44:524.e1–6.
Article12. Zhang L, Lü Y, Lu C, Wang X, Guo S, Zhang H. Treatment of the fifth metacarpal neck fracture with elastic intramedullary nail under the guidance of high frequency ultrasound. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2021; 35:154–9. Chinese.13. Gil HJ, Chung YG, Shin SH, Kim DH, Kang JW, Jeon SH. Modified split ulnar gutter splint for treatment of fifth metacarpal neck fractures. J Korean Soc Surg Hand. 2015; 20:161–7.
Article14. Tosti R, Ilyas AM, Mellema JJ, Guitton TG, Ring D; Science of Variation Group. Interobserver variability in the treatment of little finger metacarpal neck fractures. J Hand Surg Am. 2014; 39:1722–7.15. Kollitz KM, Hammert WC, Vedder NB, Huang JI. Metacarpal fractures: treatment and complications. Hand (N Y). 2014; 9:16–23.
Article16. Statius Muller MG, Poolman RW, van Hoogstraten MJ, Steller EP. Immediate mobilization gives good results in boxer's fractures with volar angulation up to 70 degrees: a prospective randomized trial comparing immediate mobilization with cast immobilization. Arch Orthop Trauma Surg. 2003; 123:534–7.17. Lee SK, Kim KJ, Choy WS. Modified retrograde percutaneous intramedullary multiple Kirschner wire fixation for treatment of unstable displaced metacarpal neck and shaft fractures. Eur J Orthop Surg Traumatol. 2013; 23:535–43.
Article18. Ozer K, Gillani S, Williams A, Peterson SL, Morgan S. Comparison of intramedullary nailing versus plate-screw fixation of extra-articular metacarpal fractures. J Hand Surg Am. 2008; 33:1724–31.
Article19. Souer JS, Mudgal CS. Plate fixation in closed ipsilateral multiple metacarpal fractures. J Hand Surg Eur Vol. 2008; 33:740–4.
Article20. Marsland D, Sanghrajka AP, Goldie B. Static monolateral external fixation for the Rolando fracture: a simple solution for a complex fracture. Ann R Coll Surg Engl. 2012; 94:112–5.
Article21. Bannasch H, Heermann AK, Iblher N, Momeni A, Schulte-Mönting J, Stark GB. Ten years stable internal fixation of metacarpal and phalangeal hand fractures-risk factor and outcome analysis show no increase of complications in the treatment of open compared with closed fractures. J Trauma. 2010; 68:624–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Miniplate and Miniscrew Fixation for the Metacarpal and Phalangeal Fractures
- Usefulness of Miniplate Fixation for the Fractures of Metacarpal and Phalangeal Bones of the Hand
- The Results of Miniplate Fixation for the Fractures of Metacarpal and Phalangeal Bones of the Hand
- Operative Treatment in Fractures of the Metacarpal and Phalanx in the Crushing Injury
- A Clinical Study on the Fractures of the Hand: Factors influencing the results