Diabetes Metab J.
2023 May;47(3):325-332. 10.4093/dmj.2022.0349.
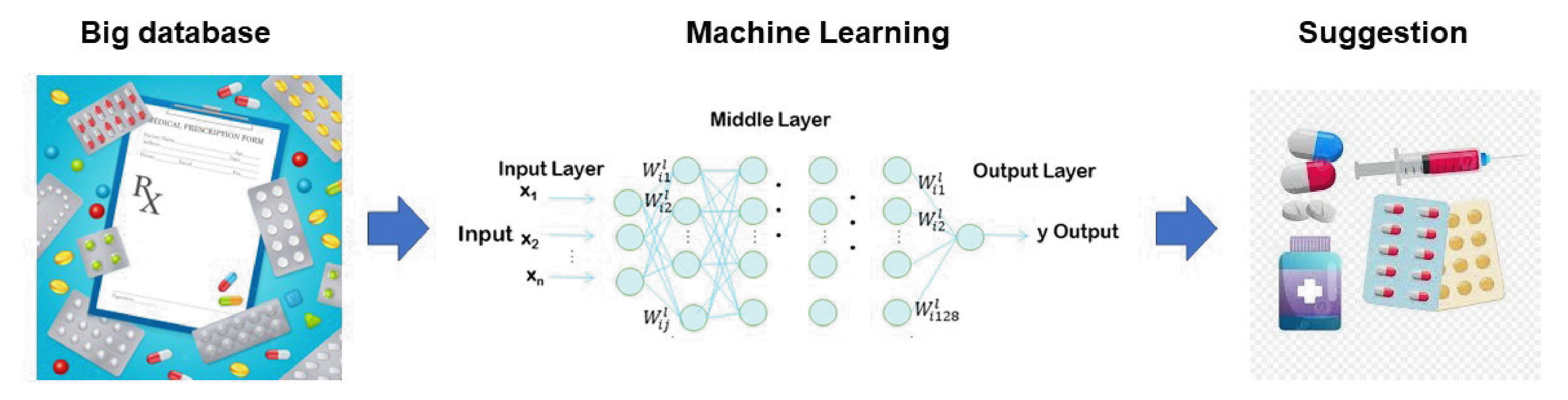
Machine Learning Approach to Drug Treatment Strategy for Diabetes Care
- Affiliations
-
- 1Department of Internal Medicine, Niigata University Faculty of Medicine, Niigata, Japan
- KMID: 2542509
- DOI: http://doi.org/10.4093/dmj.2022.0349
Abstract
- Globally, the number of people with diabetes mellitus has quadrupled in the past three decades, and approximately one in 11 adults worldwide have diabetes mellitus. Since both microvascular and macrovascular diseases in patients with diabetes predispose them to a lower quality of life as well as higher rates of mortality, managing blood glucose levels is of clinical relevance in diabetes care. Many classes of antihyperglycemic drugs are currently approved to treat hyperglycemia in patients with type 2 diabetes mellitus, with several new drugs having been developed during the last decade. Diabetes-related complications have been reduced substantially worldwide. Prioritization of therapeutic agents varies according to national guidelines. However, since the characteristics of participants in clinical trials differ from patients in actual clinical practice, it is difficult to apply the results of such trials to clinical practice. Machine learning approaches became highly topical issues in medicine along with rapid technological innovations in the fields of information and communication in the 1990s. However, adopting these technologies to support decision-making regarding drug treatment strategies for diabetes care has been slow. This review summarizes data from recent studies on the choice of drugs for type 2 diabetes mellitus focusing on machine learning approaches.
Keyword
Figure
Reference
-
1. Zheng Y, Ley SH, Hu FB. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol. 2018; 14:88–98.
Article2. Japan Diabetes Society. Treatment Guide for Diabetes 2022-2023. Tokyo: Japan Diabetes Society;2022.3. UK Prospective Diabetes Study (UKPDS) Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet. 1998; 352:854–65.4. UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ. 1998; 317:703–13.5. Shichiri M, Kishikawa H, Ohkubo Y, Wake N. Long-term results of the Kumamoto Study on optimal diabetes control in type 2 diabetic patients. Diabetes Care. 2000; 23 Suppl 2:B21–9.6. Sone H, Tanaka S, Iimuro S, Tanaka S, Oida K, Yamasaki Y, et al. Long-term lifestyle intervention lowers the incidence of stroke in Japanese patients with type 2 diabetes: a nationwide multicentre randomised controlled trial (the Japan Diabetes Complications Study). Diabetologia. 2010; 53:419–28.
Article7. Yamada-Harada M, Fujihara K, Osawa T, Yamamoto M, Kaneko M, Kitazawa M, et al. Relationship between number of multiple risk factors and coronary artery disease risk with and without diabetes mellitus. J Clin Endocrinol Metab. 2019; 104:5084–90.
Article8. Ueki K, Sasako T, Okazaki Y, Kato M, Okahata S, Katsuyama H, et al. Effect of an intensified multifactorial intervention on cardiovascular outcomes and mortality in type 2 diabetes (JDOIT3): an open-label, randomised controlled trial. Lancet Diabetes Endocrinol. 2017; 5:951–64.9. Centers for Disease Control and Prevention: Diabetes Fact Sheet. Available from: https://www.cdc.gov/diabetes/basics/quick-facts.html (cited 2023 Jan 2).10. Fujihara K, Sone H. Cardiovascular disease in Japanese patients with type 2 diabetes mellitus. Ann Vasc Dis. 2018; 11:2–14.
Article11. American Diabetes Association Professional Practice Committee, Draznin B, Aroda VR, Bakris G, Benson G, Brown FM, et al. 9. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes-2022. Diabetes Care. 2022; 45(Suppl 1):S125–43.12. Gregg EW, Li Y, Wang J, Burrows NR, Ali MK, Rolka D, et al. Changes in diabetes-related complications in the United States, 1990-2010. N Engl J Med. 2014; 370:1514–23.
Article13. Desouza CV, Bolli GB, Fonseca V. Hypoglycemia, diabetes, and cardiovascular events. Diabetes Care. 2010; 33:1389–94.
Article14. Rajkomar A, Dean J, Kohane I. Machine learning in medicine. N Engl J Med. 2019; 380:1347–58.
Article15. Yu KH, Beam AL, Kohane IS. Artificial intelligence in healthcare. Nat Biomed Eng. 2018; 2:719–31.
Article16. Perakakis N, Yazdani A, Karniadakis GE, Mantzoros C. Omics, big data and machine learning as tools to propel understanding of biological mechanisms and to discover novel diagnostics and therapeutics. Metabolism. 2018; 87:A1–9.
Article17. Muehlematter UJ, Daniore P, Vokinger KN. Approval of artificial intelligence and machine learning-based medical devices in the USA and Europe (2015-20): a comparative analysis. Lancet Digit Health. 2021; 3:e195–203.
Article18. Lyell D, Coiera E, Chen J, Shah P, Magrabi F. How machine learning is embedded to support clinician decision making: an analysis of FDA-approved medical devices. BMJ Health Care Inform. 2021; 28:e100301.19. Cabitza F, Rasoini R, Gensini GF. Unintended consequences of machine learning in medicine. JAMA. 2017; 318:517–8.
Article20. Kavakiotis I, Tsave O, Salifoglou A, Maglaveras N, Vlahavas I, Chouvarda I. Machine learning and data mining methods in diabetes research. Comput Struct Biotechnol J. 2017; 15:104–16.
Article21. Abhari S, Niakan Kalhori SR, Ebrahimi M, Hasannejadasl H, Garavand A. Artificial intelligence applications in type 2 diabetes mellitus care: focus on machine learning methods. Healthc Inform Res. 2019; 25:248–61.
Article22. Contreras I, Vehi J. Artificial intelligence for diabetes management and decision support: literature review. J Med Internet Res. 2018; 20:e10775.
Article23. Verbraak FD, Abramoff MD, Bausch GC, Klaver C, Nijpels G, Schlingemann RO, et al. Diagnostic accuracy of a device for the automated detection of diabetic retinopathy in a primary care setting. Diabetes Care. 2019; 42:651–6.
Article24. Haenssle HA, Fink C, Schneiderbauer R, Toberer F, Buhl T, Blum A, et al. Man against machine: diagnostic performance of a deep learning convolutional neural network for dermoscopic melanoma recognition in comparison to 58 dermatologists. Ann Oncol. 2018; 29:1836–42.25. Schmidt-Erfurth U, Sadeghipour A, Gerendas BS, Waldstein SM, Bogunovic H. Artificial intelligence in retina. Prog Retin Eye Res. 2018; 67:1–29.
Article26. Ting DSW, Pasquale LR, Peng L, Campbell JP, Lee AY, Raman R, et al. Artificial intelligence and deep learning in ophthalmology. Br J Ophthalmol. 2019; 103:167–75.
Article27. Munir K, Elahi H, Ayub A, Frezza F, Rizzi A. Cancer diagnosis using deep learning: a bibliographic review. Cancers (Basel). 2019; 11:1235.
Article28. Burt JR, Torosdagli N, Khosravan N, RaviPrakash H, Mortazi A, Tissavirasingham F, et al. Deep learning beyond cats and dogs: recent advances in diagnosing breast cancer with deep neural networks. Br J Radiol. 2018; 91:20170545.
Article29. Ravaut M, Harish V, Sadeghi H, Leung KK, Volkovs M, Kornas K, et al. Development and validation of a machine learning model using administrative health data to predict onset of type 2 diabetes. JAMA Netw Open. 2021; 4:e2111315.
Article30. Fujimaki R, Morinaga S. Factorized asymptotic Bayesian inference for mixture modeling. Proc Mach Learn Res. 2012; 22:400–8.31. Savage N. Breaking into the black box of artificial intelligence. Nature. 2022; Mar. 29. [Epub]. https://doi.org/10.1038/d41586-022-00858-1.
Article32. Ellahham S. Artificial intelligence: the future for diabetes care. Am J Med. 2020; 133:895–900.33. Gautier T, Ziegler LB, Gerber MS, Campos-Nanez E, Patek SD. Artificial intelligence and diabetes technology: a review. Metabolism. 2021; 124:154872.34. Nomura A, Noguchi M, Kometani M, Furukawa K, Yoneda T. Artificial intelligence in current diabetes management and prediction. Curr Diab Rep. 2021; 21:61.
Article35. Islam MM, Yang HC, Poly TN, Jian WS, Jack Li YC. Deep learning algorithms for detection of diabetic retinopathy in retinal fundus photographs: a systematic review and metaanalysis. Comput Methods Programs Biomed. 2020; 191:105320.36. Nimri R, Battelino T, Laffel LM, Slover RH, Schatz D, Weinzimer SA, et al. Insulin dose optimization using an automated artificial intelligence-based decision support system in youths with type 1 diabetes. Nat Med. 2020; 26:1380–4.
Article37. Kodama S, Fujihara K, Shiozaki H, Horikawa C, Yamada MH, Sato T, et al. Ability of current machine learning algorithms to predict and detect hypoglycemia in patients with diabetes mellitus: meta-analysis. JMIR Diabetes. 2021; 6:e22458.
Article38. Rollo ME, Aguiar EJ, Williams RL, Wynne K, Kriss M, Callister R, et al. eHealth technologies to support nutrition and physical activity behaviors in diabetes self-management. Diabetes Metab Syndr Obes. 2016; 9:381–90.
Article39. Yeoh E, Png D, Khoo J, Chee YJ, Sharda P, Low S, et al. A headto-head comparison between Guardian Connect and FreeStyle Libre systems and an evaluation of user acceptability of sensors in patients with type 1 diabetes. Diabetes Metab Res Rev. 2022; 38:e3560.
Article40. Krakauer M, Botero JF, Lavalle-Gonzalez FJ, Proietti A, Barbieri DE. A review of flash glucose monitoring in type 2 diabetes. Diabetol Metab Syndr. 2021; 13:42.
Article41. Evans M, Welsh Z, Ells S, Seibold A. The impact of flash glucose monitoring on glycaemic control as measured by HbA1c: a meta-analysis of clinical trials and real-world observational studies. Diabetes Ther. 2020; 11:83–95.
Article42. Zou Q, Qu K, Luo Y, Yin D, Ju Y, Tang H. Predicting diabetes mellitus with machine learning techniques. Front Genet. 2018; 9:515.
Article43. Kopitar L, Kocbek P, Cilar L, Sheikh A, Stiglic G. Early detection of type 2 diabetes mellitus using machine learning-based prediction models. Sci Rep. 2020; 10:11981.
Article44. Choi BG, Rha SW, Kim SW, Kang JH, Park JY, Noh YK. Machine learning for the prediction of new-onset diabetes mellitus during 5-year follow-up in non-diabetic patients with cardiovascular risks. Yonsei Med J. 2019; 60:191–9.45. Lai H, Huang H, Keshavjee K, Guergachi A, Gao X. Predictive models for diabetes mellitus using machine learning techniques. BMC Endocr Disord. 2019; 19:101.
Article46. Zhang L, Wang Y, Niu M, Wang C, Wang Z. Machine learning for characterizing risk of type 2 diabetes mellitus in a rural Chinese population: the Henan Rural Cohort Study. Sci Rep. 2020; 10:4406.
Article47. Nomura A, Yamamoto S, Hayakawa Y, Taniguchi K, Higashitani T, Aono D, et al. SAT-LB121 development of a machinelearning method for predicting new onset of diabetes mellitus: a retrospective analysis of 509,153 annual specific health checkup records. J Endocr Soc. 2020; 4(Supplement_1):SATLB121.48. American Diabetes Association. Standards of medical care in diabetes-2022 abridged for primary care providers. Clin Diabetes. 2022; 40:10–38.49. Desai NR, Shrank WH, Fischer MA, Avorn J, Liberman JN, Schneeweiss S, et al. Patterns of medication initiation in newly diagnosed diabetes mellitus: quality and cost implications. Am J Med. 2012; 125:302.50. Filion KB, Joseph L, Boivin JF, Suissa S, Brophy JM. Trends in the prescription of anti-diabetic medications in the United Kingdom: a population-based analysis. Pharmacoepidemiol Drug Saf. 2009; 18:973–6.51. Berkowitz SA, Krumme AA, Avorn J, Brennan T, Matlin OS, Spettell CM, et al. Initial choice of oral glucose-lowering medication for diabetes mellitus: a patient-centered comparative effectiveness study. JAMA Intern Med. 2014; 174:1955–62.52. Liu H, Xie G, Mei J, Shen W, Sun W, Li X. An efficacy driven approach for medication recommendation in type 2 diabetes treatment using data mining techniques. Stud Health Technol Inform. 2013; 192:1071.53. Wright AP, Wright AT, McCoy AB, Sittig DF. The use of sequential pattern mining to predict next prescribed medications. J Biomed Inform. 2015; 53:73–80.
Article54. Mei J, Zhao S, Jin F, Zhang L, Liu H, Li X, et al. Deep diabetologist: learning to prescribe hypoglycemic medications with recurrent neural networks. Stud Health Technol Inform. 2017; 245:1277.55. Tarumi S, Takeuchi W, Chalkidis G, Rodriguez-Loya S, Kuwata J, Flynn M, et al. Leveraging artificial intelligence to improve chronic disease care: methods and application to pharmacotherapy decision support for type-2 diabetes mellitus. Methods Inf Med. 2021; 60(S 01):e32–43.
Article56. Fujihara K, Matsubayashi Y, Harada Yamada M, Yamamoto M, Iizuka T, Miyamura K, et al. Machine learning approach to decision making for insulin initiation in Japanese patients with type 2 diabetes (JDDM 58): model development and validation study. JMIR Med Inform. 2021; 9:e22148.
Article57. Singla R, Aggarwal S, Bindra J, Garg A, Singla A. Developing clinical decision support system using machine learning methods for type 2 diabetes drug management. Indian J Endocrinol Metab. 2022; 26:44–9.58. Fujihara K, Igarashi R, Matsunaga S, Matsubayashi Y, Yamada T, Yokoyama H, et al. Comparison of baseline characteristics and clinical course in Japanese patients with type 2 diabetes among whom different types of oral hypoglycemic agents were chosen by diabetes specialists as initial monotherapy (JDDM 42). Medicine (Baltimore). 2017; 96:e6122.
Article59. Christodoulou E, Ma J, Collins GS, Steyerberg EW, Verbakel JY, Van Calster B. A systematic review shows no performance benefit of machine learning over logistic regression for clinical prediction models. J Clin Epidemiol. 2019; 110:12–22.
Article60. Stylianou N, Akbarov A, Kontopantelis E, Buchan I, Dunn KW. Mortality risk prediction in burn injury: comparison of logistic regression with machine learning approaches. Burns. 2015; 41:925–34.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Artificial intelligence, machine learning, and deep learning in women’s health nursing
- A Study on Methodologies of Drug Repositioning Using Biomedical Big Data: A Focus on Diabetes Mellitus
- Machine Learning Application in Diabetes and Endocrine Disorders
- Application of Machine Learning in Rhinology: A State of the Art Review
- Prediction of Diabetic Neuropathy Using Machine Learning Techniques