Ann Clin Neurophysiol.
2023;25(1):1-9. 10.14253/acn.2023.25.1.1.
Application of respiratory function tests in patients with neurological diseases
- Affiliations
-
- 1Department of Neurology, Nowon Eulji Medical Center, Eulji University School of Medicine, Seoul, Korea
- 2Department of Neurology, Seoul National University Hospital, Seoul, Korea
- 3Center for Hospital Medicine, Seoul National University Hospital, Seoul, Korea
- 4Neuroscience Research Institute, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2541816
- DOI: http://doi.org/10.14253/acn.2023.25.1.1
Abstract
- Breathing is controlled by complex interactions between the central and peripheral nervous systems in conjunction with the respiratory system. Neurological diseases predispose patients to nocturnal desaturation and pneumonia due to respiratory dysfunction, which increases mortality, daytime sleepiness and fatigue, and reduces the quality of life. Respiratory function tests are required to identify respiratory function decline and to consider compensatory management. This review summarizes the characteristics of several respiratory function tests and their applications to neurological diseases.
Figure
Reference
-
1. Vaporidi K, Akoumianaki E, Telias I, Goligher EC, Brochard L, Georgopoulos D. Respiratory drive in critically ill patients. Pathophysiology and clinical implications. Am J Respir Crit Care Med. 2020; 201:20–32.
Article2. Ikeda K, Kawakami K, Onimaru H, Okada Y, Yokota S, Koshiya N, et al. The respiratory control mechanisms in the brainstem and spinal cord: integrative views of the neuroanatomy and neurophysiology. J Physiol Sci. 2017; 67:45–62.
Article3. Routal RV, Pal GP. Location of the phrenic nucleus in the human spinal cord. J Anat. 1999; 195:617–621.
Article4. Polkey MI, Lyall RA, Moxham J, Leigh PN. Respiratory aspects of neurological disease. J Neurol Neurosurg Psychiatry. 1999; 66:5–15.
Article5. Mellies U, Dohna-Schwake C, Voit T. Respiratory function assessment and intervention in neuromuscular disorders. Curr Opin Neurol. 2005; 18:543–547.
Article6. Howard RS. Respiratory failure because of neuromuscular disease. Curr Opin Neurol. 2016; 29:592–601.
Article7. Diebold D. Management of respiratory complications in neuromuscular weakness. Clin Pulm Med. 2011; 18:175–180.
Article8. Boentert M, Wenninger S, Sansone VA. Respiratory involvement in neuromuscular disorders. Curr Opin Neurol. 2017; 30:529–537.
Article9. Polatli M, Akyol A, Cildag O, Bayülkem K. Pulmonary function tests in Parkinson’s disease. Eur J Neurol. 2001; 8:341–345.
Article10. Chiang J, Mehta K, Amin R. Respiratory diagnostic tools in neuromuscular disease. Children (Basel). 2018; 5:78.
Article11. DePalo VA, McCool FD. Respiratory muscle evaluation of the patient with neuromuscular disease. Semin Respir Crit Care Med. 2002; 23:201–209.
Article12. Crapo RO. Pulmonary-function testing. N Engl J Med. 1994; 331:25–30.
Article13. Lyall RA, Donaldson N, Polkey MI, Leigh PN, Moxham J. Respiratory muscle strength and ventilatory failure in amyotrophic lateral sclerosis. Brain. 2001; 124:2000–2013.
Article14. Morgan RK, McNally S, Alexander M, Conroy R, Hardiman O, Costello RW. Use of sniff nasal-inspiratory force to predict survival in amyotrophic lateral sclerosis. Am J Respir Crit Care Med. 2005; 171:269–274.
Article15. Davis MD, Walsh BK, Sittig SE, Restrepo RD. AARC clinical practice guideline: blood gas analysis and hemoximetry: 2013. Respir Care. 2013; 58:1694–1703.
Article16. Ak A, Ogun CO, Bayir A, Kayis SA, Koylu R. Prediction of arterial blood gas values from venous blood gas values in patients with acute exacerbation of chronic obstructive pulmonary disease. Tohoku J Exp Med. 2006; 210:285–290.
Article17. Herrington WG, Nye HJ, Hammersley MS, Watkinson PJ. Are arterial and venous samples clinically equivalent for the estimation of pH, serum bicarbonate and potassium concentration in critically ill patients? Diabet Med. 2012; 29:32–35.
Article18. Deane JC, Dagleish MP, Benamou AE, Wolf BT, Marlin D. Effects of syringe material and temperature and duration of storage on the stability of equine arterial blood gas variables. Vet Anaesth Analg. 2004; 31:250–257.
Article19. Fox MJ, Brody JS, Weintraub LR. Leukocyte larceny: a cause of spurious hypoxemia. Am J Med. 1979; 67:742–746.
Article20. Woolley A, Hickling K. Errors in measuring blood gases in the intensive care unit: effect of delay in estimation. J Crit Care. 2003; 18:31–37.
Article21. Folke M, Cernerud L, Ekström M, Hök B. Critical review of non-invasive respiratory monitoring in medical care. Med Biol Eng Comput. 2003; 41:377–383.
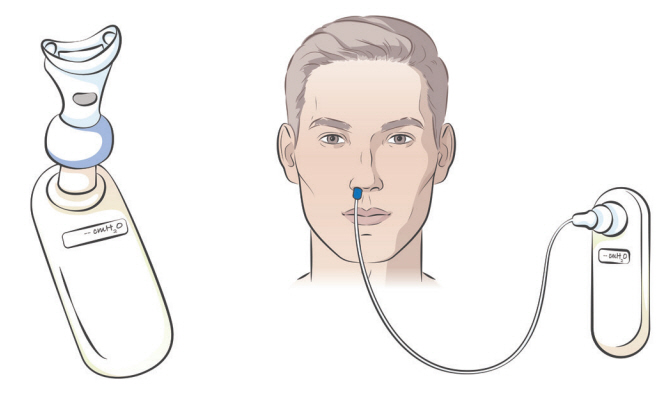
Article22. Friesen RH, Alswang M. End-tidal PCO2 monitoring via nasal cannulae in pediatric patients: accuracy and sources of error. J Clin Monit. 1996; 12:155–159.
Article23. Loughnan TE, Monagle J, Copland JM, Ranjan P, Chen MF. A comparison of carbon dioxide monitoring and oxygenation between facemask and divided nasal cannula. Anaesth Intensive Care. 2000; 28:151–154.
Article24. Linko K, Paloheimo M. Monitoring of the inspired and end-tidal oxygen, carbon dioxide, and nitrous oxide concentrations: clinical applications during anesthesia and recovery. J Clin Monit. 1989; 5:149–156.
Article25. Kavanagh BP, Sandler AN, Turner KE, Wick V, Lawson S. Use of end-tidal PCO2 and transcutaneous PCO2 as noninvasive measurement of arterial PCO2 in extubated patients recovering from general anesthesia. J Clin Monit. 1992; 8:226–230.
Article26. Santos LJ, Varon J, Pic-Aluas L, Combs AH. Practical uses of end-tidal carbon dioxide monitoring in the emergency department. J Emerg Med. 1994; 12:633–644.
Article27. Bach JR, Saporito LR. Criteria for extubation and tracheostomy tube removal for patients with ventilatory failure. A different approach to weaning. Chest. 1996; 110:1566–1571.
Article28. Evans JA, Whitelaw WA. The assessment of maximal respiratory mouth pressures in adults. Respir Care. 2009; 54:1348–1359.29. De Troyer A, Borenstein S, Cordier R. Analysis of lung volume restriction in patients with respiratory muscle weakness. Thorax. 1980; 35:603–610.
Article30. Tully K, Koke K, Garshick E, Lieberman SL, Tun CG, Brown R. Maximal expiratory pressures in spinal cord injury using two mouthpieces. Chest. 1997; 112:113–116.
Article31. Arora NS, Rochester DF. Respiratory muscle strength and maximal voluntary ventilation in undernourished patients. Am Rev Respir Dis. 1982; 126:5–8.32. Stefanutti D, Benoist MR, Scheinmann P, Chaussain M, Fitting JW. Usefulness of sniff nasal pressure in patients with neuromuscular or skeletal disorders. Am J Respir Crit Care Med. 2000; 162:1507–1511.
Article33. Mier-Jedrzejowicz A, Brophy C, Moxham J, Green M. Assessment of diaphragm weakness. Am Rev Respir Dis. 1988; 137:877–883.
Article34. Koulouris N, Mulvey DA, Laroche CM, Sawicka EH, Green M, Moxham J. The measurement of inspiratory muscle strength by sniff esophageal, nasopharyngeal, and mouth pressures. Am Rev Respir Dis. 1989; 139:641–646.
Article35. Laroche CM, Mier AK, Moxham J, Green M. The value of sniff esophageal pressures in the assessment of global inspiratory muscle strength. Am Rev Respir Dis. 1988; 138:598–603.
Article36. Miller JM, Moxham J, Green M. The maximal sniff in the assessment of diaphragm function in man. Clin Sci (Lond). 1985; 69:91–96.
Article37. Mier A, Brophy C, Moxham J, Green M. Twitch pressures in the assessment of diaphragm weakness. Thorax. 1989; 44:990–996.
Article38. Polkey MI, Duguet A, Luo Y, Hughes PD, Hart N, Hamnegård CH, et al. Anterior magnetic phrenic nerve stimulation: laboratory and clinical evaluation. Intensive Care Med. 2000; 26:1065–1075.
Article39. De Carvalho M. Electrodiagnostic assessment of respiratory dysfunction in motor neuron disease. Handbook of Clinical Neurophysiology. 2004; 4:513–528.40. Preston DC, Shapiro BE. Electromyography and neuromuscular disorders e-book: clinical-electrophysiologic-ultrasound correlations. 4th ed. Philadelphia: Elsevier Health Sciences;2020. p. 713–728.41. Gottesman E, McCool FD. Ultrasound evaluation of the paralyzed diaphragm. Am J Respir Crit Care Med. 1997; 155:1570–1574.
Article42. Wang Y, Shao WB, Gao L, Lu J, Gu H, Sun LH, et al. Abnormal pulmonary function and respiratory muscle strength findings in Chinese patients with Parkinson’s disease and multiple system atrophy--comparison with normal elderly. PLoS One. 2014; 9:e116123.
Article43. Howard RS, Rudd AG, Wolfe CD, Williams AJ. Pathophysiological and clinical aspects of breathing after stroke. Postgrad Med J. 2001; 77:700–702.
Article44. Houston JG, Morris AD, Grosset DG, Lees KR, McMillan N, Bone I. Ultrasonic evaluation of movement of the diaphragm after acute cerebral infarction. J Neurol Neurosurg Psychiatry. 1995; 58:738–741.
Article45. Cohen E, Mier A, Heywood P, Murphy K, Boultbee J, Guz A. Diaphragmatic movement in hemiplegic patients measured by ultrasonography. Thorax. 1994; 49:890–895.
Article46. Zimmer MB, Nantwi K, Goshgarian HG. Effect of spinal cord injury on the respiratory system: basic research and current clinical treatment options. J Spinal Cord Med. 2007; 30:319–330.
Article47. Hughes RA, Bihari D. Acute neuromuscular respiratory paralysis. J Neurol Neurosurg Psychiatry. 1993; 56:334–343.
Article48. Laroche CM, Mier AK, Spiro SG, Newsom-Davis J, Moxham J, Green M. Respiratory muscle weakness in the Lambert-Eaton myasthenic syndrome. Thorax. 1989; 44:913–918.
Article49. Wilcox P, Andolfatto G, Fairbarn MS, Pardy RL. Long-term follow-up of symptoms, pulmonary function, respiratory muscle strength, and exercise performance after botulism. Am Rev Respir Dis. 1989; 139:157–163.
Article50. Tsao TC, Juang YC, Lan RS, Shieh WB, Lee CH. Respiratory failure of acute organophosphate and carbamate poisoning. Chest. 1990; 98:631–636.
Article51. Howard RS, Wiles CM, Hirsch NP, Spencer GT. Respiratory involvement in primary muscle disorders: assessment and management. Q J Med. 1993; 86:175–189.52. Shahrizaila N, Kinnear WJ, Wills AJ. Respiratory involvement in inherited primary muscle conditions. J Neurol Neurosurg Psychiatry. 2006; 77:1108–1115.
Article53. Rimmer KP, Golar SD, Lee MA, Whitelaw WA. Myotonia of the respiratory muscles in myotonic dystrophy. Am Rev Respir Dis. 1993; 148:1018–1022.
Article54. Howard RS, Russell S, Losseff N, Harding AE, Hughes JM, Wiles CM, et al. Management of mitochondrial disease on an intensive care unit. QJM. 1995; 88:197–207.55. Braun NM, Arora NS, Rochester DF. Respiratory muscle and pulmonary function in polymyositis and other proximal myopathies. Thorax. 1983; 38:616–623.
Article56. Niedermeyer S, Murn M, Choi PJ. Respiratory failure in amyotrophic lateral sclerosis. Chest. 2019; 155:401–408.
Article57. Atsuta N, Watanabe H, Ito M, Banno H, Suzuki K, Katsuno M, et al. Natural history of spinal and bulbar muscular atrophy (SBMA): a study of 223 Japanese patients. Brain. 2006; 129:1446–1455.
Article58. Wijngaarde CA, Veldhoen ES, van Eijk RPA, Stam M, Otto LAM, Asselman FL, et al. Natural history of lung function in spinal muscular atrophy. Orphanet J Rare Dis. 2020; 15:88.
Article59. Finkel RS, Mercuri E, Meyer OH, Simonds AK, Schroth MK, Graham RJ, et al. Diagnosis and management of spinal muscular atrophy: part 2: pulmonary and acute care; medications, supplements and immunizations; other organ systems; and ethics. Neuromuscul Disord. 2018; 28:197–207.
Article60. Tzelepis GE, McCool FD. Respiratory dysfunction in multiple sclerosis. Respir Med. 2015; 109:671–679.
Article61. Askenasy JJ, Goldhammer I. Sleep apnea as a feature of bulbar stroke. Stroke. 1988; 19:637–639.
Article62. Devereaux MW, Keane JR, Davis RL. Automatic respiratory failure associated with infarction of the medulla. Report of two cases with pathologic study of one. Arch Neurol. 1973; 29:46–52.63. Andersen PM, Abrahams S, Borasio GD, de Carvalho M, Chio A, Van Damme P, et al. EFNS guidelines on the clinical management of amyotrophic lateral sclerosis (MALS)--revised report of an EFNS task force. Eur J Neurol. 2012; 19:360–375.64. Shoesmith C, Abrahao A, Benstead T, Chum M, Dupre N, Izenberg A, et al. Canadian best practice recommendations for the management of amyotrophic lateral sclerosis. CMAJ. 2020; 192:E1453–E1468.
Article65. Leonhard SE, Mandarakas MR, Gondim FAA, Bateman K, Ferreira MLB, Cornblath DR, et al. Diagnosis and management of Guillain-Barré syndrome in ten steps. Nat Rev Neurol. 2019; 15:671–683.
Article66. Kishnani PS, Steiner RD, Bali D, Berger K, Byrne BJ, Case LE, et al. Pompe disease diagnosis and management guideline. Genet Med. 2006; 8:267–288.
Article67. Schmidt EP, Drachman DB, Wiener CM, Clawson L, Kimball R, Lechtzin N. Pulmonary predictors of survival in amyotrophic lateral sclerosis: use in clinical trial design. Muscle Nerve. 2006; 33:127–132.
Article68. Gay PC, Westbrook PR, Daube JR, Litchy WJ, Windebank AJ, Iverson R. Effects of alterations in pulmonary function and sleep variables on survival in patients with amyotrophic lateral sclerosis. Mayo Clin Proc. 1991; 66:686–694.
Article69. Miller RG, Jackson CE, Kasarskis EJ, England JD, Forshew D, Johnston W, et al. Practice parameter update: the care of the patient with amyotrophic lateral sclerosis: drug, nutritional, and respiratory therapies (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2009; 73:1218–1226.
Article70. Finder JD, Birnkrant D, Carl J, Farber HJ, Gozal D, Iannaccone ST, et al. Respiratory care of the patient with Duchenne muscular dystrophy: ATS consensus statement. Am J Respir Crit Care Med. 2004; 170:456–465.71. Fromageot C, Lofaso F, Annane D, Falaize L, Lejaille M, Clair B, et al. Supine fall in lung volumes in the assessment of diaphragmatic weakness in neuromuscular disorders. Arch Phys Med Rehabil. 2001; 82:123–128.
Article72. Andrews JA, Meng L, Kulke SF, Rudnicki SA, Wolff AA, Bozik ME, et al. Association between decline in slow vital capacity and respiratory insufficiency, use of assisted ventilation, tracheostomy, or death in patients with amyotrophic lateral sclerosis. JAMA Neurol. 2018; 75:58–64.
Article73. Huang X, Du C, Yang Q, Fan D. Comparison of slow and forced vital capacity on ability to evaluate respiratory function in bulbar-involved amyotrophic lateral sclerosis. Front Neurol. 2022; 13:938256.
Article74. Lawn ND, Fletcher DD, Henderson RD, Wolter TD, Wijdicks EF. Anticipating mechanical ventilation in Guillain-Barré syndrome. Arch Neurol. 2001; 58:893–898.
Article75. Tzanis G, Vasileiadis I, Zervakis D, Karatzanos E, Dimopoulos S, Pitsolis T, et al. Maximum inspiratory pressure, a surrogate parameter for the assessment of ICU-acquired weakness. BMC Anesthesiol. 2011; 11:14.
Article76. Karthika M, Al Enezi FA, Pillai LV, Arabi YM. Rapid shallow breathing index. Ann Thorac Med. 2016; 11:167–176.
Article77. Lin SJ, Jerng JS, Kuo YW, Wu CL, Ku SC, Wu HD. Maximal expiratory pressure is associated with reinstitution of mechanical ventilation after successful unassisted breathing trials in tracheostomized patients with prolonged mechanical ventilation. PLoS One. 2020; 15:e0229935.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Study on Spirometry Pattern of Normal Children
- Lung function tests in preschool children
- Understanding and application of liver function tests
- Value of pulmonary function test as a predicting factor of pneumothorax in CT-guided needle aspiration of the lung
- Assessment of the relationship between pulmonary function test and dyspnea index in patients with bronchial asthma