Intest Res.
2023 Apr;21(2):235-243. 10.5217/ir.2022.00012.
Laparoscopic surgery contributes to a decrease in short-term complications in surgical ulcerative colitis patients during 2008–2017: a multicenter retrospective study in China
- Affiliations
-
- 1Department of Colorectal Surgery, Guangdong Institute of Gastroenterology, Guangdong Provincial Key Laboratory of Colorectal and Pelvic Floor Diseases, The Sixth Affiliated Hospital, Sun Yat-sen University, Guangzhou, China
- 2Department of General Surgery, Jinling Hospital, Medical School of Nanjing University, Nanjing, China
- 3Department of Colorectal Surgery, Xinhua Hospital, Shanghai Jiaotong University School of Medicine, Shanghai, China
- 4Department of Gastrointestinal Surgery, West China Hospital, Sichuan University, Chengdu, China
- 5Department of General Surgery, Sir Run Run Shaw Hospital, Zhejiang University School of Medicine, Hangzhou, China
- 6Department of General Surgery, Qilu Hospital, Shandong University, Jinan, China
- 7Department of General Surgery, Peking Union Medical College Hospital, Peking Union Medical College, Chinese Academy of Medical Sciences, Beijing, China
- 8Department of Colorectal Surgery, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, China
- 9Department of General Surgery, Nanfang Hospital, Southern Medical University, Guangzhou, China
- 10Department of General Surgery, Integrated Hospital of Traditional Chinese Medicine, Southern Medical University, Guangzhou, China
- 11Department of Geriatric Surgery, The Second Xiangya Hospital, Central South University, Changsha, China
- 12Department of Colorectal Surgery, The First Affiliated Hospital, Zhejiang University College of Medicine, Hangzhou, China
- 13Department of Colorectal and Anal Surgery, The First Hospital of Jilin University, Changchun, Jilin, China
- 14State Key Laboratory of Cancer Biology and Institute of Digestive Diseases, Xijing Hospital of Digestive Diseases, Xi’an, China
- KMID: 2541896
- DOI: http://doi.org/10.5217/ir.2022.00012
Abstract
- Background/Aims
The aim of this study was to analyze the chronological changes in postoperative complications in surgical ulcerative colitis patients over the past decade in China and to investigate the potential parameters that contributed to the changes.
Methods
Ulcerative colitis patients who underwent surgery during 2008–2017 were retrospectively enrolled from 13 hospitals in China. Postoperative complications were compared among different operation years. Risk factors for complications were identified by logistic regression analysis.
Results
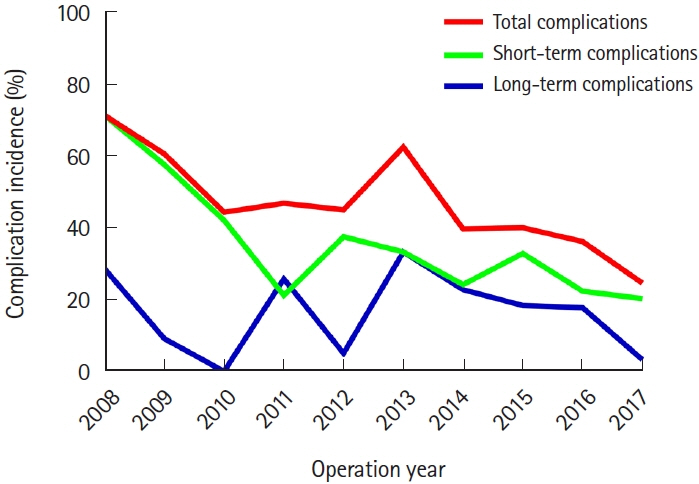
A total of 446 surgical ulcerative colitis patients were analyzed. Fewer short-term complications (24.8% vs. 41.0%, P=0.001) and more laparoscopic surgeries (66.4% vs. 25.0%, P<0.001) were found among patients who received surgery during 2014–2017 than 2008–2013. Logistic regression suggested that independent protective factors against short-term complications were a higher preoperative body mass index (odds ratio [OR], 0.870; 95% confidence interval [CI], 0.785–0.964; P=0.008), laparoscopic surgery (OR, 0.391; 95% CI, 0.217–0.705; P=0.002) and elective surgery (OR, 0.213; 95% CI, 0.067–0.675; P=0.009). The chronological decrease in short-term complications was associated with an increase in laparoscopic surgery.
Conclusions
Our data revealed a downward trend of short-term postoperative complications among surgical ulcerative colitis patients in China during the past decade, which may be due to the promotion of minimally invasive techniques among Chinese surgeons.
Keyword
Figure
Reference
-
1. Rubin DT, Ananthakrishnan AN, Siegel CA, Sauer BG, Long MD. ACG clinical guideline: ulcerative colitis in adults. Am J Gastroenterol. 2019; 114:384–413.
Article2. Hindryckx P, Jairath V, D’Haens G. Acute severe ulcerative colitis: from pathophysiology to clinical management. Nat Rev Gastroenterol Hepatol. 2016; 13:654–664.
Article3. Jeuring SF, Bours PH, Zeegers MP, et al. Disease outcome of ulcerative colitis in an era of changing treatment strategies: results from the Dutch population-based IBDSL cohort. J Crohns Colitis. 2015; 9:837–845.
Article4. Parragi L, Fournier N, Zeitz J, et al. Colectomy rates in ulcerative colitis are low and decreasing: 10-year follow-up data from the Swiss IBD cohort study. J Crohns Colitis. 2018; 12:811–818.5. Parks AG, Nicholls RJ. Proctocolectomy without ileostomy for ulcerative colitis. Br Med J. 1978; 2:85–88.
Article6. Fu W, Zhang T, Zhang Z. The application of total proctocolectomy and ileal pouch-anal anastomosis in the treatment of ulcerative colitis. Chin J Gastrointest Surg. 1999; 4:208–210.7. Han HQ, Liu G, Liu T, Lü YC, Fu Q. Clinical evaluation of restorative proctocolectomy with ileal pouch-anal anastomosis for ulcerative colitis. Zhonghua Yi Xue Za Zhi. 2011; 91:3205–3209.8. Cui L. Treatment of ulcerative colitis by total colectomy ileal pouch-anal anastomosis. Zhonghua Wei Chang Wai Ke Za Zhi. 2012; 15:1221–1223.9. Liu G, Han H, Liu T, Fu Q, Lyu Y. Clinical outcome of ileal pouchanal anastomosis for chronic ulcerative colitis in China. Chin Med J (Engl). 2014; 127:1497–1503.10. Candido FD, Fiorino G, Spadaccini M, Danese S, Spinelli A. Are surgical rates decreasing in the biological era in IBD? Curr Drug Targets. 2019; 20:1356–1362.
Article11. Wong DJ, Roth EM, Feuerstein JD, Poylin VY. Surgery in the age of biologics. Gastroenterol Rep (Oxf). 2019; 7:77–90.
Article12. Abelson JS, Michelassi F, Mao J, Sedrakyan A, Yeo H. Higher surgical morbidity for ulcerative colitis patients in the era of biologics. Ann Surg. 2018; 268:311–317.
Article13. Justiniano CF, Aquina CT, Becerra AZ, et al. Postoperative mortality after nonelective surgery for inflammatory bowel disease patients in the era of biologics. Ann Surg. 2019; 269:686–691.
Article14. Bikhchandani J, Polites SF, Wagie AE, Habermann EB, Cima RR. National trends of 3- versus 2-stage restorative proctocolectomy for chronic ulcerative colitis. Dis Colon Rectum. 2015; 58:199–204.
Article15. de Buck van Overstraeten A, Mark-Christensen A, Wasmann KA, et al. Transanal versus transabdominal minimally invasive (completion) proctectomy with ileal pouch-anal anastomosis in ulcerative colitis: a comparative study. Ann Surg. 2017; 266:878–883.16. Satsangi J, Silverberg MS, Vermeire S, Colombel JF. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006; 55:749–753.
Article17. Truelove SC, Witts LJ. Cortisone in ulcerative colitis; final report on a therapeutic trial. Br Med J. 1955; 2:1041–1048.18. Ng SC, Shi HY, Hamidi N, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2017; 390:2769–2778.
Article19. Ordás I, Domènech E, Mañosa M, et al. Post-operative morbidity and mortality of a cohort of steroid refractory acute severe ulcerative colitis: nationwide multicenter study of the GETECCU ENEIDA Registry. Am J Gastroenterol. 2018; 113:1009–1016.
Article20. Peyrin-Biroulet L, Germain A, Patel AS, Lindsay JO. Systematic review: outcomes and post-operative complications following colectomy for ulcerative colitis. Aliment Pharmacol Ther. 2016; 44:807–816.21. Yu Q, Mao R, Lian L, et al. Surgical management of inflammatory bowel disease in China: a systematic review of two decades. Intest Res. 2016; 14:322–332.
Article22. Masaki T, Kishiki T, Kojima K, Asou N, Beniya A, Matsuoka H. Recent trends (2016-2017) in the treatment of inflammatory bowel disease. Ann Gastroenterol Surg. 2018; 2:282–288.
Article23. Subramanian V, Saxena S, Kang JY, Pollok RC. Preoperative steroid use and risk of postoperative complications in patients with inflammatory bowel disease undergoing abdominal surgery. Am J Gastroenterol. 2008; 103:2373–2381.
Article24. Zittan E, Milgrom R, Ma GW, et al. Preoperative anti-tumor necrosis factor therapy in patients with ulcerative colitis is not associated with an increased risk of infectious and noninfectious complications after ileal pouch-anal anastomosis. Inflamm Bowel Dis. 2016; 22:2442–2447.
Article25. Kurnool S, Nguyen NH, Proudfoot J, et al. High body mass index is associated with increased risk of treatment failure and surgery in biologic-treated patients with ulcerative colitis. Aliment Pharmacol Ther. 2018; 47:1472–1479.
Article26. Wu XJ, He XS, Zhou XY, Zou YF, Lan P. Safety and feasibility of laparoscopic surgery and open surgery in ulcerative colitis: a meta-analysis. Zhonghua Wei Chang Wai Ke Za Zhi. 2008; 11:408–413.27. Causey MW, Stoddard D, Johnson EK, et al. Laparoscopy impacts outcomes favorably following colectomy for ulcerative colitis: a critical analysis of the ACS-NSQIP database. Surg Endosc. 2013; 27:603–609.
Article28. Tajti J Jr, Látos M, Farkas K, et al. Effect of laparoscopic surgery on quality of life in ulcerative colitis. J Laparoendosc Adv Surg Tech A. 2018; 28:833–838.
Article29. Mège D, Figueiredo MN, Manceau G, Maggiori L, Bouhnik Y, Panis Y. Three-stage laparoscopic ileal pouch-anal anastomosis is the best approach for high-risk patients with inflammatory bowel disease: an analysis of 185 consecutive patients. J Crohns Colitis. 2016; 10:898–904.
Article30. Lee GC, Deery SE, Kunitake H, et al. Comparable perioperative outcomes, long-term outcomes, and quality of life in a retrospective analysis of ulcerative colitis patients following 2-stage versus 3-stage proctocolectomy with ileal pouch-anal anastomosis. Int J Colorectal Dis. 2019; 34:491–499.
Article31. Lavryk OA, Stocchi L, Hull TL, et al. Impact of preoperative duration of ulcerative colitis on long-term outcomes of restorative proctocolectomy. Int J Colorectal Dis. 2020; 35:41–49.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Operative Outcomes of Open versus Laparoscopic Total Proctocolectomy with Ileal Pouch Anal Anastomosis in Ulcerative Colitis
- Surgical Options for Appropriate Length of J-Pouch Construction for Better Outcomes and Long-term Quality of Life in Patients with Ulcerative Colitis after Ileal Pouch-Anal Anastomosis
- A Comprehensive Review of Inflammatory Bowel Disease Focusing on Surgical Management
- Short-term Outcomes of Elective 2-Stage Restorative Proctocolectomy for Ulcerative Colitis in Korea: Does Laparoscopy Have Benefits?
- Advances in ulcerative colitis therapy