Korean Circ J.
2023 Apr;53(4):254-267. 10.4070/kcj.2022.0197.
The Clinical Outcomes of Marginal Donor Hearts: A Single Center Experience
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine and Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea
- 2Department of Thoracic and Cardiovascular Surgery and Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea
- KMID: 2542296
- DOI: http://doi.org/10.4070/kcj.2022.0197
Abstract
- Background and Objectives
Although the shortage of donor is a common problem worldwide, a significant portion of unutilized hearts are classified as marginal donor (MD) hearts. However, research on the correlation between the MD and the prognosis of heart transplantation (HTx) is lacking. This study was conducted to investigate the clinical impact of MD in HTx.
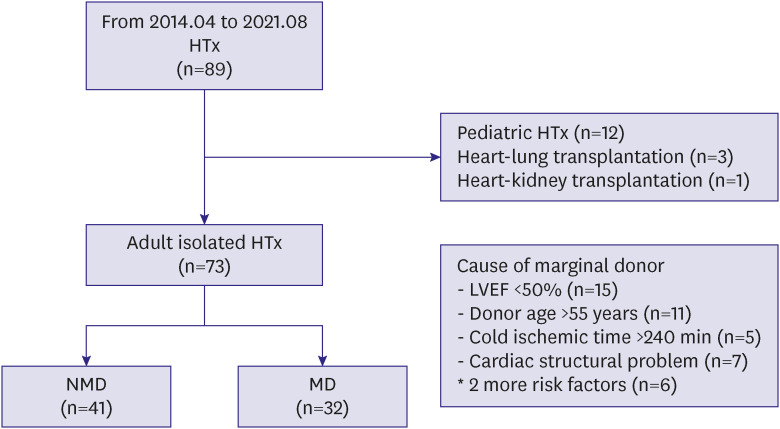
Methods
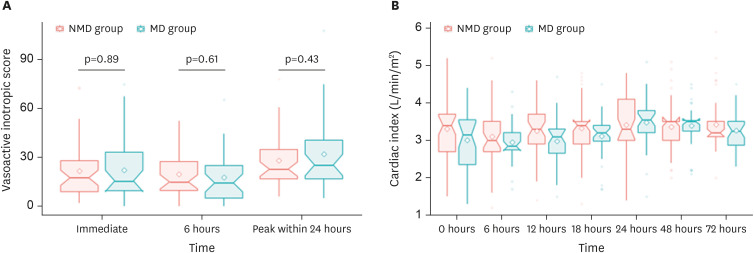
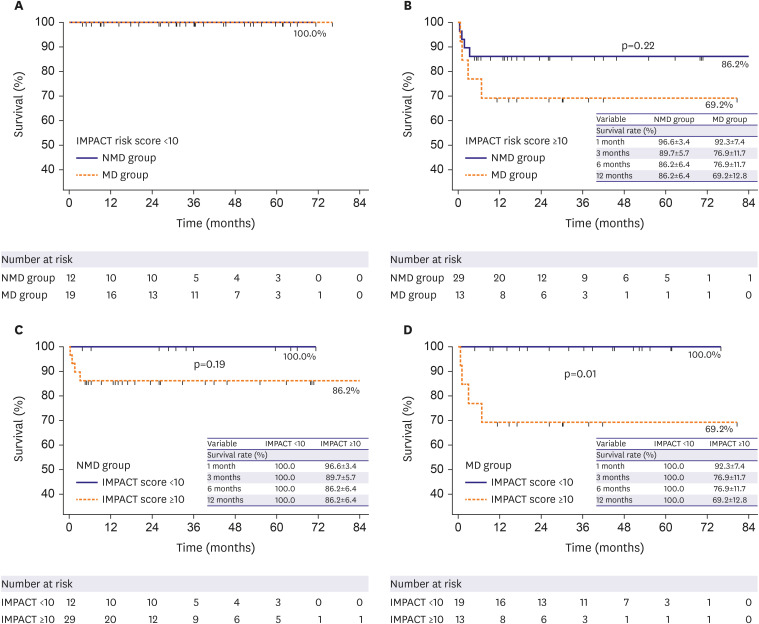
Consecutive 73 HTxs during 2014 and 2021 in a tertiary hospital were analyzed. MD was defined as follows; a donor age >55 years, left ventricular ejection fraction <50%, cold ischemic time >240 minutes, or significant cardiac structural problems. Preoperative characteristics and postoperative hemodynamic data, primary graft dysfunction (PGD), and the survival rate were analyzed. Risk stratification by Index for Mortality Prediction after Cardiac Transplantation (IMPACT) score was performed to examine the outcomes according to the recipient state. Each group was sub-divided into 2 risk groups according to the IMPACT score (low <10 vs. high ≥10).
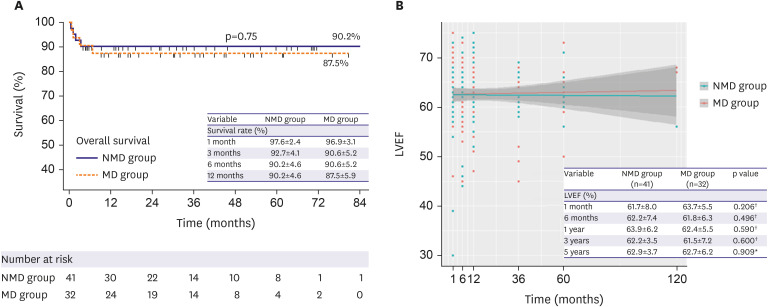
Results
A total of 32 (43.8%) patients received an organ from MDs. Extracorporeal membrane oxygenation was more frequent in the non-MD group (34.4% vs. 70.7, p=0.007) There was no significant difference in PGD, 30-day mortality and long-term survival between groups. In the subgroup analysis, early outcomes did not differ between low- and high-risk groups. However, the long-term survival was better in the low-risk group (p=0.01).
Conclusions
The outcomes of MD group were not significantly different from non-MD group. Particularly, in low-risk recipient, the MD group showed excellent early and longterm outcomes. These results suggest the usability of selected MD hearts without increasing adverse events.
Keyword
Figure
Cited by 1 articles
-
To Take or Not to Take: The Dilemma With Marginal Donor Heart?
Jin Joo Park
Korean Circ J. 2023;53(4):268-270. doi: 10.4070/kcj.2023.0045.
Reference
-
1. Eurotransplant International Foundation. Eurotransplant annual report 2020. Leiden: Eurotransplant International Foundation;2020.2. Colvin M, Smith JM, Ahn Y, et al. OPTN/SRTR 2020 Annual Data Report: Heart. Am J Transplant. 2022; 22(Suppl):350–437. PMID: 35266620.
Article3. Korea Organ Donation Agency. Report from Korean Organ Donation Agency [Internet]. Seoul: Korea Organ Donation Agency;2020. Available from: https://www.koda1458.kr/info/transplant.do.4. Korean Network for Organ Sharing. 2019 KONOS annual report. Seoul: Korean Network for Organ Sharing;2019.5. Zaroff JG, Rosengard BR, Armstrong WF, et al. Consensus conference report: maximizing use of organs recovered from the cadaver donor: cardiac recommendations, March 28-29, 2001, Crystal City, Va. Circulation. 2002; 106:836–841. PMID: 12176957.6. Kim JC, Youn JC, Lee SE, Jung SH, Kim JJ. Donor heart utilization in Korea. Int J Heart Fail. 2020; 2:254–263. PMID: 36262172.
Article7. Kobashigawa J, Zuckermann A, Macdonald P, et al. Report from a consensus conference on primary graft dysfunction after cardiac transplantation. J Heart Lung Transplant. 2014; 33:327–340. PMID: 24661451.
Article8. Weiss ES, Allen JG, Arnaoutakis GJ, et al. Creation of a quantitative recipient risk Index for Mortality Prediction after Cardiac Transplantation (IMPACT). Ann Thorac Surg. 2011; 92:914–921. PMID: 21871277.
Article9. Kilic A, Allen JG, Weiss ES. Validation of the United States-derived Index for Mortality Prediction After Cardiac Transplantation (IMPACT) using international registry data. J Heart Lung Transplant. 2013; 32:492–498. PMID: 23474362.
Article10. Singh SS, Dalzell JR, Berry C, Al-Attar N. Primary graft dysfunction after heart transplantation: a thorn amongst the roses. Heart Fail Rev. 2019; 24:805–820. PMID: 31020451.
Article11. Choi JO. Use of organ from marginal donor in cardiac transplantation: is it ready for us? Int J Heart Fail. 2020; 2:244–246. PMID: 36262170.
Article12. Aliabadi-Zuckermann AZ, Gökler J, Kaider A, et al. Donor heart selection and outcomes: an analysis of over 2,000 cases. J Heart Lung Transplant. 2018; 37:976–984. PMID: 29802081.
Article13. Wang Y, Cai J, Sun Y, et al. Extended donor criteria in heart transplantation: a retrospective study from a single Chinese institution. J Thorac Dis. 2018; 10:2153–2165. PMID: 29850119.
Article14. Galeone A, Lebreton G, Coutance G, et al. A single-center long-term experience with marginal donor utilization for heart transplantation. Clin Transplant. 2020; 34:e14057. PMID: 32757285.
Article15. Bifulco O, Bottio T, Caraffa R, et al. Marginal versus standard donors in heart transplantation: proper selection means heart transplant benefit. J Clin Med. 2022; 11:2665. PMID: 35566789.
Article16. Lima B, Rajagopal K, Petersen RP, et al. Marginal cardiac allografts do not have increased primary graft dysfunction in alternate list transplantation. Circulation. 2006; 114:I27–32. PMID: 16820584.
Article17. Chen JM, Russo MJ, Hammond KM, et al. Alternate waiting list strategies for heart transplantation maximize donor organ utilization. Ann Thorac Surg. 2005; 80:224–228. PMID: 15975371.
Article18. Rajagopalan N, Shafii AE, Dennis DR, Charnigo R, Sekela ME. Increasing heart transplant volume by expansion of donor heart selection criteria: a single-center analysis. Transplant Proc. 2020; 52:949–953. PMID: 32143873.
Article19. Trivedi JR, Cheng A, Ising M, Lenneman A, Birks E, Slaughter MS. Heart transplant survival based on recipient and donor risk scoring: a UNOS database analysis. ASAIO J. 2016; 62:297–301. PMID: 26771395.
Article20. Sathianathan S, Bhat G. Heart transplant donor selection guidelines: review and recommendations. Curr Cardiol Rep. 2022; 24:119–130. PMID: 35179716.
Article21. Taylor DO, Edwards LB, Aurora P, et al. Registry of the International Society for Heart and Lung Transplantation: twenty-fifth official adult heart transplant report--2008. J Heart Lung Transplant. 2008; 27:943–956. PMID: 18765186.
Article22. Blanche C, Kamlot A, Blanche DA, et al. Heart transplantation with donors fifty years of age and older. J Thorac Cardiovasc Surg. 2002; 123:810–815. PMID: 11986611.
Article23. Hong KN, Iribarne A, Worku B, et al. Who is the high-risk recipient? Predicting mortality after heart transplant using pretransplant donor and recipient risk factors. Ann Thorac Surg. 2011; 92:520–527. PMID: 21683337.
Article24. Daniel M, Chen C, Chung J, Goldberg L, Acker MA, Atluri P. Interaction of donor and recipient age: do older heart transplant recipients require younger hearts? Ann Thorac Surg. 2019; 107:62–66. PMID: 30172858.
Article25. World Health Organization. World Health Statistics 2021. Geneva: World Health Organization;2021.26. Khush KK, Cherikh WS, Chambers DC, et al. The international thoracic organ transplant registry of the International Society for Heart and Lung Transplantation: thirty-fifth Adult Heart Transplantation Report-2018; Focus Theme: Multiorgan transplantation. J Heart Lung Transplant. 2018; 37:1155–1168. PMID: 30293612.
Article27. Dujardin KS, McCully RB, Wijdicks EF, et al. Myocardial dysfunction associated with brain death: clinical, echocardiographic, and pathologic features. J Heart Lung Transplant. 2001; 20:350–357. PMID: 11257562.
Article28. Madan S, Saeed O, Vlismas P, et al. Outcomes after transplantation of donor hearts with improving left ventricular systolic dysfunction. J Am Coll Cardiol. 2017; 70:1248–1258. PMID: 28859788.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The clinical outcomes of marginal donor hearts: a single center experience
- The outcomes of marginal donor hearts compared with ideal donors: a single-center experience in Iran
- Split liver transplantation for one adult and one pediatric recipient: A collective review of Korean experience
- Experience of split liver transplantation from deceased marginal donor: eight adult recipients from four deceased donors
- A Preliminary Study to Revise the Marginal Donor Criteria of KONOS in Deceased Donor Kidney Transplantation