J Korean Neurosurg Soc.
2023 May;66(3):228-238. 10.3340/jkns.2022.0288.
Pathogenesis and Prevention of Intraventricular Hemorrhage in Preterm Infants
- Affiliations
-
- 1Department of Pediatrics, School of Medicine, National Yang Ming Chiao Tung University, Taipei, Taiwan
- 2Department of Pediatrics, Taipei Veterans General Hospital, Taipei, Taiwan
- KMID: 2542007
- DOI: http://doi.org/10.3340/jkns.2022.0288
Abstract
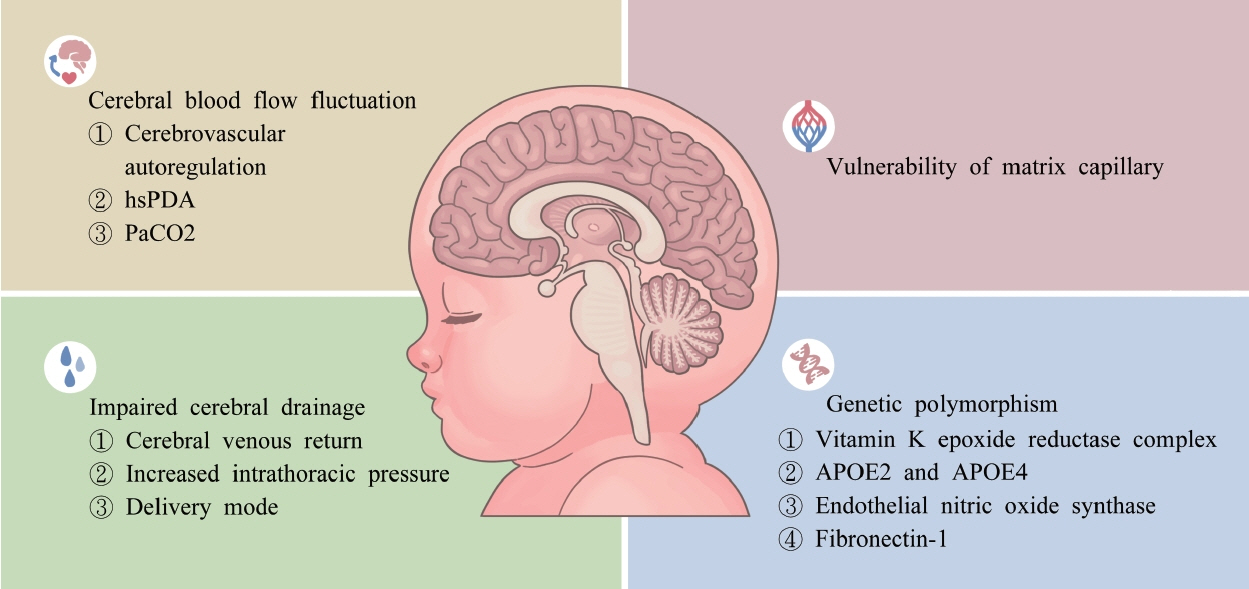
- Intraventricular hemorrhage (IVH) is a serious concern for preterm infants and can predispose such infants to brain injury and poor neurodevelopmental outcomes. IVH is particularly common in preterm infants. Although advances in obstetric management and neonatal care have led to a lower mortality rate for preterm infants with IVH, the IVH-related morbidity rate in this population remains high. Therefore, the present review investigated the pathophysiology of IVH and the evidence related to interventions for prevention. The analysis of the pathophysiology of IVH was conducted with a focus on the factors associated with cerebral hemodynamics, vulnerabilities in the structure of cerebral vessels, and host or genetic predisposing factors. The findings presented in the literature indicate that fluctuations in cerebral blood flow, the presence of hemodynamic significant patent ductus arteriosus, arterial carbon dioxide tension, and impaired cerebral venous drainage; a vulnerable or fragile capillary network; and a genetic variant associated with a mechanism underlying IVH development may lead to preterm infants developing IVH. Therefore, strategies focused on antenatal management, such as routine corticosteroid administration and magnesium sulfate use; perinatal management, such as maternal transfer to a specialized center; and postnatal management, including pharmacological agent administration and circulatory management involving prevention of extreme blood pressure, hemodynamic significant patent ductus arteriosus management, and optimization of cardiac function, can lower the likelihood of IVH development in preterm infants. Incorporating neuroprotective care bundles into routine care for such infants may also reduce the likelihood of IVH development. The findings regarding the pathogenesis of IVH further indicate that cerebrovascular status and systemic hemodynamic changes must be analyzed and monitored in preterm infants and that individualized management strategies must be developed with consideration of the risk factors for and physiological status of each preterm infant.
Figure
Cited by 1 articles
-
Editor’s Pick in May 2023
Chae-Yong Kim, Seung-Ki Kim
J Korean Neurosurg Soc. 2023;66(3):223-224. doi: 10.3340/jkns.2023.0079.
Reference
-
References
1. Al-Matary A, Abu Shaheen A, Abozaid S. Use of prophylactic indomethacin in preterm infants: a systematic review and meta-analysis. Front Pediatr. 10:760029. 2022.
Article2. Alotaibi WSM, Alsaif NS, Ahmed IA, Mahmoud AF, Ali K, Hammad A, et al. Reduction of severe intraventricular hemorrhage, a tertiary singlecenter experience: incidence trends, associated risk factors, and hospital policy. Childs Nerv Syst. 36:2971–2979. 2020.
Article3. Altaany D, Natarajan G, Gupta D, Zidan M, Chawla S. Severe intraventricular hemorrhage in extremely premature infants: are high carbon dioxide pressure or fluctuations the culprit? Am J Perinatol. 32:839–844. 2015.
Article4. Aly S, El-Dib M, Lu Z, El Tatawy S, Mohamed M, Aly H. Factors affecting cerebrovascular reactivity to CO2 in premature infants. J Perinat Med. 47:979–985. 2019.
Article5. American College of Obstetricians and Gynecologists; Society for Maternal-Fetal Medicine. Obstetric care consensus No. 6: periviable birth. Obstet Gynecol. 130:e187–e199. 2017.6. Auerbach A, Eventov-Friedman S, Arad I, Peleg O, Bdolah-Abram T, BarOz B, et al. Long duration of hyperglycemia in the first 96 hours of life is associated with severe intraventricular hemorrhage in preterm infants. J Pediatr. 163:388–393. 2013.
Article7. Ayed M, Ahmed J, More K, Ayed A, Husain H, AlQurashi A, et al. Antenatal magnesium sulfate for preterm neuroprotection: a single-center experience from Kuwait Tertiary NICU. Biomed Hub. 7:80–87. 2022.
Article8. Balasubramanian H, Ananthan A, Jain V, Rao SC, Kabra N. Umbilical cord milking in preterm infants: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 105:572–580. 2020.
Article9. Bansal V, Desai A. Efficacy of antenatal magnesium sulfate for neuroprotection in extreme prematurity: a comparative observational study. J Obstet Gynaecol India. 72:36–47. 2022.
Article10. Bates S, Odd D, Luyt K, Mannix P, Wach R, Evans D, et al. Superior vena cava flow and intraventricular haemorrhage in extremely preterm infants. J Matern Fetal Neonatal Med. 29:1581–1587. 2016.
Article11. Baumgartner S, Olischar M, Wald M, Werther T, Berger A, Waldhor T, et al. Left ventricular pumping during the transition-adaptation sequence in preterm infants: impact of the patent ductus arteriosus. Pediatr Res. 83:1016–1023. 2018.
Article12. Borna H, Rad SM, Borna S, Mohseni SM. Incidence of and risk factors for birth trauma in Iran. Taiwan J Obstet Gynecol. 49:170–173. 2010.
Article13. Brunner B, Hoeck M, Schermer E, Streif W, Kiechl-Kohlendorfer U. Patent ductus arteriosus, low platelets, cyclooxygenase inhibitors, and intraventricular hemorrhage in very low birth weight preterm infants. J Pediatr. 163:23–28. 2013.
Article14. Castrodale V, Rinehart S. The golden hour: improving the stabilization of the very low birth-weight infant. Adv Neonatal Care. 14:9–14. quiz 15-16. 2014.15. Cayabyab R, McLean CW, Seri I. Definition of hypotension and assessment of hemodynamics in the preterm neonate. J Perinatol 29 Suppl. 2:S58–S62. 2009.
Article16. Chen X, Li X, Chang Y, Li W, Cui H. Effect and safety of timing of cord clamping on neonatal hematocrit values and clinical outcomes in term infants: a randomized controlled trial. J Perinatol. 38:251–257. 2018.
Article17. Chock VY, Ramamoorthy C, Van Meurs KP. Cerebral autoregulation in neonates with a hemodynamically significant patent ductus arteriosus. J Pediatr. 160:936–942. 2012.
Article18. Christian EA, Jin DL, Attenello F, Wen T, Cen S, Mack WJ, et al. Trends in hospitalization of preterm infants with intraventricular hemorrhage and hydrocephalus in the United States, 2000-2010. J Neurosurg Pediatr. 17:260–269. 2016.
Article19. Ciccone MM, Scicchitano P, Zito A, Gesualdo M, Sassara M, Calderoni G, et al. Different functional cardiac characteristics observed in term/preterm neonates by echocardiography and tissue doppler imaging. Early Hum Dev. 87:555–558. 2011.20. Cools F, Offringa M, Askie LM. Elective high frequency oscillatory ventilation versus conventional ventilation for acute pulmonary dysfunction in preterm infants. Cochrane Database Syst Rev. (3):CD000104. 2015.
Article21. Costa STB, Costa P, Graca AM, Abrantes M; Portuguese National Registry of very low birth weight infants. Delivery mode and neurological complications in very low birth weight infants. Am J Perinatol. 2022; [Epub ahead of print].
Article22. da Costa CS, Czosnyka M, Smielewski P, Austin T. Optimal mean arterial blood pressure in extremely preterm infants within the first 24 hours of life. J Pediatr. 203:242–248. 2018.
Article23. de Bijl-Marcus K, Brouwer AJ, De Vries LS, Groenendaal F, Wezel-Meijler GV. Neonatal care bundles are associated with a reduction in the incidence of intraventricular haemorrhage in preterm infants: a multicentre cohort study. Arch Dis Child Fetal Neonatal Ed. 105:419–424. 2020.
Article24. de Figueiredo Vinagre LE, de Siqueira Caldas JP, Martins Marba ST, Procianoy RS, de Cassia Silveira R, Santiago Rego MA, et al. Temporal trends in intraventricular hemorrhage in preterm infants: a Brazilian multicenter cohort. Eur J Paediatr Neurol. 39:65–73. 2022.
Article25. Dempsey EM. What should we do about low blood pressure in preterm infants. Neonatology. 111:402–407. 2017.
Article26. Dempsey EM, Al Hazzani F, Barrington KJ. Permissive hypotension in the extremely low birthweight infant with signs of good perfusion. Arch Dis Child Fetal Neonatal Ed. 94:F241–244. 2009.
Article27. Dempsey EM, Barrington KJ. Diagnostic criteria and therapeutic interventions for the hypotensive very low birth weight infant. J Perinatol. 26:677–681. 2006.
Article28. Dix L, Molenschot M, Breur J, de Vries W, Vijlbrief D, Groenendaal F, et al. Cerebral oxygenation and echocardiographic parameters in preterm neonates with a patent ductus arteriosus: an observational study. Arch Dis Child Fetal Neonatal Ed. 101:F520–F526. 2016.
Article29. Dzietko M, Schulz S, Preuss M, Haertel C, Stein A, Felderhoff-Mueser U, et al. Apolipoprotein E gene polymorphisms and intraventricular haemorrhage in infants born preterm: a large prospective multicentre cohort study. Dev Med Child Neurol. 61:337–342. 2019.
Article30. Egesa WI, Odoch S, Odong RJ, Nakalema G, Asiimwe D, Ekuk E, et al. Germinal matrix-intraventricular hemorrhage: a tale of preterm infants. Int J Pediatr. 2021:6622598. 2021.
Article31. Erickson SJ, Grauaug A, Gurrin L, Swaminathan M. Hypocarbia in the ventilated preterm infant and its effect on intraventricular haemorrhage and bronchopulmonary dysplasia. J Paediatr Child Health. 38:560–562. 2002.
Article32. Evans N, Kluckow M. Early ductal shunting and intraventricular haemorrhage in ventilated preterm infants. Arch Dis Child Fetal Neonatal Ed. 75:F183–186. 1996.
Article33. Fabres J, Carlo WA, Phillips V, Howard G, Ambalavanan N. Both extremes of arterial carbon dioxide pressure and the magnitude of fluctuations in arterial carbon dioxide pressure are associated with severe intraventricular hemorrhage in preterm infants. Pediatrics. 119:299–305. 2007.
Article34. Ferreira DM, Girao ALA, AVS ES, Chaves EMC, de Almeida PC, Freire VS, et al. Application of a bundle in the prevention of peri-intraventricular hemorrhage in preterm newborns. J Perinat Neonatal Nurs. 34:E5–E11. 2020.
Article35. Fogarty M, Osborn DA, Askie L, Seidler AL, Hunter K, Lui K, et al. Delayed vs early umbilical cord clamping for preterm infants: a systematic review and meta-analysis. Am J Obstet Gynecol. 218:1–18. 2018.
Article36. Fortmann I, Mertens L, Boeckel H, Gruttner B, Humberg A, Astiz M, et al. A timely administration of antenatal steroids is highly protective against intraventricular hemorrhage: an observational multicenter cohort study of very low birth weight infants. Front Pediatr. 10:721355. 2022.
Article37. Friedman WF. The intrinsic physiologic properties of the developing heart. Prog Cardiovasc Dis. 15:87–111. 1972.
Article38. Gamaleldin I, Harding D, Siassakos D, Draycott T, Odd D. Significant intraventricular hemorrhage is more likely in very preterm infants born by vaginal delivery: a multi-centre retrospective cohort study. J Matern Fetal Neonatal Med. 32:477–482. 2019.
Article39. Gross M, Engel C, Trotter A. Evaluating the effect of a neonatal care bundle for the prevention of intraventricular hemorrhage in preterm infants. Children (Basel). 8:257. 2021.
Article40. Hamrick SEG, Sallmon H, Rose AT, Porras D, Shelton EL, Reese J, et al. Patent ductus arteriosus of the preterm infant. Pediatrics. 146:e20201209. 2020.
Article41. Hatfield LA, Murphy N, Karp K, Polomano RC. A systematic review of behavioral and environmental interventions for procedural pain management in preterm infants. J Pediatr Nurs. 44:22–30. 2019.
Article42. Helwich E, Rutkowska M, Bokiniec R, Gulczynska E, Hozejowski R. Intraventricular hemorrhage in premature infants with Respiratory Distress Syndrome treated with surfactant: incidence and risk factors in the prospective cohort study. Dev Period Med. 21:328–335. 2017.43. Hemmati F, Sharma D, Namavar Jahromi B, Salarian L, Farahbakhsh N. Delayed cord clamping for prevention of intraventricular hemorrhage in preterm neonates: a randomized control trial. J Matern Fetal Neonatal Med. 35:3633–3639. 2022.
Article44. Hübner ME, Ramirez R, Burgos J, Dominguez A, Tapia JL. Mode of delivery and antenatal steroids and their association with survival and severe intraventricular hemorrhage in very low birth weight infants. J Perinatol. 36:832–836. 2016.
Article45. Humberg A, Härtel C, Paul P, Hanke K, Bossung V, Hartz A, et al. Delivery mode and intraventricular hemorrhage risk in very-low-birth-weight infants: observational data of the German Neonatal Network. Eur J Obstet Gynecol Reprod Biol. 212:144–149. 2017.
Article46. Ikeda T, Ito Y, Mikami R, Matsuo K, Kawamura N, Yamoto A, et al. Fluctuations in internal cerebral vein and central side veins of preterm infants. Pediatr Int. 63:1319–1326. 2021.
Article47. Jelin AC, Zlatnik MG, Kuppermann M, Gregorich SE, Nakagawa S, Clyman R. Clamp late and maintain perfusion (CLAMP) policy: delayed cord clamping in preterm infants. J Matern Fetal Neonatal Med. 29:1705–1709. 2016.
Article48. Jim WT, Chiu NC, Chen MR, Hung HY, Kao HA, Hsu CH, et al. Cerebral hemodynamic change and intraventricular hemorrhage in very low birth weight infants with patent ductus arteriosus. Ultrasound Med Biol. 31:197–202. 2005.
Article49. Kaiser JR, Gauss CH, Pont MM, Williams DK. Hypercapnia during the first 3 days of life is associated with severe intraventricular hemorrhage in very low birth weight infants. J Perinatol. 26:279–285. 2006.
Article50. Kalani M, Shariat M, Khalesi N, Farahani Z, Ahmadi S. A comparison of early ibuprofen and indomethacin administration to prevent intraventricular hemorrhage among preterm infants. Acta Med Iran. 54:788–792. 2016.51. Karagol BS, Calisici E, Zeybek C, Unay B, Yuksel S. The impact of initial hematocrit values after birth on peri-/intraventricular hemorrhage in extremely low birth weight neonates. Childs Nerv Syst. 38:109–114. 2022.
Article52. Katheria AC, Szychowski JM, Essers J, Mendler MR, Dempsey EM, Schmolzer GM, et al. Early cardiac and cerebral hemodynamics with umbilical cord milking compared with delayed cord clamping in infants born preterm. J Pediatr. 223:51–56.e1. 2020.
Article53. Kc A, Malqvist M, Rana N, Ranneberg LJ, Andersson O. Effect of timing of umbilical cord clamping on anaemia at 8 and 12 months and later neurodevelopment in late pre-term and term infants; a facility-based, randomized-controlled trial in Nepal. BMC Pediatr. 16:35. 2016.
Article54. Khanafer-Larocque I, Soraisham A, Stritzke A, Al Awad E, Thomas S, Murthy P, et al. Intraventricular hemorrhage: risk factors and association with patent ductus arteriosus treatment in extremely preterm neonates. Front Pediatr. 7:408. 2019.
Article55. Klingenberg C, Wheeler KI, McCallion N, Morley CJ, Davis PG. Volume-targeted versus pressure-limited ventilation in neonates. Cochrane Database Syst Rev. 10:CD003666. 2017.
Article56. Kluckow M. The pathophysiology of low systemic blood flow in the preterm infant. Front Pediatr. 6:29. 2018.
Article57. Kluckow M, Evans N. Low superior vena cava flow and intraventricular haemorrhage in preterm infants. Arch Dis Child Fetal Neonatal Ed. 82:F188–194. 2000.
Article58. Kochan M, Leonardi B, Firestine A, McPadden J, Cobb D, Shah TA, et al. Elevated midline head positioning of extremely low birth weight infants: effects on cardiopulmonary function and the incidence of periventricular-intraventricular hemorrhage. J Perinatol. 39:54–62. 2019.
Article59. Kooi EMW, Richter AE. Cerebral autoregulation in sick infants: current insights. Clin Perinatol. 47:449–467. 2020.60. Kooi EMW, Verhagen EA, Elting JWJ, Czosnyka M, Austin T, Wong FY, et al. Measuring cerebrovascular autoregulation in preterm infants using near-infrared spectroscopy: an overview of the literature. Expert Rev Neurother. 17:801–818. 2017.
Article61. Kumar Nair PA, Pai MG, Gazal HA, Da Costa DE, Al Khusaiby SM. Indomethacin prophylaxis for intraventricular hemorrhage in very low birth weight babies. Indian Pediatr. 41:551–558. 2004.62. Leviton A, Fenton T, Kuban KC, Pagano M. Labor and delivery characteristics and the risk of germinal matrix hemorrhage in low birth weight infants. J Child Neurol. 6:35–40. 1991.
Article63. Lightburn MH, Gauss CH, Williams DK, Kaiser JR. Cerebral blood flow velocities in extremely low birth weight infants with hypotension and infants with normal blood pressure. J Pediatr. 154:824–828. 2009.
Article64. Ljustina S, Berisavac M, Kovacević-Vukolić L, VelickovićAleksić V, Marković N. Analysis of intracranial hemorrhage grade in preterm singleton pregnancies delivered vaginally or by cesarean section. Vojnosanit Pregl. 70:255–258. 2013.
Article65. Lou HC, Lassen NA, Friis-Hansen B. Impaired autoregulation of cerebral blood flow in the distressed newborn infant. J Pediatr. 94:118–121. 1979.
Article66. Luca A, Vinturache A, Ilea C, Avasiloaiei A, Paduraru L, Carauleanu A, et al. Birth trauma in preterm spontaneous vaginal and cesarean section deliveries: a 10-years retrospective study. PLoS One. 17:e0275726. 2022.
Article67. Martini S, Czosnyka M, Smielewski P, Iommi M, Galletti S, Vitali F, et al. Clinical determinants of cerebrovascular reactivity in very preterm infants during the transitional period. Pediatr Res. 92:135–141. 2022.
Article68. McGoldrick E, Stewart F, Parker R, Dalziel SR. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 12:CD004454. 2020.
Article69. McLendon D, Check J, Carteaux P, Michael L, Moehring J, Secrest JW, et al. Implementation of potentially better practices for the prevention of brain hemorrhage and ischemic brain injury in very low birth weight infants. Pediatrics. 111(4 Pt 2):e497–503. 2003.
Article70. Ment LR, Oh W, Ehrenkranz RA, Philip AG, Duncan CC, Makuch RW. Antenatal steroids, delivery mode, and intraventricular hemorrhage in preterm infants. Am J Obstet Gynecol. 172:795–800. 1995.
Article71. Ment LR, Oh W, Ehrenkranz RA, Philip AG, Vohr B, Allan W, et al. Lowdose indomethacin and prevention of intraventricular hemorrhage: a multicenter randomized trial. Pediatrics. 93:543–550. 1994.
Article72. Miller CJ, Prusakov P, Magers J, Speaks S, Sacic H, Escobar K, et al. Effects of prophylactic indomethacin on intraventricular hemorrhage and adverse outcomes in neonatal intensive care unit. J Perinatol. 42:1644–1648. 2022.
Article73. Mitra S, Florez ID, Tamayo ME, Mbuagbaw L, Vanniyasingam T, Veroniki AA, et al. Association of placebo, indomethacin, ibuprofen, and acetaminophen with closure of hemodynamically significant patent ductus arteriosus in preterm infants: a systematic review and meta-analysis. JAMA. 319:1221–1238. 2018.
Article74. Mittendorf R, Besinger R, Santillan M, Gianopoulos J. When used in the circumstance of preterm labor, is there a paradoxical effect of varying exposures to magnesium sulfate (MgSO4) on the developing human brain? Am J Obstet Gynecol. 193(6 Suppl):S65. 2005.
Article75. Mittendorf R, Dambrosia J, Dammann O, Pryde PG, Lee KS, Ben-Ami TE, et al. Association between maternal serum ionized magnesium levels at delivery and neonatal intraventricular hemorrhage. J Pediatr. 140:540–546. 2002.
Article76. Moriette G, Paris-Llado J, Walti H, Escande B, Magny JF, Cambonie G, et al. Prospective randomized multicenter comparison of high-frequency oscillatory ventilation and conventional ventilation in preterm infants of less than 30 weeks with respiratory distress syndrome. Pediatrics. 107:363–372. 2001.
Article77. Mullaart RA, Hopman JC, Rotteveel JJ, Stoelinga GB, De Haan AF, Daniels O. Cerebral blood flow velocity and pulsation in neonatal respiratory distress syndrome and periventricular hemorrhage. Pediatr Neurol. 16:118–125. 1997.
Article78. Noone MA, Sellwood M, Meek JH, Wyatt JS. Postnatal adaptation of cerebral blood flow using near infrared spectroscopy in extremely preterm infants undergoing high-frequency oscillatory ventilation. Acta Paediatr. 92:1079–1084. 2003.
Article79. Noori S, Seri I. Hemodynamic antecedents of peri/intraventricular hemorrhage in very preterm neonates. Semin Fetal Neonatal Med. 20:232–237. 2015.
Article80. Ohlsson A, Shah PS. Paracetamol (acetaminophen) for patent ductus arteriosus in preterm or low birth weight infants. Cochrane Database Syst Rev. 4:CD010061. 2018.
Article81. Okulu E, Haskologlu S, Guloglu D, Kostekci E, Erdeve O, Atasay B, et al. Effects of umbilical cord management strategies on stem cell transfusion, delivery room adaptation, and cerebral oxygenation in term and late preterm infants. Front Pediatr. 10:838444. 2022.82. Pan I, Shah PA, Singh J, Kelly KN, Bondi DS. Comparison of neonatal outcomes with and without prophylaxis with indomethacin in premature neonates. J Pediatr Pharmacol Ther. 26:478–483. 2021.
Article83. Panerai RB, Kelsall AW, Rennie JM, Evans DH. Cerebral autoregulation dynamics in premature newborns. Stroke. 26:74–80. 1995.
Article84. Parker LA. Part 1: early recognition and treatment of birth trauma: injuries to the head and face. Adv Neonatal Care. 5:288–297. quiz 298-300. 2005.85. Persad N, Kelly E, Amaral N, Neish A, Cheng C, Fan CS, et al. Impact of a "Brain Protection Bundle" in reducing severe intraventricular hemorrhage in preterm infants <30 weeks GA: a retrospective single centre study. Children (Basel). 8:983. 2021.
Article86. Pinto Cardoso G, Houivet E, Marchand-Martin L, Kayem G, Sentilhes L, Ancel PY, et al. Association of intraventricular hemorrhage and death with tocolytic exposure in preterm infants. JAMA Netw Open. 1:e182355. 2018.
Article87. Pishva N, Parsa G, Saki F, Saki M, Saki MR. Intraventricular hemorrhage in premature infants and its association with pneumothorax. Acta Med Iran. 50:473–476. 2012.88. Piteaud I, Abdennour L, Icke C, Stany I, Lescot T, Puybasset L. Superior vena cava syndrome: cause of secondary raise of intracranial pressure after traumatic brain injury. Ann Fr Anesth Reanim. 27:850–853. 2008.89. Poryo M, Boeckh JC, Gortner L, Zemlin M, Duppre P, Ebrahimi-Fakhari D, et al. Ante-, peri- and postnatal factors associated with intraventricular hemorrhage in very premature infants. Early Hum Dev. 116:1–8. 2018.
Article90. Rahman S, Ullah M, Ali A, Afridi N, Bashir H, Amjad Z, et al. Fetal outcomes in preterm cesarean sections. Cureus. 14:e27607. 2022.
Article91. Raybaud C. Normal and abnormal embryology and development of the intracranial vascular system. Neurosurg Clin N Am. 21:399–426. 2010.
Article92. Rhee CJ, Fraser CD 3rd, Kibler K, Easley RB, Andropoulos DB, Czosnyka M, et al. The ontogeny of cerebrovascular pressure autoregulation in premature infants. J Perinatol. 34:926–931. 2014.
Article93. Riskin A, Riskin-Mashiah S, Bader D, Kugelman A, Lerner-Geva L, Boyko V, et al. Delivery mode and severe intraventricular hemorrhage in single, very low birth weight, vertex infants. Obstet Gynecol. 112:21–28. 2008.
Article94. Rozé JC, Cambonie G, Marchand-Martin L, Gournay V, Durrmeyer X, Durox M, et al. Association between early screening for patent ductus arteriosus and in-hospital mortality among extremely preterm infants. JAMA. 313:2441–2448. 2015.
Article95. Sankar MN, Bhombal S, Benitz WE. PDA: to treat or not to treat. Congenit Heart Dis. 14:46–51. 2019.
Article96. Schreiner C, Suter S, Watzka M, Hertfelder HJ, Schreiner F, Oldenburg J, et al. Genetic variants of the vitamin K dependent coagulation system and intraventricular hemorrhage in preterm infants. BMC Pediatr. 14:219. 2014.
Article97. Schulz G, Keller E, Haensse D, Arlettaz R, Bucher HU, Fauchere JC. Slow blood sampling from an umbilical artery catheter prevents a decrease in cerebral oxygenation in the preterm newborn. Pediatrics. 111:e73–76. 2003.
Article98. Semberova J, Sirc J, Miletin J, Kucera J, Berka I, Sebkova S, et al. Spontaneous closure of patent ductus arteriosus in infants ≤1500 g. Pediatrics. 140:e20164258. 2017.
Article99. Seri I. Management of hypotension and low systemic blood flow in the very low birth weight neonate during the first postnatal week. J Perinatol 26 Suppl. 1:S8–S13. discussion S22-S23. 2006.
Article100. Shah V, Hodgson K, Seshia M, Dunn M, Schmolzer GM. Golden hour management practices for infants <32 weeks gestational age in Canada. Paediatr Child Health. 23:e70–e76. 2018.
Article101. Soul JS, Hammer PE, Tsuji M, Saul JP, Bassan H, Limperopoulos C, et al. Fluctuating pressure-passivity is common in the cerebral circulation of sick premature infants. Pediatr Res. 61:467–473. 2007.
Article102. Su BH, Lin HY, Chiu HY, Tsai ML, Chen YT, Lu IC. Therapeutic strategy of patent ductus arteriosus in extremely preterm infants. Pediatr Neonatol. 61:133–141. 2020.
Article103. Szpecht D, Al-Saad SR, Karbowski LM, Kosik K, Kurzawińska G, Szymankiewicz M, et al. Role of fibronectin-1 polymorphism genes with the pathogenesis of intraventricular hemorrhage in preterm infants. Childs Nerv Syst. 36:1729–1736. 2020.
Article104. Szpecht D, Gadzinowski J, Seremak-Mrozikiewicz A, Kurzawińska G, Drews K, Szymankiewicz M. The significance of polymorphisms in genes encoding Il-1β, Il-6, TNFα, and Il-1RN in the pathogenesis of intraventricular hemorrhage in preterm infants. Childs Nerv Syst. 33:1905–1916. 2017.
Article105. Szpecht D, Gadzinowski J, Seremak-Mrozikiewicz A, Kurzawińska G, Szymankiewicz M. Role of endothelial nitric oxide synthase and endothelin-1 polymorphism genes with the pathogenesis of intraventricular hemorrhage in preterm infants. Sci Rep. 7:42541. 2017.
Article106. Takahashi Y, Harada K, Kishkurno S, Arai H, Ishida A, Takada G. Postnatal left ventricular contractility in very low birth weight infants. Pediatr Cardiol. 18:112–117. 1997.
Article107. Thewissen L, Naulaers G, Hendrikx D, Caicedo A, Barrington K, Boylan G, et al. Cerebral oxygen saturation and autoregulation during hypotension in extremely preterm infants. Pediatr Res. 90:373–380. 2021.
Article108. Thornburg CD, Erickson SW, Page GP, Clark EAS, DeAngelis MM, Hartnett ME, et al. Genetic predictors of severe intraventricular hemorrhage in extremely low-birthweight infants. J Perinatol. 41:286–294. 2021.
Article109. Toledo JD, Rodilla S, Perez-Iranzo A, Delgado A, Maazouzi Y, Vento M. Umbilical cord milking reduces the risk of intraventricular hemorrhage in preterm infants born before 32 weeks of gestation. J Perinatol. 39:547–553. 2019.
Article110. Tomotaki S, Iwanaga K, Hanaoka S, Tomotaki H, Matsukura T, Niwa F, et al. Antenatal glucocorticoids reduce the incidence of refractory hypotension in low birthweight infants during the early neonatal period, but do not affect it beyond this time. Am J Perinatol. 38:1057–1061. 2021.
Article111. Toyoshima K, Kawataki M, Ohyama M, Shibasaki J, Yamaguchi N, Hoshino R, et al. Tailor-made circulatory management based on the stress-velocity relationship in preterm infants. J Formos Med Assoc. 112:510–517. 2013.
Article112. Tsuji M, Saul JP, du Plessis A, Eichenwald E, Sobh J, Crocker R, et al. Cerebral intravascular oxygenation correlates with mean arterial pressure in critically ill premature infants. Pediatrics. 106:625–632. 2000.
Article113. van Beek PE, Groenendaal F, Broeders L, Dijk PH, Dijkman KP, van den Dungen FAM, et al. Survival and causes of death in extremely preterm infants in the Netherlands. Arch Dis Child Fetal Neonatal Ed. 106:251–257. 2021.
Article114. van Bel F, Mintzer JP. Monitoring cerebral oxygenation of the immature brain: a neuroprotective strategy? Pediatr Res. 84:159–164. 2018.
Article115. van der Laan ME, Roofthooft MT, Fries MW, Berger RM, Schat TE, van Zoonen AG, et al. A hemodynamically significant patent ductus arteriosus does not affect cerebral or renal tissue oxygenation in preterm infants. Neonatology. 110:141–147. 2016.
Article116. Verma PK, Panerai RB, Rennie JM, Evans DH. Grading of cerebral autoregulation in preterm and term neonates. Pediatr Neurol. 23:236–242. 2000.
Article117. Vesoulis ZA, Flower AA, Zanelli S, Rambhia A, Abubakar M, Whitehead HV, et al. Blood pressure extremes and severe IVH in preterm infants. Pediatr Res. 87:69–73. 2020.
Article118. Vesoulis ZA, Liao SM, Mathur AM. Gestational age-dependent relationship between cerebral oxygen extraction and blood pressure. Pediatr Res. 82:934–939. 2017.
Article119. Vinukonda G, Dummula K, Malik S, Hu F, Thompson CI, Csiszar A, et al. Effect of prenatal glucocorticoids on cerebral vasculature of the developing brain. Stroke. 41:1766–1773. 2010.
Article120. Wardle SP, Yoxall CW, Weindling AM. Determinants of cerebral fractional oxygen extraction using near infrared spectroscopy in preterm neonates. J Cereb Blood Flow Metab. 20:272–279. 2000.
Article121. Wei JC, Catalano R, Profit J, Gould JB, Lee HC. Impact of antenatal steroids on intraventricular hemorrhage in very-low-birth weight infants. J Perinatol. 36:352–356. 2016.
Article122. Wolf HT, Weber T, Schmidt S, Norman M, Varendi H, Piedvache A, et al. Mode of delivery and adverse short- and long-term outcomes in vertex-presenting very preterm born infants: a European populationbased prospective cohort study. J Perinat Med. 49:923–931. 2021.
Article123. Wong FY, Leung TS, Austin T, Wilkinson M, Meek JH, Wyatt JS, et al. Impaired autoregulation in preterm infants identified by using spatially resolved spectroscopy. Pediatrics. 121:e604–e611. 2008.
Article124. Xu H, Hu F, Sado Y, Ninomiya Y, Borza DB, Ungvari Z, et al. Maturational changes in laminin, fibronectin, collagen IV, and perlecan in germinal matrix, cortex, and white matter and effect of betamethasone. J Neurosci Res. 86:1482–1500. 2008.
Article125. Yao SL, Smit E, Odd D. The effectiveness of interventions to prevent intraventricular haemorrhage in premature infants: a systematic review and network meta-analysis. J Neonatal Perinatal Med. 16:5–20. 2023.
Article126. Committee Opinion No. 455. magnesium sulfate before anticipated preterm birth for neuroprotection. Obstet Gynecol. 115:669–671. 2010.127. Committee Opinion No 652. magnesium sulfate use in obstetrics. Obstet Gynecol. 127:e52–e53. 2016.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fibrinolytic (Thrombolytic) Therapy for Post Intraventricular Hemorrhagic Hydrocephalus in Preterm Infants
- Pharmacological Management of Germinal Matrix-Intraventricular Hemorrhage
- Neurodevelopmental Outcomes and Brain Volumetric Analysis of Low-Grade Intraventricular Hemorrhage
- Perspectives : Understanding the Pathophysiology of Intraventricular Hemorrhage in Preterm Infants and Considering of the Future Direction for Treatment
- Effect of Indomethacin Therpy on Prevention of Intraventricular Hemorrhage in Very